4例不同类型胆管损伤型药物性肝损伤的临床病理特点分析
DOI: 10.3969/j.issn.1001-5256.2023.07.021
Clinical and pathological features of drug-induced liver injury with different types of bile duct injury: An analysis of four cases
-
摘要:
目的 对比观察不同类型胆管损伤型药物性肝损伤(DILI)患者的临床、生化、病理、病程及预后特点。 方法 选取石家庄市第五医院2015年3月-2020年10月经肝穿刺组织病理明确诊断为胆管损伤型DILI 4例患者。收集患者的临床资料、历次实验室检查、影像学检查及预后情况, 并对肝脏病理形态进行半定量评分, 对比分析4例患者各指标之间的差异。 结果 胆管损伤型DILI女性患者多见, 多数预后较好。胆管损伤的部位、级别、范围及再生修复不同, 其相应的临床症状、肝生化指标及预后亦不同。 结论 肝穿刺组织病理仍然是胆管损伤型DILI明确诊断、了解病变损伤情况及判断预后的金标准。 -
关键词:
- 化学性与药物性肝损伤 /
- 胆汁淤积 /
- 病理状态, 体征和症状
Abstract:Objective To investigate the clinical, biochemical, pathological, disease course, and prognostic features of drug-induced liver injury (DILI) patients with different types of bile duct injury. Methods Four patients who were diagnosed with bile duct injury-type DILI by liver biopsy in Shijiazhuang Fifth Hospital, from March 2015 to October 2010 were selected, and related data were collected, including clinical data, laboratory examinations, radiological examination, and prognosis.The semi-quantitative score was determined for liver pathological morphology, and each indicator was compared between the four patients. Results Bile duct injury-type DILI was more common in female patients, and most patients tended to have a good prognosis.Clinical symptoms, liver biochemical parameters, and prognosis varied with the site, grade, scope, regeneration, and repair of bile duct injury. Conclusion Liver biopsy is still the gold standard for making a definite diagnosis of bile duct injury-type DILI, understanding the condition of lesions, and judging the prognosis of this disease. -
表 1 患者一般情况
Table 1. General data of patients
病例 性别 年龄
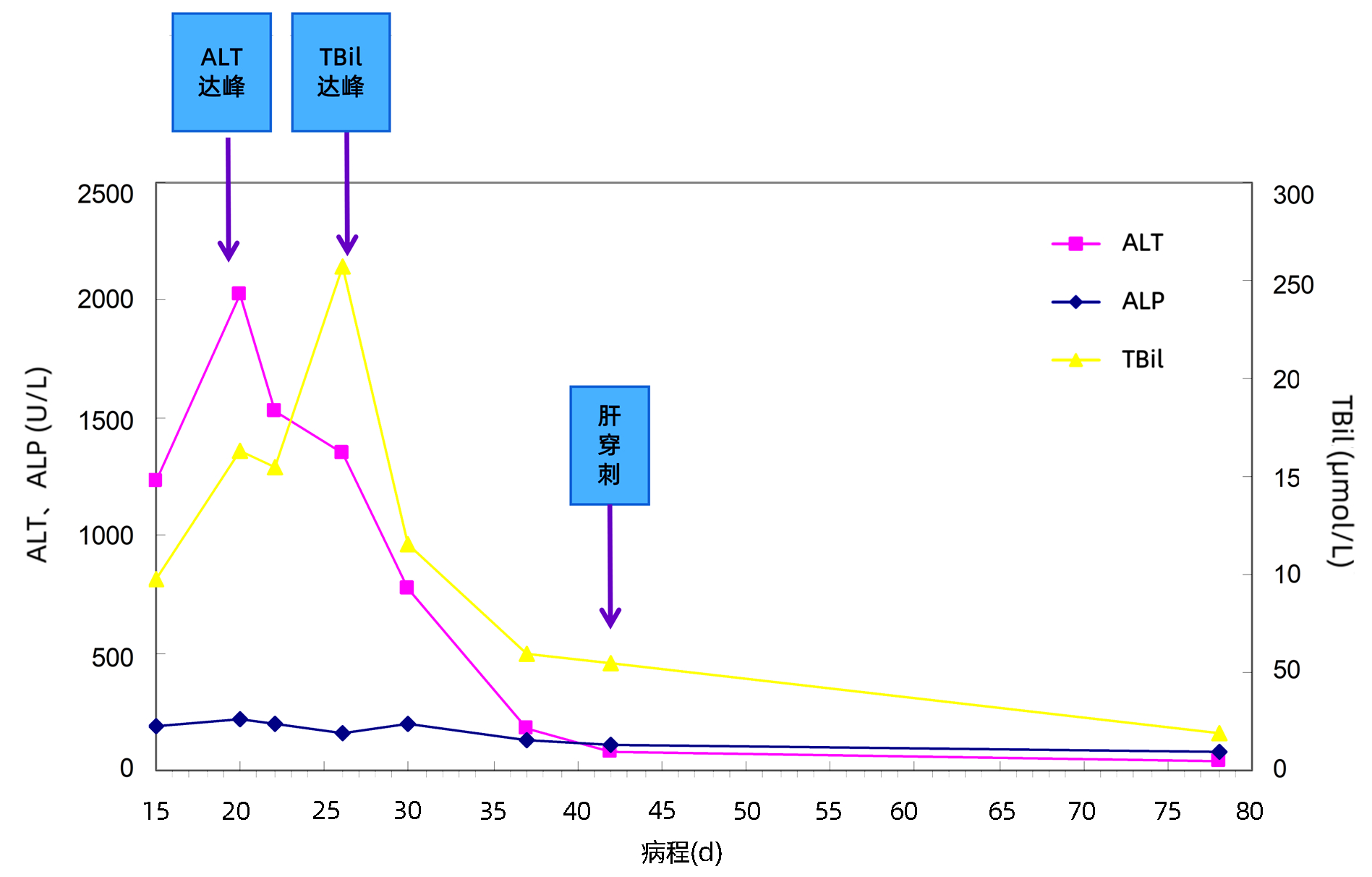
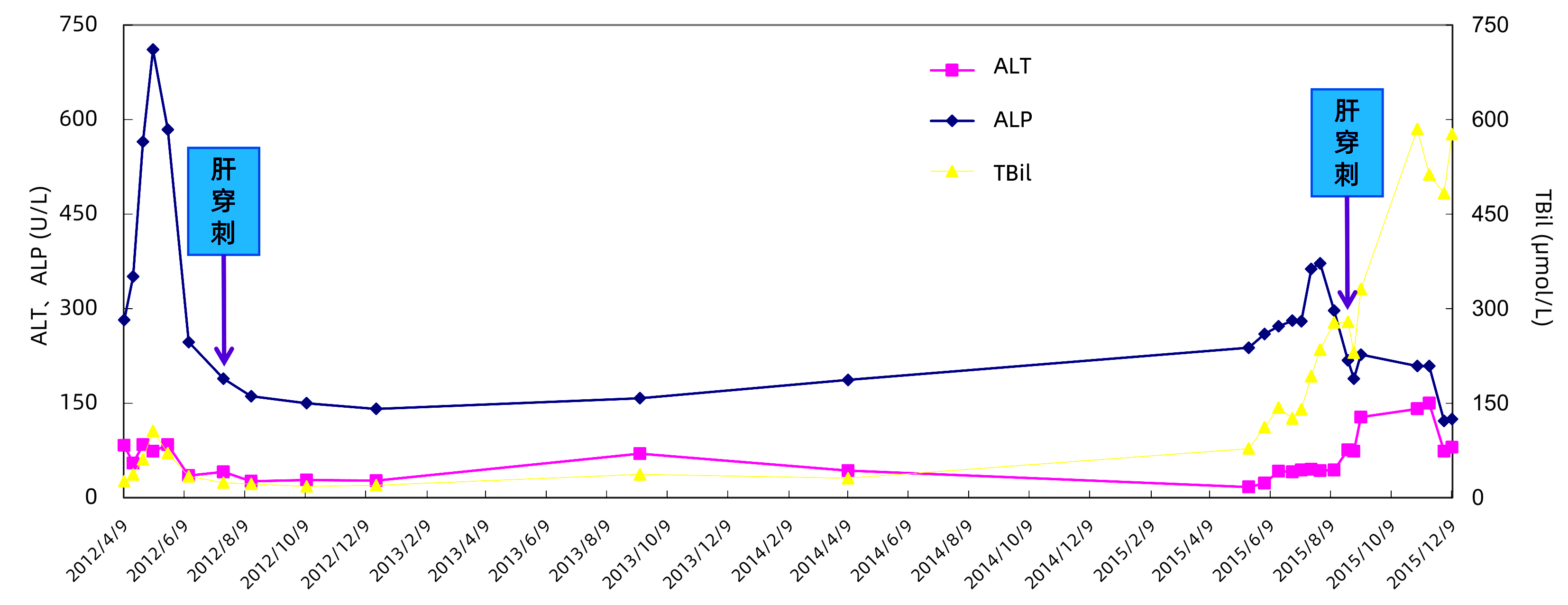
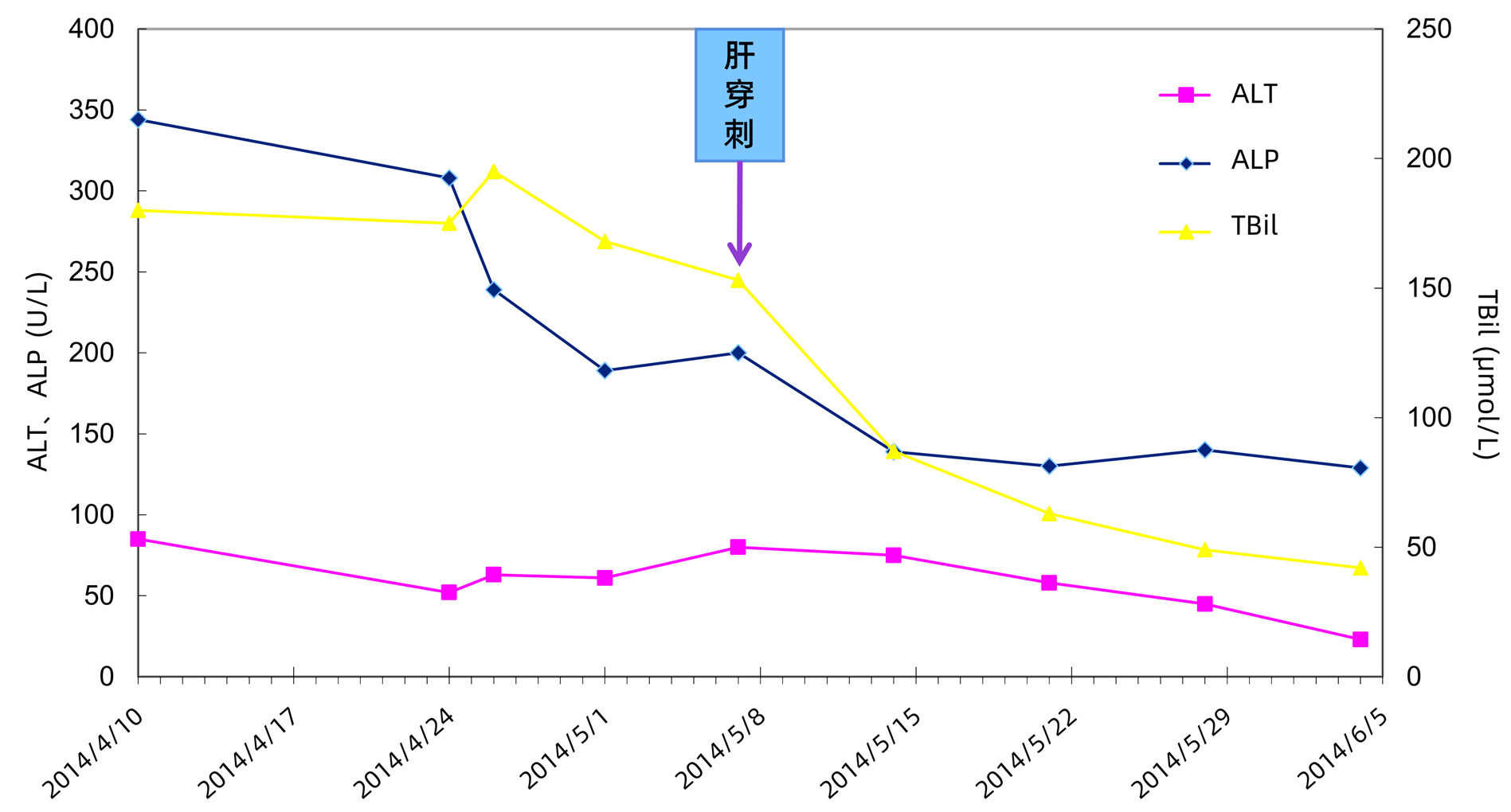
(岁)既往史 用药史 病理诊断 病程 预后 1 女 59 无 因关节痛口服10付中药(含红花,土鳖等) 单纯胆汁淤积 2.5个月肝功能恢复 好 2 女 70 无 服“生发”中药(均含何首乌)治疗4个月 淤胆性肝炎 3个月肝功能恢复 好 3 女 23 无 因面部座疮口服“土霉素片”2个月 急性VBDS 1年肝功能基本恢复 较好 4 男 47 饮酒史20年 反复服用“阿莫西林” 3年 胆汁性肝硬化 3年7个月进展为肝衰竭 差 注:VBDS,胆管消失综合征。 表 2 患者临床症状及体征情况
Table 2. Clinical symptoms and signs of patients
症状 单纯淤胆
(病例1)淤胆性肝炎
(病例2)急性VBDS
(病例3)胆汁性肝硬化
(病例4)乏力 - + - + 食欲不振 - + - + 呕吐 - - - - 恶心 - - - - 发热 - 一过性 - - 瘙痒 ++ ++ - ++ 皮肤巩膜黄染 ++ ++ + +++ 厌油腻 - + - + 茶色尿 + + - + 大便发白 + - - - 蜘蛛痣/肝掌 - - - -/+ 腹痛/腹泻 - - - -/+ 呕血/黑便 - - - - 食管胃底静脉曲张 - - - + 肝大 - 肋下2 cm + 剑突下8 cm 脾大 - 肋下7 cm + 巨脾 皮疹 - - - 偶有 注:+ 轻度;++ 中度;+++ 重度。 表 3 患者肝生化指标高峰值及自身抗体情况
Table 3. The peak value of liver biochemical indexes and autoantibodies of patients
病例 ALT
(U/L)AST
(U/L)ALP
(U/L)GGT
(U/L)TBil
(μmol/L)DBil
(μmol/L)Alb
(g/L)GLB
(g/L)TBA
(μmol/L)ChE
(U/L)TC
(U/L)TG
(U/L)自身抗体 1 88 83 344 114 195 151 39 34 231 4 297 6.8 / - 2 1 427 1 506 295 196 266 193 28 53 129 3 916 7.5 3.4 ANA 1∶640 3 356 258 745 826 54 38 35 46 135 3 824 10.9 2.9 - 4 150 193 711 514 585 447 26 33 389 1 189 4.7 1.6 - 注:肝功能各项指标均为病程中最高值(Alb为最低值)。GLB,球蛋白;ChE,胆碱酯酶;ANA,抗核抗体。/,未检测,-,阴性。 表 4 患者影像学及病理检查
Table 4. Imaging and pathological examination of the patient
病例 胆囊壁厚
(mm)脾长/厚
(cm)肝最大斜径
(cm)损伤靶点 病理描述 1 2 10.7/2.4 10.8 单纯毛细胆管损伤DILI临床分类淤胆型 肝小叶2带、3带肝细胞胆汁淤积及毛细胆管胆栓形成,吞噬细胞吞噬毛细胆管胆栓致肝窦轻度扩张,肝板排列较规整。汇管区内无明显炎症浸润。病理诊断:单纯性胆汁淤积 2 6 6.7/3.6 13.6 毛细胆管+肝细胞损伤DILI临床分类混合型 中央静脉周围可见融合性坏死,并见羽毛样变性及毛细胆管胆栓,坏死带内肝细胞脱失、网架塌陷,周围肝板呈双排(提示肝细胞再生);汇管区内中度混合性炎细胞浸润。汇管区周边少数细胆管增生,部分小胆管上皮排列不整。病理诊断:淤胆性肝炎,早期再生修复 3 3 12.5/4.1 11.8 小叶间胆管损伤(VBDS) 汇管区间质内轻度单个核细胞浸润,并见蜡质样细胞沉积,其中5个汇管区均未见小叶间胆管;小叶内局部肝板断离及肝窦扩张,周围可见增宽的肝板(提示肝细胞再生)。病理诊断:VBDS 4 4 18.4/5.6 12.4 小叶间胆管及隔胆管以上较大胆管损伤(VBDS +胆汁性肝硬化) 第一次肝穿刺: 肝实质被纤维化扩大的汇管区及纤维间隔分隔成七巧板样结节,大部汇管区内未见小动脉伴行小胆管,可见较多增生细胆管,周边带肝细胞部分肿大呈胆盐淤积,毛细胆管内见粗大胆栓。病理诊断:胆汁性肝硬化
第二次肝穿刺: 汇管区纤维化扩大程度较第一次肝穿刺加重,肝实质被破坏,仅见小团肝细胞残留。扩大汇管区及间隔内中度单个核细胞浸润,周边带细胆管增生较明显。被分隔肝实质内毛细胆管胆栓较第一次肝穿刺明显增多。病理诊断:胆汁性肝硬化,肝内慢性淤胆,药物性胆管损伤(VBDS)可能性大表 5 患者病理形态学特点及评分情况
Table 5. Pathological morphological characteristics and scores of patients
项目 单纯淤胆
(病例1)淤胆性肝炎
(病例2)急性VBDS
(病例3)胆汁性肝硬化
(病例4)发病-肝穿刺时间 28天 42天 60天 3年5个月 肝穿刺长(cm)/汇管区(个) 1.0/7 1.2/10 1.2/6 1.3 坏死(分) 0 2 2 1 凋亡(分) 0 1 0 0 羽毛样变性(分) 1 2 0 1 毛细胆管胆栓(分) 2 1 0 3 胆色素(分) 2 2 0 0 吞噬细胞(分) 2 2 0 0 肝细胞再生(分) 0 3 2 0 汇管区扩大(分) 0 2 1 4 汇管区炎症(分) 1 3 1 2 炎细胞成分 单个核细胞 混合性炎细胞EOS+、P++ 单个核细胞 混合性炎细胞 界面炎(分) 0 2 1 3 边缘胆管 轻度扩张、增生 轻度扩张、增生 无 中度扩张、增生 细胆管增生Ⅱ型(分) 0 1 0 3 纤维化分期 0 1 0 4 小叶间胆管损伤特点 胆管上皮变性、排列不整 胆管上皮空泡变、嗜酸性变性,排列不整 5/7汇管区缺乏小叶间胆管; 另2个汇管区内小叶间胆管变性、排列不整 汇管区内绝大部分小叶间胆管消失 注:EOS,嗜酸性粒细胞;P,浆细胞;各形态评分参照王泰龄教授DILI评分标准[5]。 -
[1] LAI RT, YU YC, CHEN CW. Review and clinical concerns of drug-induced liver injury in 2021[J]. Chin Hepatol, 2022, 27(1): 1-3. DOI: 10.3969/j.issn.1008-1704.2022.01.001.赖荣陶, 于乐成, 陈成伟. 2021药物性肝损伤研究回顾和临床关注的问题[J]. 肝脏, 2022, 27(1): 1-3. DOI: 10.3969/j.issn.1008-1704.2022.01.001. [2] KLEINER DE, CHALASANI NP, LEE WM, et al. Hepatic histological findings in suspected drug-induced liver injury: Systematic evaluation and clinical associations[J]. Hepatology, 2014, 59(2): 661-670. DOI: 10.1002/hep.26709. [3] LEWIS JH, KLEINER DE. Hepatic injury due to drugs, herbal compounds, chemicals and toxins[M]// MacSween's Pathology of the Liver, 6th ed. Edinburgh: Churchill Livingstone, 2014: 654-655. [4] Drug-induced Liver Disease Study Group, Chinese Society of Hepatology, Chinese Medical Association. Guidelines for the management of drug-induced liver injury[J]. J Clin Hepatol, 2015, 31(11): 1752-1769. DOI: 10.3969/j.issn.1001-5256.2015.11.002.中华医学会肝病学分会药物性肝病学组. 药物性肝损伤诊治指南[J]. 临床肝胆病杂志, 2015, 31(11): 1752-1769. DOI: 10.3969/j.issn.1001-5256.2015.11.002. [5] Drug-induced Liver Disease Study Group, Chinese Society of Hepatology, Chinese Medical Association. Interpretation of CSH clinical guideline: The diagnosis and management of drug-induced liver injury[M]. Shanghai: Shanghai Scientific & Technical Publishers, 2015.中华医学会肝脏病学分会药物性肝病学组. 药物性肝损伤诊治指南解读[M]. 上海: 上海科学技术出版社, 2015. [6] VUPPALANCHI R, CHALASANI N, SAXENA R. Restoration of bile ducts in drug-induced vanishing bile duct syndrome due to zonisamide[J]. Am J Surg Pathol, 2006, 30(12): 1619-1623. DOI: 10.1097/01.pas.0000213342.78475.48. [7] YANG Y, GE FL, HUANG Q, et al. Risk factors for herb-induced liver injury[J]. J Clin Hepatol, 2022, 38(5): 1183-1187. DOI: 10.3969/j.issn.1001-5256.2022.05.044.杨燕, 葛斐林, 黄倩, 等. 中药相关肝损伤的风险因素[J]. 临床肝胆病杂志, 2022, 38(5): 1183-1187. DOI: 10.3969/j.issn.1001-5256.2022.05.044. [8] WANG HZ, LI XH. Research advances in the pathogenesis of drug-induced liver injury[J]. J Clin Hepatol, 2018, 34(4): 883-887. DOI: 10.3969/j.issn.1001-5256.2018.04.040.王海珍, 李秀惠. 药物性肝损伤发病机制研究进展[J]. 临床肝胆病杂志, 2018, 34(4): 883-887. DOI: 10.3969/j.issn.1001-5256.2018.04.040. [9] WANG TL, ZHAO XY, SHAO C, et al. A proposed pathologic sub-classification of drug-induced liver injury[J]. Hepatol Int, 2019, 13(3): 339-351. DOI: 10.1007/s12072-019-09940-9. [10] WASUWANICH P, CHOUDRY H, SO JM, et al. Vanishing bile duct syndrome after drug-induced liver injury[J]. Clin Res Hepatol Gastroenterol, 2022, 46(9): 102015. DOI: 10.1016/j.clinre.2022.102015. [11] BELL LN, CHALASANI N. Epidemiology of idiosyncratic drug-induced liver injury[J]. Semin Liver Dis, 2009, 29(4): 337-347. DOI: 10.1055/s-0029-1240002. [12] MEDINA-CALIZ I, ROBLES-DIAZ M, GARCIA-MUÑOZ B, et al. Definition and risk factors for chronicity following acute idiosyncratic drug-induced liver injury[J]. J Hepatol, 2016, 65(3): 532-542. DOI: 10.1016/j.jhep.2016.05.003. [13] de VRIES E, BEUERS U. Management of cholestatic disease in 2017[J]. Liver Int, 2017, 37(Suppl 1): 123-129. DOI: 10.1111/liv.13306. [14] WU WX, WANG T, GENG XC, et al. Progress in study of drug-induced cholestasis liver injury[J]. Chin J New Drugs, 2020, 29(2): 143-151. DOI: 10.3969/j.issn.1003-3734.2020.02.005.吴文晓, 王婷, 耿兴超, 等. 药物性胆汁淤积型肝损伤的研究进展[J]. 中国新药杂志, 2020, 29(2): 143-151. DOI: 10.3969/j.issn.1003-3734.2020.02.005. [15] MANCO R, CLERBAUX LA, VERHULST S, et al. Reactive cholangiocytes differentiate into proliferative hepatocytes with efficient DNA repair in mice with chronic liver injury[J]. J Hepatol, 2019, 70(6): 1180-1191. DOI: 10.1016/j.jhep.2019.02.003. [16] ZHU ZW, HUANG HL. Research progress on physiological characteristics of bile duct epithelial cells and their correlation with liver diseases[J]. J Hepatopancreatobiliary Surg, 2022, 34(3): 187-192. DOI: 10.11952/j.issn.1007-1954.2022.03.013.朱志文, 黄海丽. 胆管上皮细胞的生理学特点及其与肝脏疾病相关性的研究进展[J]. 肝胆胰外科杂志, 2022, 34(3): 187-192. DOI: 10.11952/j.issn.1007-1954.2022.03.013. [17] CHEUNG AC, LORENZO PISARELLO MJ, LARUSSO NF. Pathobiology of biliary epithelia[J]. Biochim Biophys Acta BBA Mol Basis Dis, 2018, 1864(4): 1220-1231. DOI: 10.1016/j.bbadis.2017.06.024. [18] RAVEN A, LU WY, MAN TY, et al. Cholangiocytes act as facultative liver stem cells during impaired hepatocyte regeneration[J]. Nature, 2017, 547(7663): 350-354. DOI: 10.1038/nature23015. [19] CHALASANI NP, HAYASHI PH, BONKOVSKY HL, et al. ACG Clinical Guideline: The diagnosis and management of idiosyncratic drug-induced liver injury[J]. Am J Gastroenterol, 2014, 109(7): 950-966; quiz967. DOI: 10.1038/ajg.2014.131. -



 PDF下载 ( 2634 KB)
PDF下载 ( 2634 KB)

 下载:
下载: