脑乳酸水平与肝性脑病的关系
DOI: 10.3969/j.issn.1001-5256.2023.07.031
利益冲突声明:本文不存在任何利益冲突。
作者贡献声明:刘玉琴负责选题,收集分析资料,撰写文章;陈密、唐兰燕、周丽智、黄鑫参与收集资料,修改论文;张磐拟定写作方向和思路,指导文章撰写,提供修改意见并最终定稿。
-
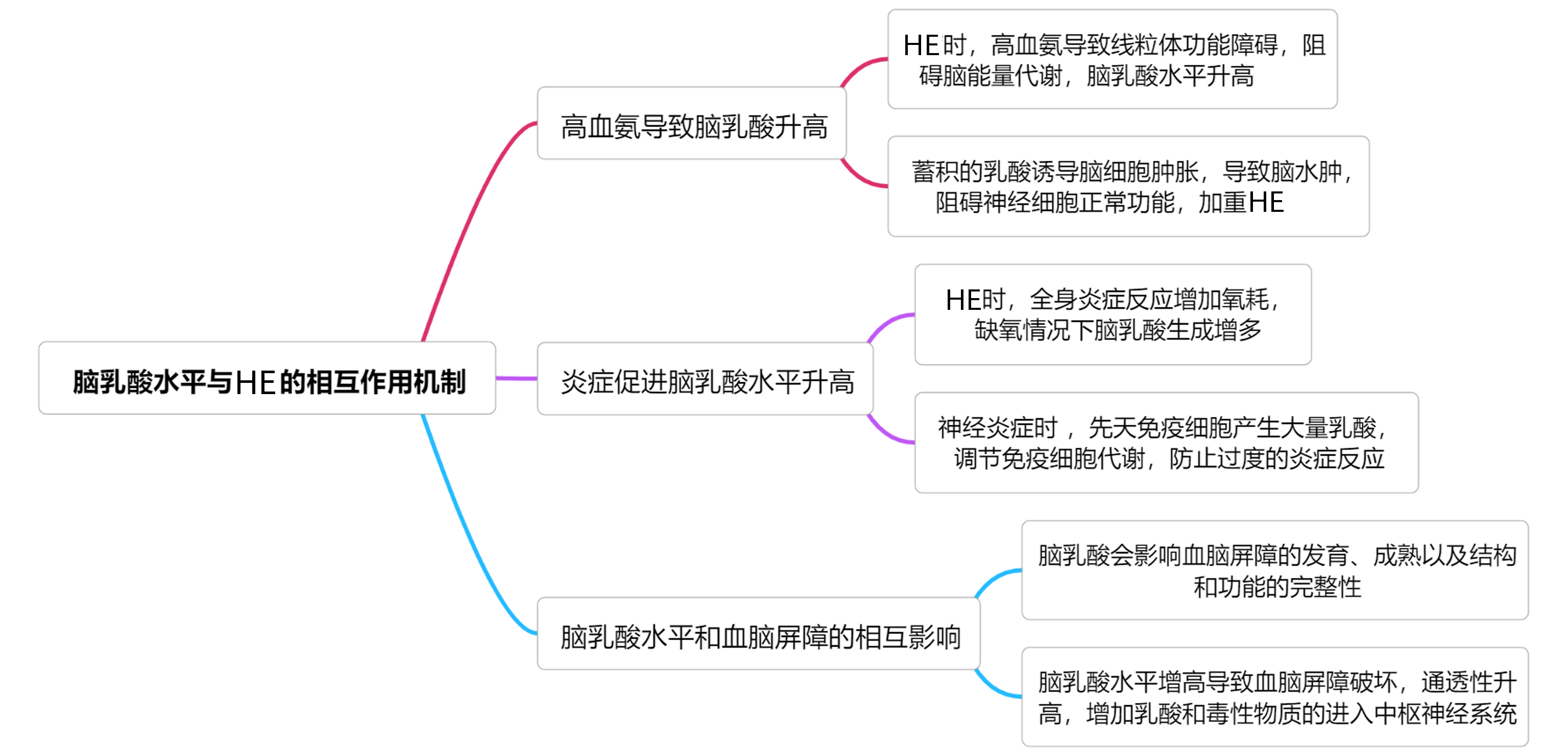
摘要: 肝性脑病(HE)是肝硬化患者常见的并发症,也是肝硬化患者死亡的独立危险因素。脑乳酸水平与HE的进展及严重程度相关,对于脑乳酸水平的研究有助于进一步解释HE的发病机制。本文通过总结脑乳酸代谢过程、脑乳酸水平与HE的关系、HE潜在治疗靶点,为临床医生进一步系统地评估HE患者的病情进展、治疗效果及预后情况提供一定的参考依据,旨在减轻患者医药负担,改善HE患者预后。Abstract: Hepatic encephalopathy (HE) is a common complication and an independent risk factor for death in patients with liver cirrhosis. Brain lactate level is associated with the progression and severity of HE, and research on brain lactate level may help to further explain the pathogenesis of HE. This article summarizes the metabolic process of brain lactate, the association between brain lactate level and HE, and the potential therapeutic targets for HE and provides a reference for clinicians to further systematically evaluate the progression, treatment outcome, and prognosis of patients with HE, in order to reduce the medical burden of patients and improve the prognosis of patients with HE.
-
Key words:
- Hepatic Encephalopathy /
- Lactic Acid /
- Blood-Brain Barrier /
- Brain Edema
-
[1] Chinese Society of Hepatology, Chinese Medical Association. Guidelines on the management of hepatic encephalopathy in cirrhosis[J]. J Clin Hepatol, 2018, 34(10): 2076-2089. DOI: 10.3969/j.issn.1001-5256.2018.10.007.中华医学会肝病学分会. 肝硬化肝性脑病诊疗指南[J]. 临床肝胆病杂志, 2018, 34(10): 2076-2089. DOI: 10.3969/j.issn.1001-5256.2018.10.007. [2] GUO JS. Epidemiology, diagnosis and treatment of minimal hepatic encephalopathy[J]. Chin J Hepatol, 2014, 22(2): 92-93. DOI: 10.3760/cma.j.issn.1007-3418.2014.02.005.郭津生. 重视轻微型肝性脑病的流行病学及诊断与治疗[J]. 中华肝脏病杂志, 2014, 22(2): 92-93. DOI: 10.3760/cma.j.issn.1007-3418.2014.02.005. [3] LIU SY, LI LH, LI SX, et al. Predictive value of controlled nutritional status score for overt hepatic encephalopathy after transjugular intrahepatic portosystemic stent-shunt of Budd-Chiari syndrome[J]. Chin J Dig Surg, 2023, 22(2): 251-259. DOI: 10.3760/cma.j.cn115610-20221205-00733.刘胜炎, 李路豪, 李素新, 等. 控制营养状况评分对布-加综合征患者行经颈静脉肝内门腔内支架分流术后发生显性肝性脑病的预测价值[J]. 中华消化外科杂志, 2023, 22(2): 251-259. DOI: 10.3760/cma.j.cn115610-20221205-00733. [4] JANSEN TC, van BOMMEL J, BAKKER J. Blood lactate monitoring in critically ill patients: a systematic health technology assessment[J]. Crit Care Med, 2009, 37(10): 2827-2839. DOI: 10.1097/CCM.0b013e3181a98899. [5] ROSE CF. Increase brain lactate in hepatic encephalopathy: cause or consequence?[J]. Neurochem Int, 2010, 57(4): 389-394. DOI: 10.1016/j.neuint.2010.06.012. [6] ANDERSEN LW, MACKENHAUER J, ROBERTS JC, et al. Etiology and therapeutic approach to elevated lactate levels[J]. Mayo Clin Proc, 2013, 88(10): 1127-1140. DOI: 10.1016/j.mayocp.2013.06.012. [7] LEVY B. Lactate and shock state: the metabolic view[J]. Curr Opin Crit Care, 2006, 12(4): 315-321. DOI: 10.1097/01.ccx.0000235208.77450.15. [8] JUEL C. Lactate-proton cotransport in skeletal muscle[J]. Physiol Rev, 1997, 77(2): 321-358. DOI: 10.1152/physrev.1997.77.2.321. [9] TANG F, LANE S, KORSAK A, et al. Lactate-mediated glia-neuronal signalling in the mammalian brain[J]. Nat Commun, 2014, 5: 3284. DOI: 10.1038/ncomms4284. [10] BASTIAN C, ZERIMECH S, NGUYEN H, et al. Aging astrocytes metabolically support aging axon function by proficiently regulating astrocyte-neuron lactate shuttle[J]. Exp Neurol, 2022, 357: 114173. DOI: 10.1016/j.expneurol.2022.114173. [11] VAN HALL G. Lactate kinetics in human tissues at rest and during exercise[J]. Acta Physiol (Oxf), 2010, 199(4): 499-508. DOI: 10.1111/j.1748-1716.2010.02122.x. [12] JHA MK, MORRISON BM. Lactate transporters mediate glia-neuron metabolic crosstalk in homeostasis and disease[J]. Front Cell Neurosci, 2020, 14: 589582. DOI: 10.3389/fncel.2020.589582. [13] BOSOI CR, ROSE CF. Identifying the direct effects of ammonia on the brain[J]. Metab Brain Dis, 2009, 24(1): 95-102. DOI: 10.1007/s11011-008-9112-7. [14] RAMA RAO KV, NORENBERG MD. Brain energy metabolism and mitochondrial dysfunction in acute and chronic hepatic encephalopathy[J]. Neurochem Int, 2012, 60(7): 697-706. DOI: 10.1016/j.neuint.2011.09.007. [15] KALA G, HERTZ L. Ammonia effects on pyruvate/lactate production in astrocytes-interaction with glutamate[J]. Neurochem Int, 2005, 47(1-2): 4-12. DOI: 10.1016/j.neuint.2005.04.001. [16] LERCHUNDI R, FERNÁNDEZ-MONCADA I, CONTRERAS-BAEZA Y, et al. NH4(+) triggers the release of astrocytic lactate via mitochondrial pyruvate shunting[J]. Proc Natl Acad Sci U S A, 2015, 112(35): 11090-11095. DOI: 10.1073/pnas.1508259112. [17] QIN ZW, LIU JT, FAN XH, et al. Relationship between intestinal flora and hepatic encephalopathy[J]. Chin J Gastroenter Hepatol, 2021, 30(1): 34-37. DOI: 10.3969/j.issn.1006-5709.2021.01.008.秦子文, 刘晶涛, 范晓红, 等. 肠道菌群与肝性脑病的关系[J]. 胃肠病学和肝病学杂志, 2021, 30(1): 34-37. DOI: 10.3969/j.issn.1006-5709.2021.01.008. [18] BEARD E, LENGACHER S, DIAS S, et al. Astrocytes as key regulators of brain energy metabolism: New therapeutic perspectives[J]. Front Physiol, 2021, 12: 825816. DOI: 10.3389/fphys.2021.825816. [19] LOMNETH R, MEDRANO S, GRUENSTEIN EI. The role of transmembrane pH gradients in the lactic acid induced swelling of astrocytes[J]. Brain Res, 1990, 523(1): 69-77. DOI: 10.1016/0006-8993(90)91636-u. [20] ANDERSSON AK, ADERMARK L, PERSSON M, et al. Lactate contributes to ammonia-mediated astroglial dysfunction during hyperammonemia[J]. Neurochem Res, 2009, 34(3): 556-565. DOI: 10.1007/s11064-008-9819-1. [21] LIU PF, BAO J. Changes of intestinal flora and serum inflammatory factor levels of patients with subclinical hepatic encephalopathy and the intervention effect of probiotics[J]. Chin J Microecol, 2020, 32(2): 180-182, 6. DOI: 10.13381/j.cnki.cjm.202002012.柳萍飞, 包健. 亚临床肝性脑病患者肠道菌群和血清炎症因子水平变化及益生菌的干预作用[J]. 中国微生态学杂志, 2020, 32(2): 180-182, 6. DOI: 10.13381/j.cnki.cjm.202002012. [22] XIE NW, LU J, HE JQ, et al. IL-6, IL-10, TNF in patients with HBV-ACLF hepatic encephalopathy- α Horizontal expression and significance[J]. Chongqing Med, 2017, 46(9): 1268-1271. DOI: 10.3969/j.issn.1671-8348.2017.09.038.谢能文, 炉军, 何金秋, 等. HBV-ACLF肝性脑病患者IL-6、IL-10、TNF-α水平表达及意义[J]. 重庆医学, 2017, 46(9): 1268-1271. DOI: 10.3969/j.issn.1671-8348.2017.09.038. [23] MANZHALII E, VIRCHENKO O, FALALYEYEVA T, et al. Hepatic Encephalopathy Aggravated by Systemic Inflammation[J]. Dig Dis, 2019, 37(6): 509-517. DOI: 10.1159/000500717. [24] ARROYO V, ANGELI P, MOREAU R, et al. The systemic inflammation hypothesis: Towards a new paradigm of acute decompensation and multiorgan failure in cirrhosis[J]. J Hepatol, 2021, 74(3): 670-685. DOI: 10.1016/j.jhep.2020.11.048. [25] HUANG X, HUSSAIN B, CHANG J. Peripheral inflammation and blood-brain barrier disruption: effects and mechanisms[J]. CNS Neurosci Ther, 2021, 27(1): 36-47. DOI: 10.1111/cns.13569. [26] AGUSTI A, HERNÁNDEZ-RABAZA V, BALZANO T, et al. Sildenafil reduces neuroinflammation in cerebellum, restores GABAergic tone, and improves motor in-coordination in rats with hepatic encephalopathy[J]. CNS Neurosci Ther, 2017, 23(5): 386-394. DOI: 10.1111/cns.12688. [27] RATTER JM, ROOIJACKERS H, HOOIVELD GJ, et al. In vitro and in vivo effects of lactate on metabolism and cytokine production of Human primary PBMCs and monocytes[J]. Front Immunol, 2018, 9: 2564. DOI: 10.3389/fimmu.2018.02564. [28] DALSGAARD MK, QUISTORFF B, DANIELSEN ER, et al. A reduced cerebral metabolic ratio in exercise reflects metabolism and not accumulation of lactate within the human brain[J]. J Physiol, 2004, 554(Pt 2): 571-578. DOI: 10.1113/jphysiol.2003.055053. [29] GERHART DZ, ENERSON BE, ZHDANKINA OY, et al. Expression of monocarboxylate transporter MCT1 by brain endothelium and glia in adult and suckling rats[J]. Am J Physiol, 1997, 273(1 Pt 1): E207-E213. DOI: 10.1152/ajpendo.1997.273.1.E207. [30] BERGERSEN LH. Lactate transport and signaling in the brain: potential therapeutic targets and roles in body-brain interaction[J]. J Cereb Blood Flow Metab, 2015, 35(2): 176-185. DOI: 10.1038/jcbfm.2014.206. [31] TOFTENG F, LARSEN FS. Monitoring extracellular concentrations of lactate, glutamate, and glycerol by in vivo microdialysis in the brain during liver transplantation in acute liver failure[J]. Liver Transpl, 2002, 8(3): 302-305. DOI: 10.1053/jlts.2002.32283. [32] SALMINA AB, KUVACHEVA NV, MORGUN AV, et al. Glycolysis-mediated control of blood-brain barrier development and function[J]. Int J Biochem Cell Biol, 2015, 64: 174-184. DOI: 10.1016/j.biocel.2015.04.005. [33] WANG J, CUI YX, YU ZX, et al. Brain endothelial cells maintain lactate homeostasis and control adult hippocampal neurogenesis[J]. Cell Stem Cell, 2019, 25(6): 754-767. DOI: 10.1016/j.stem.2019.09.009. [34] REX A, BERT B, FINK H, et al. Stimulus-dependent changes of extracellular glucose in the rat hippocampus determined by in vivo microdialysis[J]. Physiol Behav, 2009, 98(4): 467-473. DOI: 10.1016/j.physbeh.2009.07.015. [35] ERLICHMAN JS, HEWITT A, DAMON TL, et al. Inhibition of monocarboxylate transporter 2 in the retrotrapezoid nucleus in rats: a test of the astrocyte-neuron lactate- shuttle hypothesis[J]. J Neurosci, 2008, 28(19): 4888-4896. DOI: 10.1523/JNEUROSCI.5430-07.2008. [36] GORDON GR, CHOI HB, RUNGTA RL, et al. Brain metabolism dictates the polarity of astrocyte control over arterioles[J]. Nature, 2008, 456(7223): 745-749. DOI: 10.1038/nature07525. [37] OHBUCHI T, SATO K, SUZUKI H, et al. Acid-sensing ion channels in rat hypothalamic vasopressin neurons of the supraoptic nucleus[J]. J Physiol, 2010, 588(Pt 12): 2147-2162. DOI: 10.1113/jphysiol.2010.187625. [38] BERGERSEN LH, GJEDDE A. Is lactate a volume transmitter of metabolic states of the brain?[J]. Front Neuroenergetics, 2012, 4: 5. DOI: 10.3389/fnene.2012.00005. [39] YANG S, LIU K, YANG L, et al. Value of lactate level in predicting the short-term prognosis of patients with acute-on-chronic hepatitis B liver failure[J]. J Clin Hepatol, 2022, 38(7): 1482-1488. DOI: 10.3969/j.issn.1001-5256.2022.07.007.杨烁, 刘坤, 杨兰, 等. 乳酸水平对HBV相关慢加急性肝衰竭患者短期预后的预测价值[J]. 临床肝胆病杂志, 2022, 38(7): 1482-1488. DOI: 10.3969/j.issn.1001-5256.2022.07.007. [40] WALSH TS, MCLELLAN S, MACKENZIE SJ, et al. Hyperlactatemia and pulmonary lactate production in patients with fulminant hepatic failure[J]. Chest, 1999, 116(2): 471-476. DOI: 10.1378/chest.116.2.471. [41] ENGELMANN C, CLÀRIA J, SZABO G, et al. Pathophysiology of decompensated cirrhosis: Portal hypertension, circulatory dysfunction, inflammation, metabolism and mitochondrial dysfunction[J]. J Hepatol, 2021, 75(Suppl 1): S49-S66. DOI: 10.1016/j.jhep.2021.01.002. [42] CHATAURET N, ZWINGMANN C, ROSE C, et al. Effects of hypothermia on brain glucose metabolism in acute liver failure: a H/C-nuclear magnetic resonance study[J]. Gastroenterology, 2003, 125(3): 815-824. DOI: 10.1016/s0016-5085(03)01054-0. [43] BOSOI CR, ZWINGMANN C, MARIN H, et al. Increased brain lactate is central to the development of brain edema in rats with chronic liver disease[J]. J Hepatol, 2014, 60(3): 554-560. DOI: 10.1016/j.jhep.2013.10.011. [44] DIENEL GA. The metabolic trinity, glucose-glycogen-lactate, links astrocytes and neurons in brain energetics, signaling, memory, and gene expression[J]. Neurosci Lett, 2017, 637: 18-25. DOI: 10.1016/j.neulet.2015.02.052. [45] CHATAURET N, ROSE C, BUTTERWORTH RF. Mild hypothermia in the prevention of brain edema in acute liver failure: mechanisms and clinical prospects[J]. Metab Brain Dis, 2002, 17(4): 445-451. DOI: 10.1023/a:1021982523691. [46] SHANGRAW RE, WINTER R, HROMCO J, et al. Amelioration of lactic acidosis with dichloroacetate during liver transplantation in humans[J]. Anesthesiology, 1994, 81(5): 1127-1138. DOI: 10.1097/00000542-199411000-00006. -



 PDF下载 ( 2047 KB)
PDF下载 ( 2047 KB)

 下载:
下载:


