Basic management of nonalcoholic fatty liver disease
-
-
临床上,胰腺恶性肿瘤大部分为原发肿瘤,胰腺转移癌少见[1]。胰腺转移癌与胰腺原发肿瘤鉴别困难,极易造成误诊,延误治疗。目前,胰腺转移癌国内外尚无统一治疗标准,原发肿瘤的生物学特性和针对原发肿瘤的综合治疗是决定其预后的主要因素,个体化差异较大。近期,笔者接诊1例宫颈鳞癌胰腺转移患者,现将病例资料及经验总结报告如下。
1. 病例资料
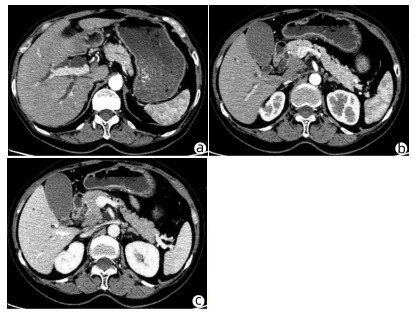
患者女性,63岁,因“皮肤、巩膜黄染20余天”于2021年3月27日入本院。起初黄染程度不重,后进行性加重,无腹痛腹胀,无阴道流血等其他不适。曾于2013年9月6日因阴道异常流血于外院行宫颈活检,病理学诊断为宫颈中分化鳞癌ⅢB期,予局部放疗联合TP方案(多西他赛+奥沙利铂)化疗,于2015年结束治疗后复查腹盆腔脏器、腹腔、盆腔均未见肿瘤转移。出院后患者再未复查,亦无特殊不适。入院查体:皮肤巩膜明显黄染,腹平坦,腹部无压痛,腹部未触及肿块。辅助检查:TBil 282.99 μmol/L,DBil 203.80 μmol/L,CA19-9正常;妇科彩超示:老年性子宫;全腹盆腔增强CT示:肝内外胆管扩张,主胰管可见(图 1a),胆囊明显增大,胆总管下段狭窄,动脉期见胰腺钩突区低密度肿块(图 1b),静脉期肿块轻度强化(图 1c),子宫显示不明显,腹膜后可见多发淋巴结肿大;磁共振胰胆管造影示:胰头区异常信号肿块,肝内外胆管扩张,胆汁淤积;超声内镜示:胰头钩突区占位,直径约3 cm。入院后予以护肝利胆治疗,患者黄疸进行性加重,建议患者行穿刺活检、PET-CT检查,患方拒绝。2021年4月4日行剖腹探查:术中探查发现肿瘤位于胰头钩突区,质地硬,侵犯十二指肠壁和胆总管,腹膜后见多发淋巴结肿大,行胰头十二指肠切除术。术后病理学检查结果:胰腺钩突肿块大小3.0 cm×2.0 cm×1.5 cm,癌组织侵犯十二指肠及胆总管,胰腺切缘未见癌。癌组织呈团块状或条索状癌巢(图 2a),癌细胞及核大小、形态不一,分布不规则,核分裂像多见,癌组织侵犯淋巴管及血管,脉管内见癌栓(图 2b),周围淋巴结可见癌转移(2/2)。免疫组化:P16(弥漫性+),P63(+),P40(+),CK7(+),CK8(+),CK19(+),ER(+)(图 2c、d)。诊断考虑胰腺钩突区中分化鳞状细胞癌,结合临床病史及免疫组化结果,考虑宫颈鳞癌转移。目前,该患者于本院进一步针对原发肿瘤行化疗等综合治疗,日常生活行为已恢复正常。
2. 讨论
据统计,宫颈癌的患病/病死率在女性恶性肿瘤中居第4位,鳞状细胞癌是最常见的病理类型,占比约80%,P16、P40等表达阳性对宫颈鳞癌诊断有重要意义。宫颈鳞癌早期往往无特殊表现,晚期可出现异常阴道流血、腰痛、盆腔痛、性交痛、贫血等表现,诊断时大多发生转移,多转移至直肠、膀胱、盆腔、肺、骨、肝等。临床上,胰腺癌多为原发肿瘤,胰腺转移癌罕见,仅占胰腺恶性肿瘤总数的2%~3%[2]。在一项纳入973例胰腺肿瘤手术标本病理资料的研究[3]中,共38例为胰腺转移瘤,主要包括淋巴瘤11例,胃癌7例,肾癌6例,肺癌2例,肝癌、前列腺癌、卵巢癌、子宫癌各1例,默克尔细胞癌1例,另有3例胃肠道恶性间质瘤和1例腹膜后平滑肌肉瘤;81例转移性胰腺肿瘤尸检报告显示,主要来源肺癌34例,胃肠道20例,肾脏4例,乳腺3例,肝脏2例,卵巢和膀胱各1例,另有6例来自造血系统,黑色素瘤、肉瘤和间皮瘤各2例。来源于宫颈的胰腺转移癌并不多见,笔者在国内外文献检索系统中,共检出各类型宫颈癌胰腺转移病例报告10例[4-7],其中鳞癌3例,神经内分泌癌5例,腺癌2例;转移灶位于胰头3例,位于颈部1例,位于胰腺体部3例,位于尾部、体尾部和胰头及体尾部各1例。转移灶位于胰头的3例患者中,1例为鳞癌,2例为神经内分泌癌,胰腺转移部位与宫颈癌病理类型无明显关联。本例患者在宫颈鳞癌同步放化疗后再未复查,6年后转移至胰腺钩突,临床表现为梗阻性黄疸,行胰头十二指肠切除术,术后病理学检查考虑鳞癌,结合免疫组化考虑为宫颈癌来源。目前,国内尚未见类似报道,国外也鲜有相关报道。
原发性胰腺癌与胰腺转移癌鉴别需依赖血清CA19-9水平、CT、MRI、磁共振胰胆管造影、内镜逆行胰胆管造影、超声内镜等检查手段。本例患者CT和MRI特点较原发性胰腺癌无特异表现,鉴别困难。血清CA19-9水平升高常见于胆道、胰腺恶性肿瘤,对诊断原发性胰腺癌有较高的敏感度和特异度[8]。鉴别困难时,可采用通过超声、CT及内镜引导下穿刺活检获取胰腺组织学、细胞学标本进行确诊,但需要评估穿刺活检的出血风险[9]。一般认为,超声内镜经十二指肠细针穿刺抽吸活检可提高胰腺疾病诊断的准确性,且相对安全[10-11]。本例患者术前影像学检查提示胰头钩突区占位,CA19-9水平不高,且有宫颈鳞癌病史,建议进一步行穿刺活检、PET-CT检查。但患者存在梗阻性黄疸,肝功能持续恶化,有手术指征,且患者家属不同意术前行穿刺活检、PET-CT等进一步检查,因此术前未能获得病理学诊断。
转移性胰腺癌临床表现因胰腺转移部位不同而异。在笔者检出的10例报告中,仅有1例(鳞癌)出现梗阻性黄疸,提示宫颈癌胰腺转移鲜有梗阻性黄疸症状,部分病例可因肿瘤压迫出现胆胰管扩张。转移性胰腺癌出现胰胆管梗阻较少见,可能与原发肿瘤主要经过淋巴及血行途径转移侵犯胰腺,不侵犯胆胰管有关[12]。本例患者胰腺转移性肿瘤致梗阻性黄疸,目前国内尚未见类似报道,国外仅有1例类似报道,但未分析相关转移机制。本例患者影像学检查示肝、胃、肠道等器官均未见肿瘤,但有腹膜后淋巴结肿大,病理学检查阳性;在既往10例报告中,3例胰腺转移性宫颈鳞癌有2例伴腹膜后淋巴结肿大,因此笔者推测宫颈鳞癌胰腺转移可能与腹膜后淋巴结侵犯相关。
关于转移性胰腺癌是否需要手术,意见尚未统一。以急腹症、进行性黄疸、出血为临床表现患者,应行急诊手术治疗,解除症状同时,切除病灶送检,根据病理学检查结果制订综合治疗方案。研究[13-14]表明,转移性胰腺癌行手术切除相较于保守治疗可延长生存期,且根治性手术相较于姑息性手术,预后更好。术后根据原发病灶辅以化疗等综合治疗,可提高治疗效果。对无法接受手术的转移性胰腺癌患者,应根据原发肿瘤的生物学特性制订以放疗为主的个体化综合治疗方案[15]。本例患者影像学检查提示存在胆道梗阻,并见胰头钩突区占位;胆红素水平持续升高,手术指征明确,手术切除胰腺钩突病灶、解除胆道梗阻后,胆红素水平明显下降,目前患者恢复良好,进一步接受化疗等综合治疗,延长生存期。
笔者经验总结:(1)对于诊断不明确的胰腺肿瘤,术前条件允许情况下需行穿刺活检明确性质,以指导下一步治疗方案;(2)胰腺转移癌在具备手术条件情况下,应积极采取以根治性手术为主的治疗方案,姑息性切除方案亦可行。胰腺转移癌为晚期癌症,术后需早期予以放化疗、靶向、免疫治疗等综合治疗;(3)对于不具备手术条件的患者,需根据原发肿瘤予以抗肿瘤综合治疗,包括放疗、化疗以及免疫治疗、靶向治疗等[16-17]。
-
[1]Fan JG, Zhu J, Li XJ, et al.Prevalence of and risk factors for fatty liver in a general population of Shanghai, China[J].J Hepatol, 2005, 43 (3) :508-514. [2]Amarapurkar DN, Hashimoto E, Lesmana LA, et al.How common is non-alcoholic fatty liver disease in the Asia-Pacific region and are there local differences-[J].J Gastroenterol Hepatol, 2007, 22 (6) :788-793. [3]Ekstedt M, Franzen LE, Mathiesen UL, et al.Long-term follow-up of patients with NAFLD and elevated liver enzymes[J].Hepatolo-gy, 2006, 44 (4) :865-873. [4]Wong VW, Chan HL, Hui AY, et al.Clinical and histological fea-tures of non-alcoholic fatty liver disease in Hong Kong Chinese[J].Aliment Pharmacol Ther, 2004, 20 (1) :45-49. [5]Hui AY, Wong VW, Chan HL, et al.Histological progression of non-alcoholic fatty liver disease in Chinese patients[J].Aliment Phar-macol Ther, 2005, 21 (4) :407-413. [6]Farrell GC, Chitturi S, Lau GK, et al.Guidelines for the assessment and management of non-alcoholic fatty liver disease in the Asia-Pacific region:executive summary[J].J Gastroenterol Hepatol, 2007, 22 (6) :775-777. [7]Wong VW, Hui AY, Tsang SW, et al.Metabolic and adipokine pro-file of Chinese patients with nonalcoholic fatty liver disease[J].Clin Gastroenterol Hepatol, 2006, 4 (9) :1154-1161. [8]Targher G, Bertolini L, Rodella S, et al.Nonalcoholic fatty liver disease is independently associated with an increased incidence of cardiovascular events in type2diabetic patients[J].Diabetes Care, 2007, 30 (8) :2119-2121. [9]Wong VW, Hui AY, Tsang SW, et al.Prevalence of undiagnosed diabetes and postchallenge hyperglycaemia in Chinese patients with non-alcoholic fatty liver disease[J].Aliment Pharmacol Ther, 2006, 24 (8) :1215-1222. [10]Merriman RB, Ferrell LD, Patti MG, et al.Correlation of paired liver biopsies in morbidly obese patients with suspected nonalcoholic fatty liver disease[J].Hepatology, 2006, 44 (4) :874-880. [11]Chan HL.Non-invasive assessment of NAFLD[J].J Clin Hepa-tol, 2010, 26 (1) . [12]Feldstein AE, Wieckowska A, Lopez AR, et al.Cytokeratin-18fragment levels as noninvasive biomarkers for nonalcoholic steatohepa-titis:a multicenter validation study[J].Hepatology, 2009, 50 (4) :1072-1078. [13]Wong VW, Verginol J, Wong GL, et al.Diagnosis of fibrosis and cirrhosis using liver stiffness measurement in nonalcoholic fatty liver disease[J].Hepatology, 2010, 51 (2) :454-462. [14]Knowler WC, Barrett-Connor E, Fowler SE.Reduction in the in-cidence of type2diabetes with lifestyle intervention or metformin[J].N Engl J Med, 2002, 346 (6) :393-403. [15]Musso G, Gambino R, De Michieli F, et al.Dietary habits and their relations to insulin resistance and postprandial lipemia in nonal-coholic steatohepatitis[J].Hepatology, 2003, 37 (4) :909-916. [16]Solga S, Alkhuraishe AR, Clark JM, et al.Diehl AM, Magnuson T.Dietary composition and nonalcoholic fatty liver disease[J].Dig Dis Sci, 2004, 49 (10) :1578-1583. [17]Cortez-Pinto H, Jesus L, Barros H, et al.Howdifferent is the di-etary pattern in non-alcoholic steatohepatitis patients-[J].Clin Nutr, 2006, 25 (5) :816-823. [18]Ouyang X, Cirillo P, Sautin Y, et al.Fructose consumption as a risk factor for non-alcoholic fatty liver disease[J].J Hepatol, 2008, 48 (6) :993-999. [19]Cortez-Pinto H, Chatham J, Chacko VP, et al.Alterations in liv-er ATP homeostasis in human nonalcoholic steatohepatitis:a pilot study[J].JAMA, 1999, 282 (17) :1659-1664. [20]Daubioul CA, Horsmans Y, Lambert P, et al.Effects of oligofruc-tose on glucose and lipid metabolism in patients with nonalcoholic steatohepatitis:results of a pilot study[J].Eur J Clin Nutr, 2005, 59 (5) :723-726. [21]Gasteyger C, Larsen TM, Vercruysse F, et al.Effect of a dietary-induced weight loss on liver enzymes in obese subjects[J].Am J Clin Nutr, 2008, 87 (5) :1141-1147. [22]St George A, Bauman A, Johnston A, et al.Effect of a lifestyle in-tervention in patients with abnormal liver enzymes and metabolic risk factors[J].J Gastroenterol Hepatol, 2009, 24 (3) :399-407. [23]Huang MA, Greenson JK, Chao C, et al.One-year intense nutri-tional counseling results in histological improvement in patients with non-alcoholic steatohepatitis:a pilot study[J].Am J Gastroen-terol, 2005, 100 (5) :1072-1081. [24]Kirk E, Reeds DN, Finck BN, et al.Dietary fat and carbohydrates differentially alter insulin sensitivity during caloric restriction[J].Gastroenterology, 2009, 136 (5) :1552-1560. [25]Shai I, Schwarzfuchs D, Henkin Y, et al.Weight loss with a low-carbohydrate, Mediterranean, or low-fat diet[J].N Engl J Med, 2008, 359 (3) :229-241. [26]Zelber-Sagi S, Nitzan-Kaluski D, Goldsmith R, et al.Role of leisure-time physical activity in nonalcoholic fatty liver disease:a population-based study[J].Hepatology, 2008, 48 (6) :1791-1798. [27]Kugelmas M, Hill DB, Vivian B, et al.Cytokines and NASH:a pilot study of the effects of lifestyle modification and vitamin E[J].Hepatology, 2003, 38 (2) :413-419. [28]Hickman IJ, Jonsson JR, Prins JB, et al.Modest weight loss andphysical activity in overweight patients with chronic liver disease re-sults in sustained improvements in alanine aminotransferase, fasting insulin, and quality of life[J].Gut, 2004, 53 (3) :413-419. [29]Osland EJ, Powell EE, Banks M, et al.Obesity management in liver clinics:translation of research into clinical practice[J].J Gas-troenterol Hepatol, 2007, 22 (4) :504-509. [30]St George A, Bauman A, Johnston A, et al.Independent effects of physical activity in patients with nonalcoholic fatty liver disease[J].Hepatology, 2009, 50 (1) :68-76. [31]Johnson NA, Sachinwalla T, Walton DW, et al.Aerobic exercise training reduces hepatic and visceral lipids in obese individuals with-out weight loss[J].Hepatology, 2009, 50 (4) :1105-1112. [32]Harrison SA, Torgerson S, Hayashi P, et al.Vitamin E and vita-min C treatment improves fibrosis in patients with nonalcoholic steato-hepatitis[J].Am J Gastroenterol, 2003, 98 (11) :2485-2490. [33]Ersoz G, Gunsar F, Karasu Z, et al.Management of fatty liver dis-ease with vitamin E and C compared to ursodeoxycholic acid treat-ment[J].Turk J Gastroenterol, 2005, 16 (3) :124-128. [34]Nobili V, Manco M, Devito R, et al.Lifestyle intervention and an-tioxidant therapy in children with nonalcoholic fatty liver disease:a randomized, controlled trial[J].Hepatology, 2008, 48 (1) :119-128. [35]Santos VN, Lanzoni VP, Szejnfeld J, et al.Arandomized double-blind study of the short-time treatment of obese patients with nonal-coholic fatty liver disease with ursodeoxycholic acid[J].Braz J Med Biol Res, 2003, 36 (6) :723-729. [36]Lindor KD, Kowdley KV, Heathcote EJ, et al.Ursodeoxycholic acid for treatment of nonalcoholic steatohepatitis:results of a random-ized trial[J].Hepatology, 2004, 39 (3) :770-778. [37]Bugianesi E, Gentilcore E, Manini R, et al.A randomized con-trolled trial of metformin versus vitamin E or prescriptive diet in non-alcoholic fatty liver disease[J].Am J Gastroenterol, 2005, 100 (5) :1082-1090. [38]Nair S, Diehl AM, Wiseman M, et al.Metformin in the treatment of non-alcoholic steatohepatitis:a pilot open label trial[J].Ali-ment Pharmacol Ther, 2004, 20 (1) :23-28. [39]Sanyal AJ, Mofrad PS, Contos MJ, et al.Apilot study of vitamin E versus vitamin E and pioglitazone for the treatment of nonalcoholic steatohepatitis[J].Clin Gastroenterol Hepatol, 2004, 2 (12) :1107-1115. [40]Belfort R, Harrison SA, Brown K, et al.Aplacebo-controlled tri-al of pioglitazone in subjects with nonalcoholic steatohepatitis[J].N Engl J Med, 2006, 355 (22) :2297-2307. [41]Ratziu V, Giral P, Jacqueminet S, et al.Rosiglitazone for nonalco-holic steatohepatitis:one-year results of the randomized placebo-controlled Fatty Liver Improvement with Rosiglitazone Therapy (FLIRT) Trial[J].Gastroenterology, 2008, 135 (1) :100-110. [42]Aithal GP, Thomas JA, Kaye PV, et al.Randomized, placebo-controlled trial of pioglitazone in nondiabetic subjects with nonalco-holic steatohepatitis[J].Gastroenterology, 2008, 135 (4) :1176-1184. [43]Lutchman G, Modi A, Kleiner DE, et al.The effects of discontinu-ing pioglitazone in patients with nonalcoholic steatohepatitis[J].Hepatology, 2007, 46 (2) :424-429. [44]Krall RL.Cardiovascular safety of rosiglitazone[J].Lancet, 2007, 369 (9578) :1995-1996. [45]Balas B, Belfort R, Harrison SA, et al.Pioglitazone treatment in-creases whole body fat but not total body water in patients with non-alcoholic steatohepatitis[J].J Hepatol, 2007, 47 (4) :565-570. [46]Jonsson JR, Clouston AD, Ando Y, et al.Angiotensin-converting enzyme inhibition attenuates the progression of rat hepatic fibrosis[J].Gastroenterology, 2001, 121 (1) :148-155. [47]Yokohama S, Yoneda M, Haneda M, et al.Therapeutic efficacy of an angiotensin II receptor antagonist in patients with nonalcoholic steatohepatitis[J].Hepatology, 2004, 40 (5) :1222-1225. [48]Harrison SA, Fecht W, Brunt EM, et al.Orlistat for overweight subjects with nonalcoholic steatohepatitis:Arandomized, prospective trial[J].Hepatology, 2009, 49 (1) :80-86. [49]Osei-Hyiaman D, Liu J, Zhou L, et al.Hepatic CB1receptor is required for development of diet-induced steatosis, dyslipidemia, and insulin and leptin resistance in mice[J].J Clin Invest, 2008, 118 (9) :3160-3169. [50]Gary-Bobo M, Elachouri G, Gallas JF, et al.Rimonabant reduces obesity-associated hepatic steatosis and features of metabolic syn-drome in obese Zucker fa/fa rats[J].Hepatology, 2007, 46 (1) :122-129. [51]Ekstedt M, Franzen LE, Mathiesen UL, et al.Statins in non-al-coholic fatty liver disease and chronically elevated liver enzymes:a histopathological follow-up study[J].J Hepatol, 2007, 47 (1) :135-141. [52]Lewis JH, Mortensen ME, Zweig S, et al.Efficacy and safety of high-dose pravastatin in hypercholesterolemic patients with well-compensated chronic liver disease:Results of a prospective, random-ized, double-blind, placebo-controlled, multicenter trial[J].Hepatology, 2007, 46 (5) :1453-1463. [53]Adams TD, Gress RE, Smith SC, et al.Long-term mortality after gastric bypass surgery[J].N Engl J Med, 2007, 357 (8) :753-761. [54]Sjostrom L, Narbro K, Sjostrom CD, et al.Effects of bariatric sur-gery on mortality in Swedish obese subjects[J].N Engl J Med, 2007, 357 (8) :741-752. [55]Mathurin P, Hollebecque A, Arnalsteen L, et al.Prospective study of the long-termeffects of bariatric surgery on liver injury in patients without advanced disease[J].Gastroenterology, 2009, 137 (2) :532-540. 期刊类型引用(1)
1. 李帅,王娟,夏仕雪,顾鹏. 子宫颈混合性腺神经内分泌癌胰腺转移1例. 中国医学影像学杂志. 2022(12): 1283-1284 .  百度学术
百度学术其他类型引用(0)
-




 PDF下载 ( 223 KB)
PDF下载 ( 223 KB)


 下载:
下载:

 百度学术
百度学术
 下载:
下载: