肝/脾CT值、受控衰减参数(CAP)和磁共振质子密度脂肪分数(MRI-PDFF)在慢性乙型肝炎脂肪变性患者中的应用价值
DOI: 10.12449/JCH240109
Application value of liver/spleen CT value, controlled attenuation parameter, and magnetic resonance imaging-proton density fat fraction in chronic hepatitis B patients with hepatic steatosis
-
摘要:
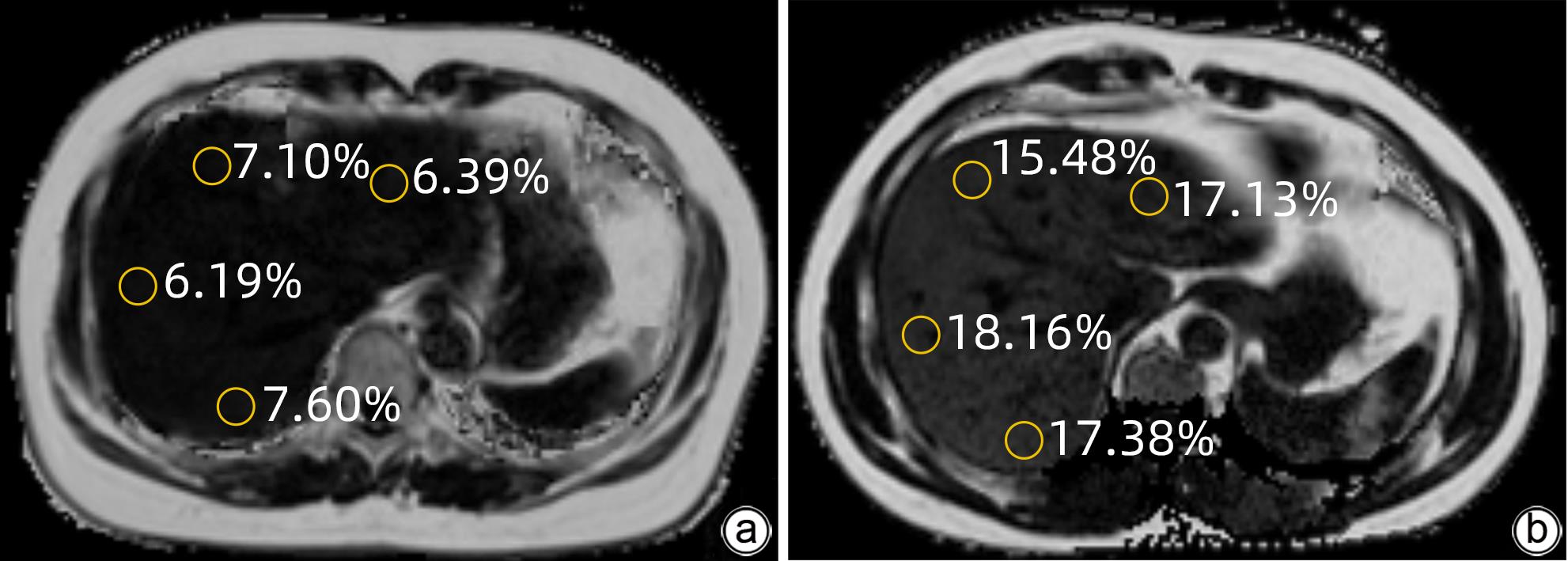
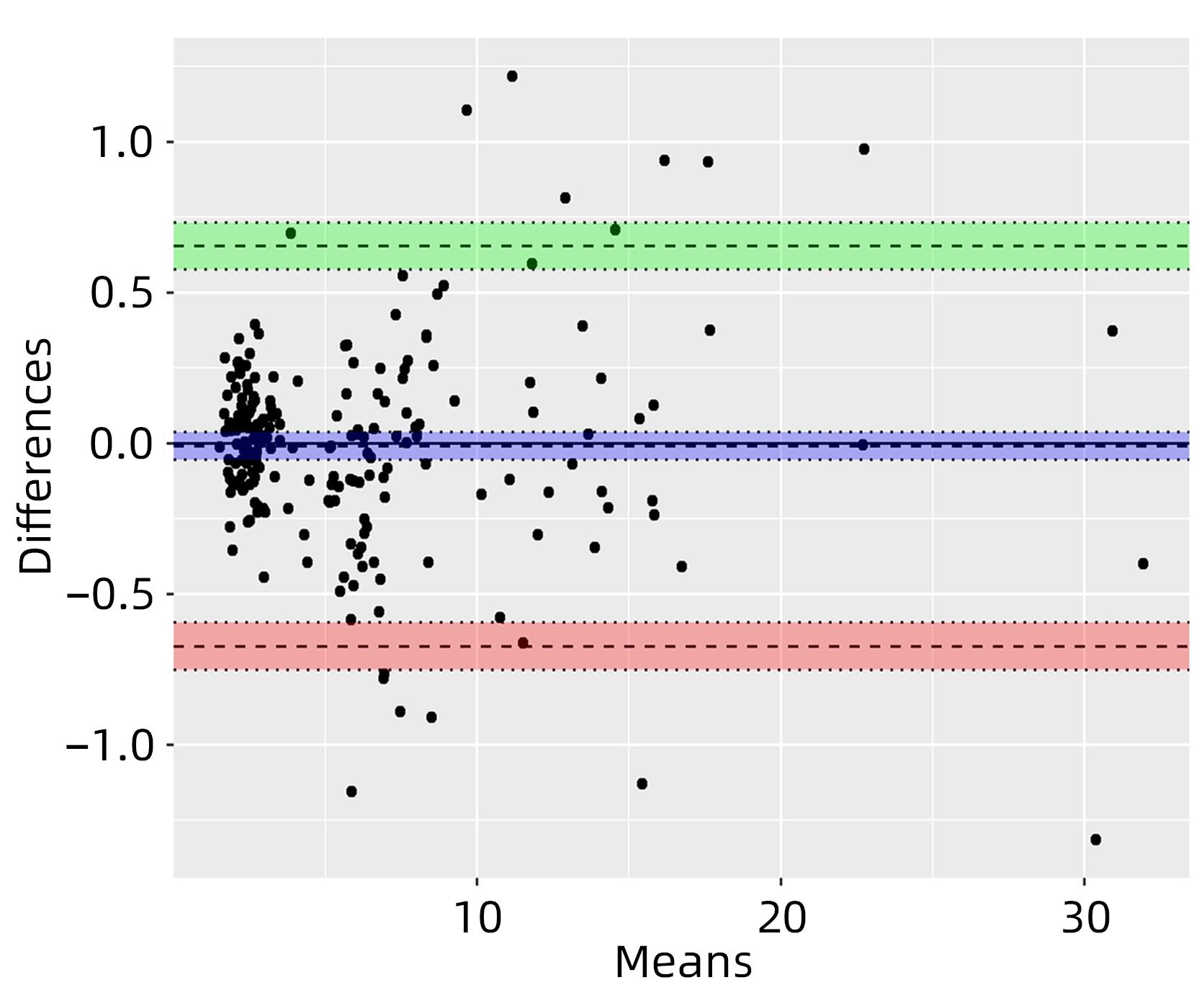
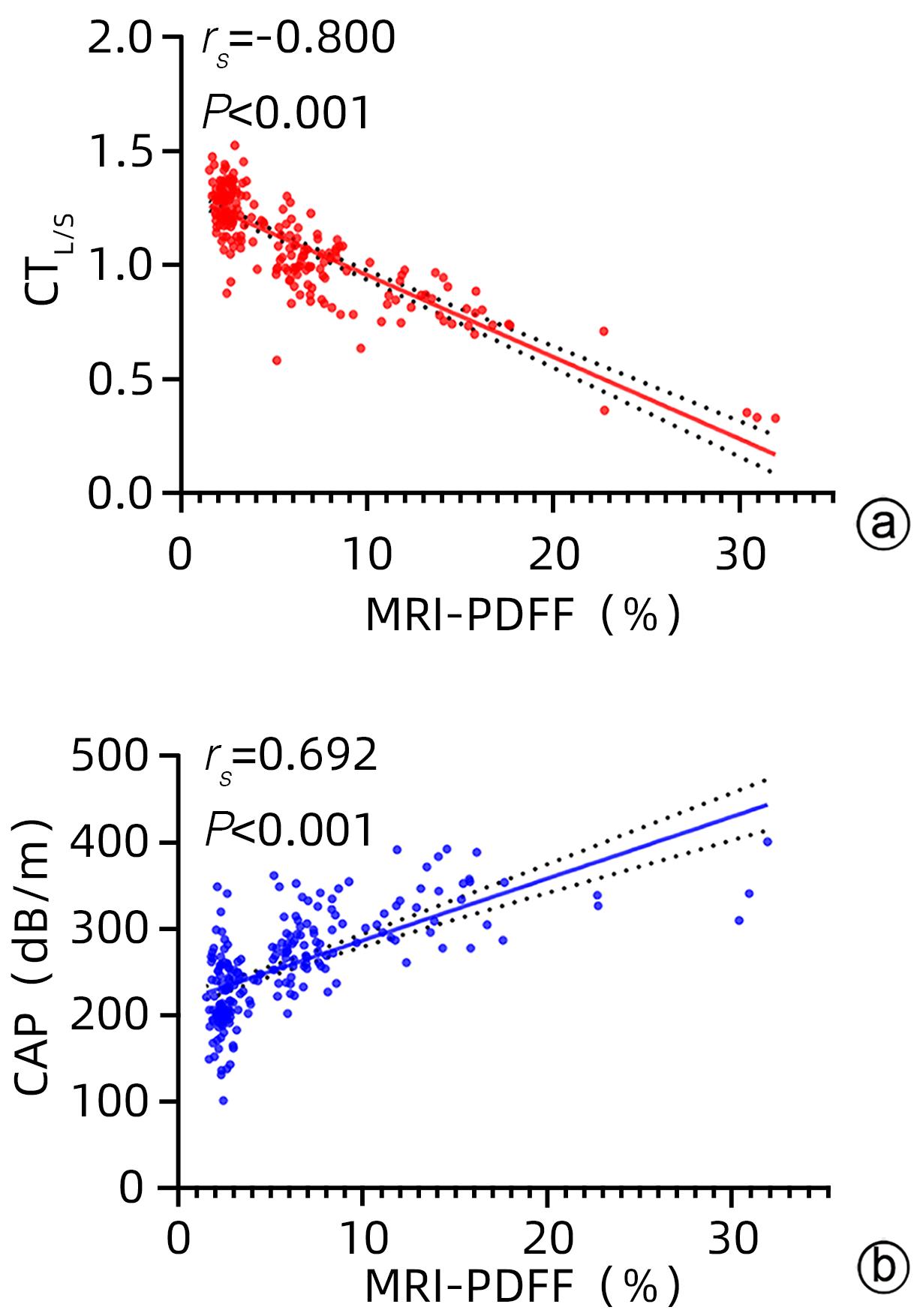
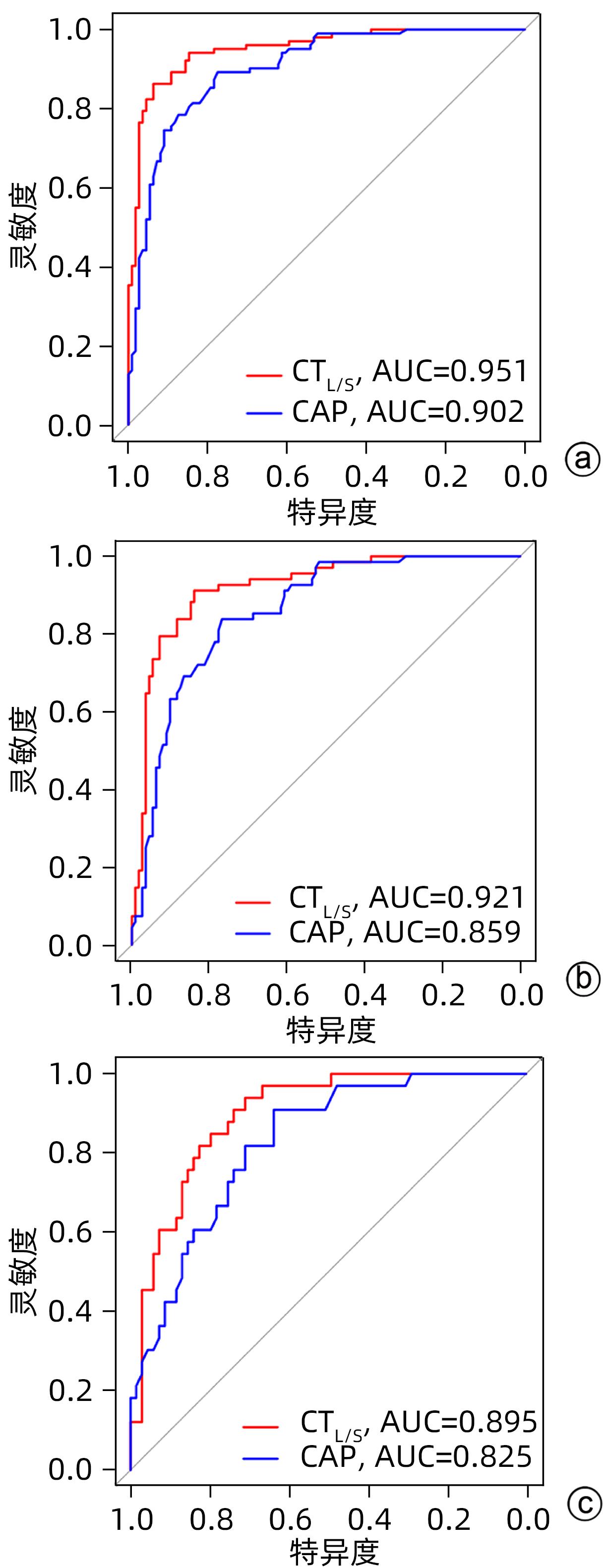
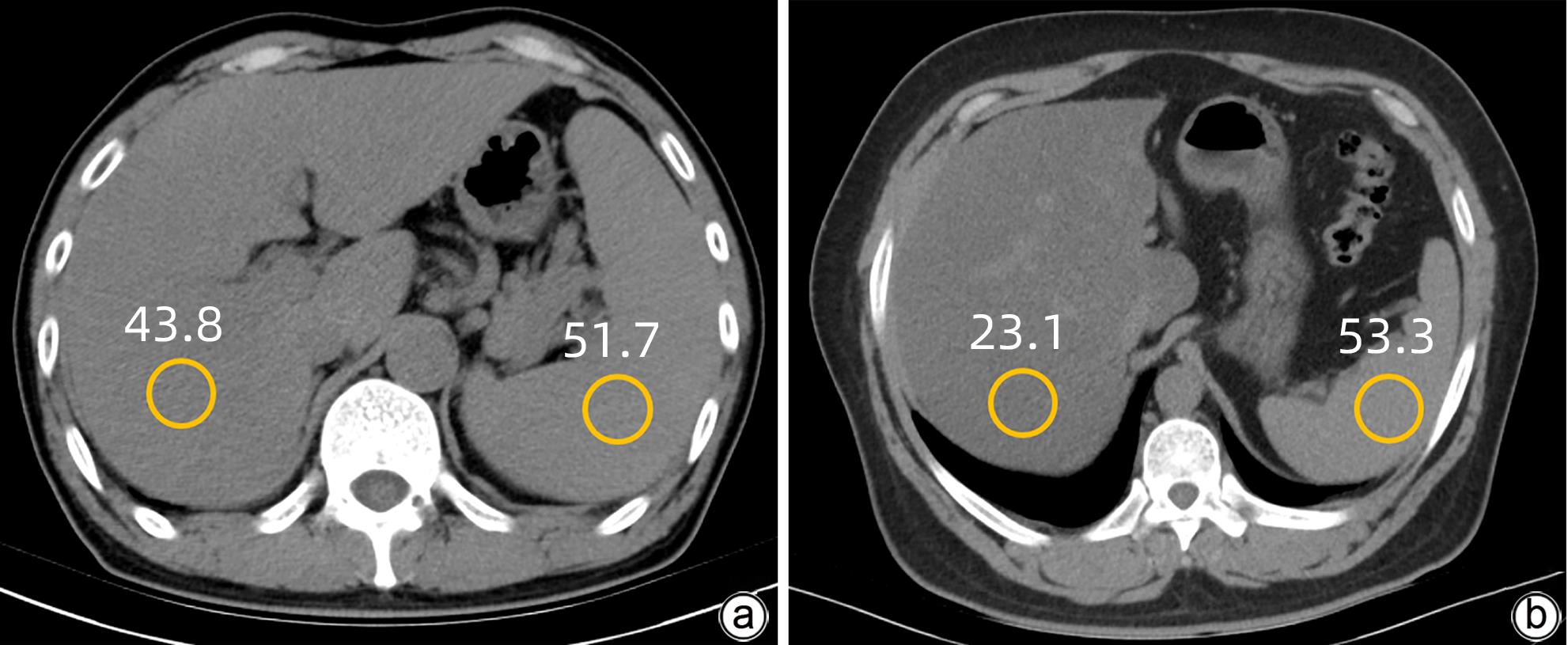
目的 探讨肝/脾CT值(CTL/S)、受控衰减参数(CAP)和磁共振质子密度脂肪分数(MRI-PDFF)在慢性乙型肝炎(CHB)肝脂肪变性患者中的应用价值。 方法 回顾性收集2018年10月—2022年12月在延安大学附属医院行肝脏CT、CAP和MRI-PDFF检查的213例CHB患者的临床资料。根据MRI-PDFF结果,将213例患者分为单纯CHB组(MRI-PDFF<5%,n=111)和CHB合并脂肪变性组(MRI-PDFF≥5%,n=102);其中轻度脂肪变性69例,中度至重度脂肪变性33例。符合正态分布的计量资料组间比较采用成组t检验;不符合正态分布的计量资料组间比较采用Mann-Whitney U检验。绘制Bland-Altman图,评价两位医师测量MRI-PDFF的一致性。采用Spearman相关系数分析CTL/S和MRI-PDFF、CAP和MRI-PDFF的相关性。通过分析受试者工作特征曲线(ROC曲线),计算曲线下面积(AUC),评估CTL/S和CAP对不同程度脂肪变性的诊断价值,并使用DeLong检验比较两种影像诊断方法的AUC。 结果 MRI-PDFF在CHB患者中具有较高的可重复性及稳定性,CTL/S和MRI-PDFF之间呈显著负相关(r=-0.800,P<0.001),CAP与MRI-PDFF之间呈显著正相关(r=0.692,P<0.001)。CTL/S和CAP诊断CHB肝脂肪变性均有较高的准确度(AUC分别为0.951、0.902),且CTL/S优于CAP(P<0.05)。在检测轻度和中重度脂肪变性时,CTL/S的AUC分别为0.921和0.895,CAP的AUC分别为0.859和0.825。 结论 MRI-PDFF技术在CHB患者中具有较高的可重复性及稳定性,CTL/S和CAP对不同程度的CHB肝脂肪变性均具有较高的诊断价值。 Abstract:Objective To investigate the application value of liver/spleen CT value (CTL/S), controlled attenuation parameter (CAP), and magnetic resonance imaging-proton density fat fraction (MRI-PDFF) in chronic hepatitis B (CHB) patients with hepatic steatosis. Methods A retrospective analysis was performed for the clinical data of 213 CHB patients who underwent liver CT, CAP, and MRI-PDFF examinations in Affiliated Hospital of Yan’an University from October 2018 to December 2022. According to MRI-PDFF, the 213 patients were divided into CHB group with 111 patients (MRI-PDFF<5%) and CHB+hepatic steatosis group with 102 patients (MRI-PDFF≥5%), among whom there were 69 patients with mild hepatic steatosis and 33 patients with moderate to severe hepatic steatosis. The independent-samples t test was used for comparison of normally distributed continuous data between groups, and the Mann-Whitney U test was used for comparison of non-normally distributed continuous data between groups. The Bland-Altman plot was used to evaluate the consistency in MRI-PDFF measurement between two physicians. The Spearman’s correlation coefficient was used to analyze the correlation between CTL/S and MRI-PDFF and between CAP and MRI-PDFF. The receiver operating characteristic (ROC) curve was plotted and the area under the ROC curve (AUC) was calculated to investigate the value of CTL/S and CAP in the diagnosis of different degrees of hepatic steatosis, and the DeLong test was used to compare the AUCs of the two radiological examinations. Results MRI-PDFF had relatively high repeatability and stability in CHB patients. There is a significant negative correlation between CTL/S and MRI-PDFF (r=-0.800, P<0.001) and a significant positive correlation between CAP and MRI-PDFF (r=0.692, P<0.001). Both CTL/S and CAP had a relatively high accuracy in the diagnosis of hepatic steatosis in CHB patients, with an AUC of 0.951 and 0.902, respectively, and CTL/S had a better accuracy than CAP (P<0.05). In the diagnosis of mild and moderate-to-severe hepatic steatosis, CTL/S had an AUC of 0.921 and 0.895, respectively, and CAP had an AUC of 0.859 and 0.825, respectively, suggesting that CTL/S had a slightly higher diagnostic efficiency than CAP. Conclusion MRI-PDFF has high repeatability and stability in CHB patients, and CTL/S and CAP have a high diagnostic value for different degrees of hepatic steatosis in CHB patients. -
Key words:
- Hepatitis B, Chronic /
- Fatty Liver /
- Diagnosis
-
表 1 单纯CHB组和CHB合并脂肪变性组的临床特征、影像学特征比较
Table 1. Comparison of clinical and imaging features between simple CHB group and CHB with steatosis group
项目 单纯CHB组(n=111) CHB合并脂肪变性组(n=102) 统计值 P值 性别[例(%)] χ2=6.191 0.013 男 66(59) 77(75) 女 45(41) 25(25) 年龄(岁) 50.00±11.17 47.00±9.79 t=0.146 0.084 BMI(kg/m2) 23.67(21.86~25.26) 26.38(23.88~28.40) Z=-5.887 P<0.001 CAP(dB/m) 216.00±42.21 291.50±42.91 t=-14.236 P<0.001 CTL/S 1.27(1.20~1.34) 0.97(0.83~1.04) Z=-11.368 P<0.001 MRI-PDFF 2.45%(2.19%~2.80%) 7.55%(6.12%~11.85%) Z=-12.598 P<0.001 表 2 CTL/S和CAP对慢性乙型肝炎不同程度脂肪变性的诊断效能
Table 2. Diagnostic efficacy of CTL/S and CAP for different degrees of steatosis in chronic hepatitis B
项目 无脂肪变性 vs 脂肪变性 无脂肪变性 vs 轻度脂肪变性 轻度脂肪变性 vs 中重度脂肪变性 CTL/S 最佳截断值 1.09 1.17 0.97 AUC 0.951 0.921 0.895 灵敏度(%) 86.3 91.2 93.9 特异度(%) 93.7 83.9 71.0 阳性预测值(%) 92.6 77.5 60.8 阴性预测值(%) 88.1 94.0 96.1 CAP 最佳截断值 251.5 251.5 285.5 AUC 0.9021) 0.859 0.825 灵敏度(%) 89.2 83.8 90.9 特异度(%) 77.5 76.8 63.8 阳性预测值(%) 78.4 68.7 54.5 阴性预测值(%) 88.7 88.7 93.6 注:与CTL/S比较,1)P<0.05。 -
[1] Polaris Observatory Collaborators. Global prevalence, treatment, and prevention of hepatitis B virus infection in 2016: a modelling study[J]. Lancet Gastroenterol Hepatol, 2018, 3( 6): 383- 403. DOI: 10.1016/S2468-1253(18)30056-6. [2] ZHOU WW, HUANG J, PAN FM. Research progress in epidemiological characteristics and therapeutic drugs of chronic hepatitis B[J]. J Changchun Univ Chin Med, 2022, 38( 12): 1420- 1424. DOI: 10.13463/j.cnki.cczyy.2022.12.028.周薇薇, 黄俊, 潘发明. 慢性乙型肝炎流行病学特点和治疗药物研究进展[J]. 长春中医药大学学报, 2022, 38( 12): 1420- 1424. DOI: 10.13463/j.cnki.cczyy.2022.12.028. [3] RINELLA ME, NEUSCHWANDER-TETRI BA, SIDDIQUI MS, et al. AASLD Practice Guidance on the clinical assessment and management of nonalcoholic fatty liver disease[J]. Hepatology, 2023, 77( 5): 1797- 1835. DOI: 10.1097/HEP.0000000000000323. [4] LEE YB, HA Y, CHON YE, et al. Association between hepatic steatosis and the development of hepatocellular carcinoma in patients with chronic hepatitis B[J]. Clin Mol Hepatol, 2019, 25( 1): 52- 64. DOI: 10.3350/cmh.2018.0040. [5] SHIHA G, IBRAHIM A, HELMY A, et al. Asian-Pacific Association for the Study of the Liver(APASL) consensus guidelines on invasive and non-invasive assessment of hepatic fibrosis: a 2016 update[J]. Hepatol Int, 2017, 11( 1): 1- 30. DOI: 10.1007/s12072-016-9760-3. [6] ROGIER J, ROULLET S, CORNÉLIS F, et al. Noninvasive assessment of macrovesicular liver steatosis in cadaveric donors based on computed tomography liver-to-spleen attenuation ratio[J]. Liver Transpl, 2015, 21( 5): 690- 695. DOI: 10.1002/lt.24105. [7] FERRAIOLI G. Quantitative assessment of liver steatosis using ultrasound controlled attenuation parameter(Echosens)[J]. J Med Ultrason(2001), 2021, 48( 4): 489- 495. DOI: 10.1007/s10396-021-01106-1. [8] Committee of Hepatology, Chinese Research Hospital Association, Fatty Liver Expert Committee, Chinese Medical Doctor Association, National Workshop on Fatty Liver and Alcoholic Liver Disease, Chinese Society of Hepatology, et al. Expert recommendations on standardized diagnosis and treatment for fatty liver disease(2019 revised edition)[J]. J Clin Hepatol, 2019, 35( 11): 2426- 2430. DOI: 10.3969/j.issn.1001-5256.2019.11.007.中国研究型医院学会肝病专业委员会, 中国医师协会脂肪性肝病专家委员会, 中华医学会肝病学分会脂肪肝与酒精性肝病学组, 等. 脂肪性肝病诊疗规范化的专家建议(2019年修订版)[J]. 临床肝胆病杂志, 2019, 35( 11): 2426- 2430. DOI: 10.3969/j.issn.1001-5256.2019.11.007. [9] TAMAKI N, AJMERA V, LOOMBA R. Non-invasive methods for imaging hepatic steatosis and their clinical importance in NAFLD[J]. Nat Rev Endocrinol, 2022, 18( 1): 55- 66. DOI: 10.1038/s41574-021-00584-0. [10] DULAI PS, SIRLIN CB, LOOMBA R. MRI and MRE for non-invasive quantitative assessment of hepatic steatosis and fibrosis in NAFLD and NASH: Clinical trials to clinical practice[J]. J Hepatol, 2016, 65( 5): 1006- 1016. DOI: 10.1016/j.jhep.2016.06.005. [11] National Workshop on Fatty Liver and Alcoholic Liver Disease, Chinese Society of Hepatology, Chinese Medical Association, Fatty Liver Expert Committee, Chinese Medical Doctor Association. Guidelines of prevention and treatment for nonalcoholic fatty liver disease: A 2018 update[J]. J Clin Hepatol, 2018, 34( 5): 947- 957. DOI: 10.3969/j.issn.1001-5256.2018.05.007.中华医学会肝病学分会脂肪肝和酒精性肝病学组, 中国医师协会脂肪性肝病专家委员会. 非酒精性脂肪性肝病防治指南(2018年更新版)[J]. 临床肝胆病杂志, 2018, 34( 5): 947- 957. DOI: 10.3969/j.issn.1001-5256.2018.05.007. [12] YE J, WU Y, LI F, et al. Effect of orlistat on liver fat content in patients with nonalcoholic fatty liver disease with obesity: assessment using magnetic resonance imaging-derived proton density fat fraction[J]. Therap Adv Gastroenterol, 2019, 12: 1756284819879047. DOI: 10.1177/1756284819879047. [13] YANG M, WEI L. Impact of NAFLD on the outcome of patients with chronic hepatitis B in Asia[J]. Liver Int, 2022, 42( 9): 1981- 1990. DOI: 10.1111/liv.15252. [14] CASTERA L, FRIEDRICH-RUST M, LOOMBA R. Noninvasive assessment of liver disease in patients with nonalcoholic fatty liver disease[J]. Gastroenterology, 2019, 156( 5): 1264- 1281.e4. DOI: 10.1053/j.gastro.2018.12.036. [15] PARK CC, NGUYEN P, HERNANDEZ C, et al. Magnetic resonance elastography vs transient elastography in detection of fibrosis and noninvasive measurement of steatosis in patients with biopsy-proven nonalcoholic fatty liver disease[J]. Gastroenterology, 2017, 152( 3): 598- 607.e2. DOI: 10.1053/j.gastro.2016.10.026. [16] LEE SS, PARK SH. Radiologic evaluation of nonalcoholic fatty liver disease[J]. World J Gastroenterol, 2014, 20( 23): 7392- 7402. DOI: 10.3748/wjg.v20.i23.7392. [17] ZHONG L, CHEN JJ, CHEN J, et al. Nonalcoholic fatty liver disease: quantitative assessment of liver fat content by computed tomography, magnetic resonance imaging and proton magnetic resonance spectroscopy[J]. J Dig Dis, 2009, 10( 4): 315- 320. DOI: 10.1111/j.1751-2980.2009.00402.x. [18] CHEN S, HUANG ZH. Advances in quantitative imaging evaluation of non-alcoholic fatty liver disease[J]. J New Clin Medicine, 2018, 11( 12): 1283- 1286. DOI: 10.3969/j.issn.1674-3806.2018.12.32.陈松, 黄泽和. 非酒精性脂肪肝病的影像学定量评估研究进展[J]. 中国临床新医学, 2018, 11( 12): 1283- 1286. DOI: 10.3969/j.issn.1674-3806.2018.12.32. [19] KARLAS T, PETROFF D, SASSO M, et al. Individual patient data meta-analysis of controlled attenuation parameter(CAP) technology for assessing steatosis[J]. J Hepatol, 2017, 66( 5): 1022- 1030. DOI: 10.1016/j.jhep.2016.12.022. [20] NOGAMI A, YONEDA M, IWAKI M, et al. Non-invasive imaging biomarkers for liver steatosis in non-alcoholic fatty liver disease: present and future[J]. Clin Mol Hepatol, 2023, 29( Suppl): S123- S135. DOI: 10.3350/cmh.2022.0357. [21] MA YN, LIU JC. Research progress in the noninvasive quantitative diagnosis of hepatic steatosis using controlled attenuation parameters[J]. Chin J Gastroenterol Hepatol, 2020, 29( 11): 1309- 1312. DOI: 10.3969/j.issn.1006-5709.2020.11.023.马亚楠, 刘近春. 受控衰减参数无创定量诊断肝脂肪变性的研究进展[J]. 胃肠病学和肝病学杂志, 2020, 29( 11): 1309- 1312. DOI: 10.3969/j.issn.1006-5709.2020.11.023. -



 PDF下载 ( 1052 KB)
PDF下载 ( 1052 KB)

 下载:
下载: