Clinical value of the measurement of intra-abdominal pressure, C-reactive protein, and procalcitonin in patients with acute pancreatitis in late pregnancy
-
摘要:
目的探讨检测腹内压(IAP)、C反应蛋白(CRP)、降钙素原(PCT)在妊娠晚期急性胰腺炎中的临床价值。方法选取2008年9月-2018年9月于南华大学附属第一医院妇产科和肝胆外科住院的妊娠晚期(28周以上)急性胰腺炎孕妇80例,其中轻症及中重症急性胰腺炎45例(对照组),重症急性胰腺炎35例(观察组)。收集两组孕妇临床资料,包括IAP、CRP、PCT、胎儿窘迫、新生儿Apgar评分等。计量资料两组间比较采用t检验;计数资料两组间比较采用χ2检验。Pearson相关法检验CRP、PCT、IAP与胰腺炎严重程度,以及与胎儿不良结局(胎儿窘迫、出生时1 min Apgar评分)的相关性。根据受试者工作特征曲线(ROC曲线)计算各项指标诊断准确度最高的临界值,以及该值所对应的敏感度和特异度,评价各项指标对妊娠晚期急性胰腺炎的预判价值。结果观察组CRP[(185. 92±23. 59) mg/L vs (120. 92±20. 02) mg/L]、PCT[(12. 93±3. 16) ng/ml vs (5. 67±1. 65) ng/ml]、IAP[(12. 67±1. 40) mm Hg ...
Abstract:Objective To investigate the clinical value of the measurement of intra-abdominal pressure (IAP) , C-reactive protein (CRP) , and procalcitonin (PCT) in patients with acute pancreatitis in late pregnancy. Methods A total of 80 patients with acute pancreatitis in late pregnancy (≥28 gestational weeks) who were hospitalized in Department of Obstetrics and Gynecology and Department of Hepatobiliary Surgery in The First Affiliated Hospital of Nanhua University from September 2008 to September 2018 were enrolled, and among these patients, 45 with mild or moderately severe acute pancreatitis were enrolled as control group, and 35 with severe acute pancreatitis were enrolled as observation group. Related clinical data were collected, including IAP, CRP, PCT, fetal distress, and neonatal Apgar score. The t-test was used for comparison of continuous data between two groups, and the chi-square test was used for comparison of categorical data between two groups. A Pearson correlation analysis was used to investigate the correlation of CRP, PCT, and IAP with the severity of pancreatitis and poor fetal outcomes (fetal distress and neonatal Apgar score at 1 minute after birth) . The receiver operating characteristic (ROC) curve was used to calculate the optimal cut-off values of these indices for accurate diagnosis and corresponding sensitivity and specificity, in order to evaluate their value in predicting acute pancreatitis in late pregnancy. Results Compared with the control group, the observation group had significantly higher levels of CRP (185. 92 ± 23. 59 mg/L vs 120. 92 ± 20. 02 mg/L, t = 13. 318, P < 0. 001) , PCT (12. 93 ± 3. 16 ng/ml vs 5. 67 ± 1. 65 ng/ml, t = 12. 298, P < 0. 001) , and IAP (12. 67 ± 1. 40 mm Hg vs 5. 77 ± 1. 10 mm Hg, t =23. 858, P < 0. 001) . Compared with the observation group, the control group had a significantly lower incidence rate of fetal distress (6/45vs 15/35, χ2= 8. 864, P = 0. 003) and a significantly higher neonatal 1-minute Apgar score (8. 22 ± 0. 67 vs 5. 97 ± 0. 78, t =-13. 817, P < 0. 001) . The correlation analysis showed that IAP was positively correlated with CRP, PCT, and Ranson score for pancreatitis in late pregnancy (r = 0. 814, 0. 712, and 0. 788, all P < 0. 001) and was negatively correlated with neonatal 1-minute Apgar score (r =-0. 820, P < 0. 001) . CRP had an area under the ROC curve (AUC) of 0. 838 at the optimal cut-off value of 158. 32 mg/L, with a sensitivity of77. 1% and a specificity of 93. 3%; PCT had an AUC of 0. 853 at the optimal cut-off value of 10. 23 ng/L, with a sensitivity of 71. 4%and a specificity of 97. 8%; IAP had an AUC of 0. 903 at the optimal cut-off value of 10. 09 mm Hg, with a sensitivity of 82. 9% and a specificity of 95. 6%. Conclusion The measurement of IAP, CRP, and PCT has a good value in the early prediction of severe acute pancreatitis in pregnancy and can help to determine the severity of pancreatitis in late pregnancy and decide the timing of termination of pregnancy.
-
Key words:
- pancreatitis /
- intra-abdominal hypertension /
- C-reactive protein /
- procalcitonin
-
慢性HBV感染的自然史划分为4个期,即免疫耐受期、免疫清除期、免疫控制期和再活动期[1]。目前,对于处于免疫清除期以及再活动期的慢性乙型肝炎(CHB)患者,各大指南均推荐抗病毒治疗,对于免疫耐受期则不推荐抗病毒治疗,建议长期随访[1-4]。然而,有研究[5-11]表明,10%~49%免疫耐受期CHB (Immune-tolerant CHB,IT-CHB) 患者经肝组织病理学检查证实存在明显的肝脏炎症和/或纤维化,若不积极治疗,发展至肝硬化及肝癌的风险增加。IT-CHB患者是否抗病毒治疗尚存在争议[12-18],而评估肝组织学显著肝脏炎症及纤维化对于抗病毒治疗具有重要意义,肝活检仍然是金标准,但其有创性及不易重复等缺点限制了临床应用。本研究通过分析IT-CHB患者显著肝损伤(≥G2/S2)的高危因素,构建无创的个体化列线图预测模型,旨在为指导IT-CHB抗病毒治疗提供参考依据。
1. 资料和方法
1.1 研究对象
回顾性选取2002年8月—2017年12月在解放军总医院第五医学中心住院的IT-CHB患者。免疫耐受期的诊断标准符合2018年版美国肝病学会CHB指南[2]中的定义。纳入标准:(1)年龄>18岁;(2)HBsAg阳性及HBeAg阳性>1年;(3)ALT水平持续正常(男性35 U/L,女性25 U/L)>1年;(4)HBV DNA>1×106 IU/ml;(5)接受肝活检。排除标准:(1)合并其他病毒感染;(2)其他类型肝脏疾病;(3)失代偿期肝硬化;(4)肝癌或其他恶性肿瘤病史;(5)严重的心脏、肾脏或者其他脏器的原发疾病或精神系统疾病。
1.2 肝组织学检查
采用16G活检针进行超声引导下经皮肝活检,要求肝组织长度≥15 mm,至少包括11个汇管区[19]。由2名经验丰富的病理医师进行双盲法阅片,肝组织炎症分级和纤维化分期标准参照《慢性乙型肝炎防治指南(2015年版)》[20]。显著肝损伤(≥G2/S2)定义为肝组织学存在明显的肝脏炎症(≥G2)或纤维化(≥S2)。
1.3 血清学检测
采用贝克曼库尔特AU5421全自动生化仪检测血清ALT、AST、TBil、PLT等。乙型肝炎血清学标志物采用罗氏E170电化学发光法检测。计算APRI指数和FIB-4指数,APRI = (AST/正常值上限×100)/PLT,FIB-4=(年龄×AST)/(PLT×ALT1/2)[21]。
1.4 伦理学审查
本研究通过解放军总医院第五医学中心伦理委员会审批,批号:2020056D。
1.5 统计学方法
采用SPSS 22.0进行统计分析。正态分布的计量数据以x±s表示,2组间比较采用独立样本t检验;非正态分布数据以M(P25~P75)表示,2组间比较采用Mann- Whitney U检验; 多组比较采用Kruskal-Wallis H检验;计数资料2组间比较采用χ2检验。相关性分析采用Spearman秩相关。通过多因素logistic回归模型进入法筛选显著肝损伤的相关因素,采用R语言(3.6.1)的RMS(Regression Modeling Strategies)程序包构建列线图模型,通过Bootstrap重抽样法对模型进行内部验证,用一致性指数(C-指数)、ROC曲线、校准曲线来评价列线图的区分度及校准度。P<0.05为差异有统计学意义。
2. 结果
2.1 一般资料
共纳入382例IT-CHB患者,其中82例(21.5%)存在显著肝损伤。肝组织炎症活动度分级: G0 29例(7.6%)、G1 301例(78.8%)、G2 50例(13.1%)、G3 2例(0.5%);肝组织纤维化分期: S0 57例(14.9%)、S1 251例(65.7%)、S2 39例(10.2%)、S3 23例(6.0%)、S4 12例(3.1%)。按照是否存在显著肝损伤(≥G2/S2)分为2组,2组年龄、HBV DNA载量、ALT、AST、PLT比较差异均有统计学意义(P值均<0.001)(表 1)。
表 1 患者基线的一般资料指标 总体(n=382) 非显著肝损伤组(n=300) 显著肝损伤组(n=82) 统计值 P值 男性[例(%)] 261(68.3) 201(67.0) 60(73.2) χ2=1.133 0.287 年龄(岁) 33.3±10.2 31.5±9.1 39.9±11.2 t=-7.071 <0.001 年龄段[例(%)] χ2=56.472 <0.001 <30岁 161(42.1) 147(49.0) 14(17.1) 30~39岁 130(34.0) 106(35.3) 24(29.3) 40~49岁 64(16.8) 35(11.7) 29(35.4) ≥50岁 27(7.1) 12(4.0) 15(18.3) 乙型肝炎家族史[例(%)] 221(57.9) 173(57.7) 48(58.5) χ2=0.020 0.888 BMI(kg/m2) 23.2±3.53 23.0±3.4 23.7±3.9 t=-1.021 0.308 HBV DNA(log10IU/ml) 8.4(7.8~8.8) 8.4(8.0~8.8) 7.9(6.9~8.5) Z=-4.924 <0.001 ALT(U/L) 23.0(18.0~28.0) 23.0(18.0~28.0) 25.5(21.0~32.0) Z=-3.693 <0.001 AST(U/L) 23.0(19.0~27.0) 21.0(19.0~26.0) 28.0(23.0~34.0) Z=-6.945 <0.001 TBil(μmol/L) 11.1(8.3~15.3) 10.9(8.3~15.3) 11.5(8.6~15.4) Z=-0.585 0.559 PLT(×109/L) 202(164~234) 208(176~239) 161(137~209) Z=-5.723 <0.001 2.2 年龄与肝组织损伤病理学的关系
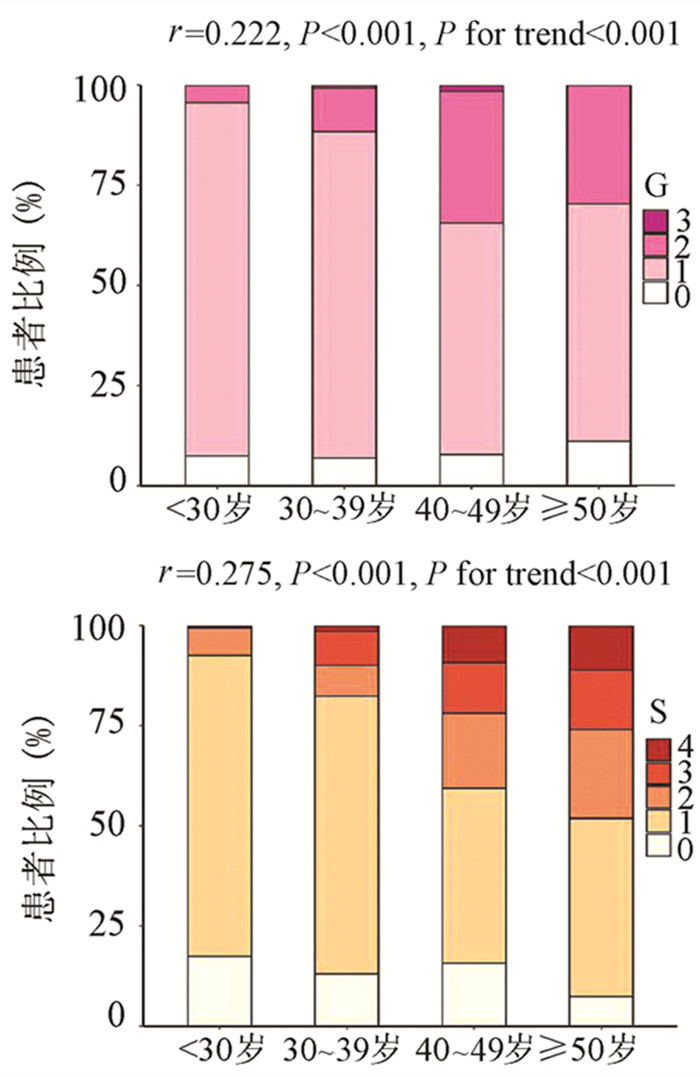
为了评估年龄对IT-CHB显著肝损伤的影响,将患者分为4个年龄段,即<30岁、30~39岁、40~49岁和≥50岁。随年龄的增加,肝组织炎症及纤维化程度逐渐升高,趋势性检验结果表明差异均具有统计学意义(P值均<0.001)。Spearman等级相关分析显示,两者呈正相关(r值分别为0.222、0.275,P值均<0.001)(图 1)。Logistic单因素分析结果显示,较年龄<30岁组,30~39岁组、40~49岁组、年龄≥50岁组出现显著肝损伤的可能性分别为2.4倍(95%CI: 1.175~4.811)、8.7倍(95%CI: 4.165~18.175)、13.1倍(95%CI: 5.146~33.477)(P值均<0.05)。
2.3 HBV DNA与肝组织损伤病理学的关系
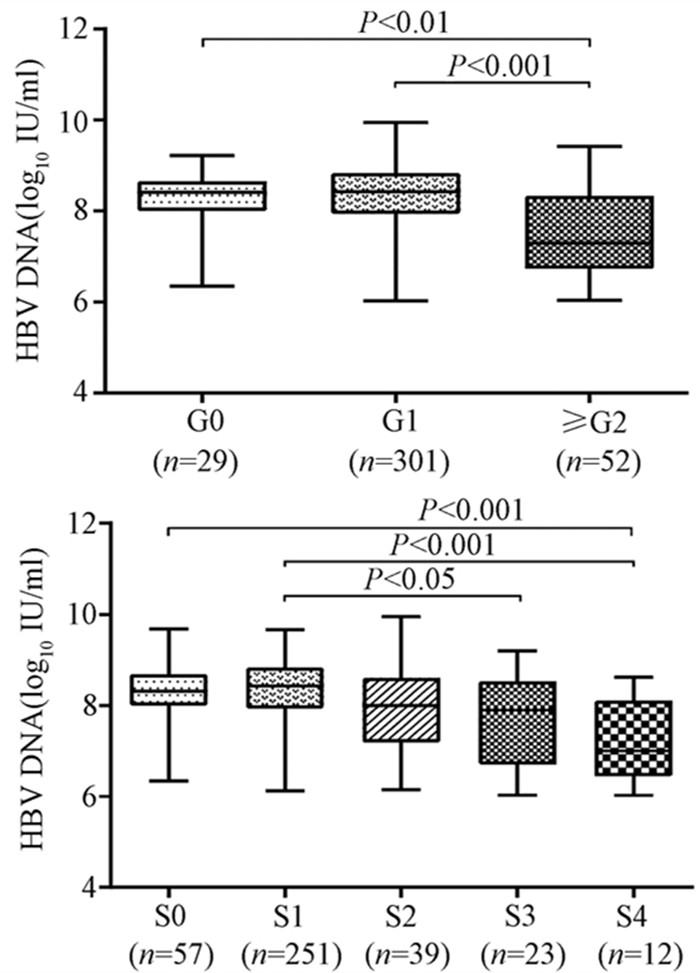
随着肝脏坏死性炎症的加剧,HBV DNA水平呈下降趋势(H=34.161,P<0.001),组间两两比较结果显示:G0组、G1组与≥G2组之间差异有统计学意义(H值分别为80.688、96.903,P值均<0.05),而GO组与G1组无差异(图 2)。伴随肝纤维化的进展,HBV DNA同样表现出下降的趋势(H=26.627,P<0.001),组间两两比较显示,S0与S4、S1与S4、S1与S3之间差异均有统计学意义(H值分别为112.287、125.953、74.354,P值均<0.05)(图 2)。
2.4 显著肝损伤的单因素及多因素分析
为进一步构建无创预测模型,基于无创参数中单因素分析P<0.05的变量作为自变量,以显著肝损伤作为因变量进行logistic回归分析。结果显示,年龄、HBV DNA水平、AST以及PLT是显著肝损伤的独立影响因素(P值均<0.01)(表 2)。
表 2 显著肝损伤的logistic回归分析因素 单因素分析 多因素分析 OR(95%CI) P值 OR(95%CI) P值 年龄 1.084 (1.057~1.113) <0.001 1.074(1.043~1.107) <0.001 HBV DNA 0.437 (0.324~0.589) <0.001 0.442(0.314~0.624) <0.001 ALT 1.076(1.036~1.119) <0.001 1.009(0.959~1.060) 0.736 AST 1.132 (1.089~1.177) <0.001 1.096(1.051~1.142) <0.001 PLT 0.985 (0.98~0.991) <0.001 0.992(0.986~0.998) 0.006 2.5 列线图的制作与检验
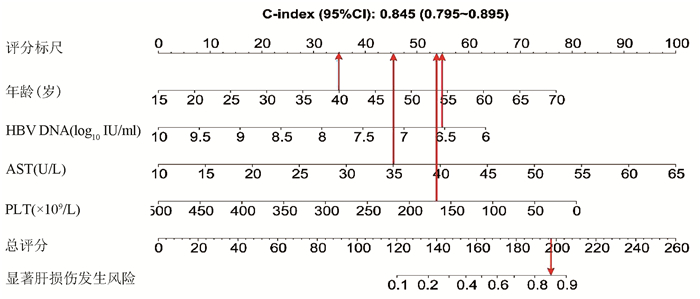
基于logistic回归分析结果,将独立影响因素引入R软件建立预测显著肝损伤的个体化列线图预测模型,并绘制校准曲线和ROC曲线。结果显示,列线图模型预测IT-CHB发生显著肝损伤的C-指数的ROC曲线下面积(AUC)为0.845(95%CI: 0.795~0.895), 明显优于单独使用APRI(AUC=0.781, 95%CI: 0.723~0.840)以及FIB-4(AUC=0.802, 95%CI: 0.746~0.859),差异有统计学意义。校正曲线贴近于理想曲线(对角线),斜率为1.017,Hosmer-Lemeshow拟合优度检验χ2=8.224,P=0.412,提示模型预测值与实际观测值之间的差异无统计学意义,预测模型有良好的校准度。ROC曲线分析显示,列线图的AUC高于APRI、FIB-4,预测IT-CHB患者显著肝损伤的最佳界值为141.4,其敏感度、特异度分别为74.4%、84.7%,差异有统计学意义(P<0.05)(表 3, 图 3)。
表 3 列线图、APRI、FIB-4诊断显著肝损伤的效能比较诊断参数 AUC 95%CI 界值 敏感度(%) 特异度(%) 阳性预测值(%) 阴性预测值(%) Youden指数 列线图 0.845 0.795 ~ 0.895 141.4 74.4 84.7 57.0 92.4 0.59 APRI 0.781 0.723 ~ 0.840 0.338 70.7 77.7 46.4 90.7 0.48 FIB-4 0.802 0.746 ~ 0.859 0.882 78.1 72.3 43.5 92.3 0.50 3. 讨论
全球慢性HBV感染者约2.92亿人,其中约5940万处于免疫耐受期,我国的IT-CHB患者约有1584万例[22]。目前国内外指南对于免疫耐受期的定义尚存在争议[1-4, 23-25],ALT正常上限的标准亦不同, 按照美国肝病学会的标准意味我国IT-CHB患者并非全部处于免疫耐受阶段。单纯用病毒学、ALT水平评估免疫耐受可能存在临床误判,“真正”的免疫耐受需在肝活检基础上进一步确诊,目前多项研究[5-9]表明,10%~49% IT-CHB患者存在明显的肝细胞炎症坏死和肝纤维化病理学改变, 此类患者是否应抗病毒治疗逐渐成为热点问题。
本研究发现IT-CHB患者中21.5%(82/382)存在显著肝损伤,19.4%(74/382)呈显著肝纤维化,其中12例患者(3.1%)处于S4期,提示并不是全部IT-CHB患者均不需要治疗,如何筛选出需要治疗的患者尤为重要。本研究筛选出4个显著肝损伤的高危因素,包括年龄、HBV DNA水平、AST以及PLT,其中AST、PLT作为APRI、FIB-4的参数之一,已被充分证实与肝纤维化程度有关[21, 26]。既往研究[27-28]表明,年龄是CHB患者疾病进展的独立危险因素,尤其年龄>30岁时,HBV相关性肝纤维化、肝硬化、肝癌患者的比例显著增加。Xing等[6]发现年龄是影响肝组织炎症及纤维化的独立预测因子,这一点与本研究结果一致,将IT-CHB患者的年龄分为4个年龄亚组,结果表明,随年龄的增加,肝组织炎症及纤维化程度逐渐升高。关于HBV DNA,我国台湾的大样本研究[29]发现高HBV DNA水平CHB患者进展至肝硬化的风险增加,但其中81.6%(2923/3582) 为HBeAg阴性患者,不属于IT-CHB患者,因此该研究无法准确反映高HBV DNA水平与IT-CHB患者肝纤维化的关系。而本研究发现,IT-CHB患者随着肝脏炎症及纤维化程度的加重,HBV DNA呈下降趋势;并且轻度肝损伤(<G2/S2)的IT- CHB患者中位HBV DNA水平更高(8.4 log10 IU/ml),因此单纯HBV DNA水平并不能准确反映出IT-CHB患者纤维化程度。基于上述分析,本研究建立了无创的列线图模型用于预测IT-CHB患者的显著肝损伤,该模型具有无创的优势,并将多因素分析结果可视化、量化、个体化,具有可重复性,可作为肝活检的有效替代方式。根据该列线图模型,假设某40岁的IT-CHB患者,HBV DNA水平为6.56 log10 IU/ml,AST 35 U/L,PLT 166×109/L,则该患者总得分为188.6分,发生显著肝损伤的概率高达85%,需积极抗病毒治疗。
综上所述,免疫耐受期具有显著肝损伤的患者比例并不少见,基于年龄、HBV DNA、AST、PLT 4个因素构建的列线图模型具有良好的预测准确性,可用于个体化预测IT-CHB患者的显著肝损伤,减少肝活检,为抗病毒的精准治疗提供参考。
-
[1] DUCARME G, MAIRE F, CHATEL P, et al. Acute pancreatitis during pregnancy:A review[J]. J Perinatol, 2014, 34 (2) :87-94. [2] WEI XY. Analysis of clinical characteristics of acute pancreatitis associated with pregnancy[D]. Zhengzhou:Zhengzhou University, 2017. (in Chinese) 魏晓艳.妊娠合并急性胰腺炎的临床特点分析[D].郑州:郑州大学, 2017. [3] YUAN J, MENG F, TANG XW, et al. Clinical features and prognosis of acute pancreatitis in pregnancy[J]. J Clin Hepatol, 2019, 35 (1) :138-142. (in Chinese) 袁景, 孟飞, 汤小伟, 等.妊娠合并急性胰腺炎的临床特征与预后分析[J].临床肝胆病杂志, 2019, 35 (1) :138-142. [4] ZHAO HY, ZHANG Q, WU YZ. High risk factors and prognosis of acute pancreatitis in pregnancy[J]. J Med Postgraduates, 2015, 28 (1) :64-66. (in Chinese) 赵昊云, 张秦, 吴元赭.妊娠合并急性胰腺炎的高危因素及预后评估[J].医学研究生学报, 2015, 28 (1) :64-66. [5] Group of Pancreas Surgery, Chinese Society of Surgery, Chinese Medical Association. Guidelines for the management of acute pancreatitis (2014) [J]. J Clin Hepatol, 2015, 31 (1) :17-20. (in Chinese) 中华医学会外科学分会胰腺外科学组.急性胰腺炎诊治指南 (2014) [J].临床肝胆病杂志, 2015, 31 (1) :17-20. [6] CHUN R, BAGHIRZADA L, TIRUTA C, et al. Measurement of intra-abdominal pressure in term pregnancy:A pilot study[J]. Int J Obstet Anesth, 2012, 21 (2) :135-139. [7] SUN JQ, ZHOU J, ZHENG RJ, et al. The diagnostic value of serum PCT, CRP, LPS for infected pancreatic necrosis in the late course of severe acute pancreatitis[J]. Zhejiang Clin Med J, 2017, 19 (6) :1130-1131. (in Chinese) 孙久庆, 周峻, 郑儒君, 等.血清PCT、CRP、LPS检测对SAP后期感染性胰腺坏死的诊断价值[J].浙江临床医学, 2017, 19 (6) :1130-1131. [8] TAN C, LING Z, HUANG Y, et al. Dysbiosis of intestinal microbiota associated with inflammation involved in the progression of acute pancreatitis[J]. Pancreas, 2015, 44 (6) :868-875. [9] LIU T, ZHAO G. The research progress of laboratory diagnosis for acute pancreatitis[J]. Clin J Med Offic, 2014, 42 (10) :1070-1072, 1075. (in Chinese) 刘婷, 赵冠.急性胰腺炎实验室诊断的研究进展[J].临床军医杂志, 2014, 42 (10) :1070-1072, 1075. [10] LI XP, LI J. Clinical value of serum C-reactive protein, procalcitonin, and lipase in predicting severe acute pancreatitis during pregnancy[J]. J Clin Hepatol, 2016, 32 (10) :1939-1942. (in Chinese) 黎先萍, 李娟.血清CRP、降钙素原及脂肪酶对妊娠合并重症急性胰腺炎的预判价值[J].临床肝胆病杂志, 2016, 32 (10) :1939-1942. [11] van BRUNSCHOT S, SCHUT AJ, BOUWENSE SA, et al. Abdominal compartment syndrome in acute pancreatitis:A systematic review[J]. Pancreas, 2014, 43 (5) :665-674. [12] WANG XY, LIU Z, PAN GD, et al. Diagnosis and treatment of23 severe acute pancreatitis patients with abdominal compartment syndrome[J]. J Chin Physician, 2014, 16 (3) :364-367. (in Chinese) 王晓源, 刘振, 潘光栋, 等.重症急性胰腺炎合并腹腔间隔室综合征23例诊治分析[J].中国医师杂志, 2014, 16 (3) :364-367. [13] SUN L, LI W, SUN F, et al. Intra-abdominal pressure in third trimester pregnancy complicated by acute pancreatitis:An observational study[J]. BMC Pregnancy Childbirth, 2015, 15:223. [14] YE XZ, YAO GF. Value of combined measurement of procalcitonin, C-reactive protein, and serum amyloid A in the diagnosis of sepsis and their influence on prognosis[J]. Clin J Med Offic, 2017, 45 (11) :1191-1193. (in Chinese) 叶先智, 姚桂芬.降钙素原、C-反应蛋白、血清淀粉样蛋白A联合检测对脓毒血症诊断及其预后影响[J].临床军医杂志, 2017, 45 (11) :1191-1193. [15] SUN CW, LI AJ, YANG ZG, et al. Association of serum levels of C-reactive protein and complement C3 with the prognosis of children with acute appendicitis[J]. Trauma Crit Med, 2018, 6 (3) :160-161, 163. (in Chinese) 孙传玮, 李爱军, 杨忠刚, 等.血清C反应蛋白及补体C3水平与急性阑尾炎患儿预后相关性[J].创伤与急危重病医学, 2018, 6 (3) :160-161, 163. [16] ZHAO ZQ, XI Z, YAN PF. Clinical value of combined detection of amylase, lipase and procalcitonin in the diagnosis of children with acute pancreatitis[J]. Chin J Clin Pharmacol Ther, 2017, 22 (11) :1265-1268. (in Chinese) 赵志强, 席錾, 闫鹏飞.血清脂肪酶、血清淀粉酶与血清降钙素原在儿童急性胰腺炎诊断中的意义[J].中国临床药理学与治疗学, 2017, 22 (11) :1265-1268. [17] MUNIGALA S, CONWELL DL, GELRUD A, et al. Heavy smoking is associated with lower age at first episode of acute pancreatitis and a higher risk of recurrence[J]. Pancreas, 2015, 44 (6) :876-881. 期刊类型引用(9)
1. 李晓蓉,姚家喜,施志斌. SAA、GRP78、miR-21-3p与老年急性胰腺炎Ranson和APACHEⅡ评分的关联性. 中国老年学杂志. 2025(05): 1092-1095 .  百度学术
百度学术2. 赵永红,陈爱荣,胡梦茹,王燚鑫,衣桂荣. 急性胰腺炎伴代谢综合征的临床特点和危险因素分析. 现代消化及介入诊疗. 2024(06): 664-669 .  百度学术
百度学术3. 宋小利,陈璐. 大剂量维生素C联合乌司他丁、生长抑素治疗急性胰腺炎的效果及对肝肾功能的影响. 临床医学研究与实践. 2024(28): 39-42 .  百度学术
百度学术4. 卢景涛,彭琼. 非酒精性脂肪性肝病诊断联合BISAP评分对急性胰腺炎严重程度的预测价值. 医学信息. 2023(04): 118-122 .  百度学术
百度学术5. 黄雯雪,陈春洁,孙艳. 急性胰腺炎相关危险因素、严重程度评估及临床护理研究进展. 中国基层医药. 2022(03): 473-476 .  百度学术
百度学术6. 刘国雄,匡桥贵,喻欣荷,刘访,王宇,俞洋,陈杨. 加味大承气汤治疗湿热蕴结型高脂血症性急性胰腺炎的疗效及作用机制. 中国实验方剂学杂志. 2021(05): 91-97 .  百度学术
百度学术7. 王婷婷,何家俊,杨楚婷,李圆浩,陈炜炜,刘军. 非酒精性脂肪性肝病与急性胰腺炎的关系. 临床肝胆病杂志. 2021(03): 729-732 .  本站查看
本站查看8. 赵冬雨,成丽娅,邵伟,马程,沈宏. 胰胆舒胶囊联合乌司他丁治疗急性胰腺炎的临床研究. 现代药物与临床. 2021(04): 712-716 .  百度学术
百度学术9. 黄莹,苗雨,林晚,刘昊,张飞雄,阮继刚. 急性复发性胰腺炎合并代谢综合征的临床特点及预后分析. 宁夏医学杂志. 2021(11): 968-971 .  百度学术
百度学术其他类型引用(7)
-




 PDF下载 ( 2112 KB)
PDF下载 ( 2112 KB)

 下载:
下载:



 百度学术
百度学术
 下载:
下载: