Influence of ideal cardiovascular health behaviors and factors on the onset of primary liver cancer
-
摘要:
目的探究理想心血管健康行为和因素对中国北方地区原发性肝癌的发病有无影响。方法采用前瞻性队列的研究方法,收集2006年7月-2007年6月95 055例参加健康查体的开滦集团在职及离退休职工的体检资料,并对原发性肝癌的发病情况进行随访。根据心血管健康评分(CHS)对研究对象进行分组,其中第一分位组(CHS≤7分) 27 143例,第二分位组(7分<CHS≤9分) 35 488例,第三分位组(9分<CHS≤14分) 32 424例,计算各组的肝癌人年发病率。正态分布的计量资料多组间比较采用单因素方差分析;偏态分布的计量资料多组间比较采用Kruskal-Wallis H检验。计数资料组间比较采用χ2检验。用寿命表法计算各分组原发性肝癌的累积发病率,并用log-rank检验比较组间累积发病率的差异;采用Cox比例风险模型分析理想心血管健康行为和因素对原发性肝癌发病的影响。结果 3组年龄、男性比例、BMI、总胆固醇、空腹血糖、ALT、超敏C反应蛋白水平及饮酒、家庭收入、受教育程度、脂肪肝、癌症家族史、理想吸烟、理想体育锻炼、理想BMI、理想血压、理想总胆固醇、理想血糖、理想饮食比例组...
Abstract:Objective To investigate the influence of ideal cardiovascular health behaviors and factors on the onset of primary liver cancer in northern China. Methods A prospective cohort study was conducted for 95 055 on-the-job or retired employees of Kailuan Group who underwent physical examination from July 2006 to June 2007,and related data were collected. They were followed up to observe the onset of primary liver cancer. According to the cardiovascular health score( CHS),the subjects were divided into first quartile group with 27 143 subjects( CHS≤7),second quartile group with 35 488 subjects( 7 < CHS≤9),and third quartile group with 32 424 subjects( 9 < CHS≤14),and the person-year incidence rate was calculated. A one-way analysis of variance was used for comparison of normally distributed continuous data between multiple groups,and the Kruskal-Wallis H test was used for comparison of continuous data with skewed distribution between multiple groups. The chi-square test was used for comparison of categorical data between groups. The life-table method was used to calculate the cumulative incidence rate of primary liver cancer,and the log-rank test was used for comparison of cumulative incidence rate between groups. The Cox proportional hazards model was used to analyze the influence of ideal cardiovascular health behaviors and factors on the onset of primary liver cancer. Results There were significant differences between the three groups in age,male/female ratio,body mass index,total cholesterol,fasting blood glucose,alanine aminotransferase,hypersensitive C-reactive protein,drinking,family income,educational level,fatty liver disease,family history of cancer,and proportion of subjects with ideal smoking,ideal physical exercise,ideal body mass index,ideal blood pressure,ideal total cholesterol,ideal blood glucose,and ideal diet ratio( all P < 0. 05). The mean follow-up time was 11. 49 ± 1. 86 years,and a total of 387 cases of primary liver cancer were observed,among whom there were 360 male and 27 female patients. The person-year incidence rates of the three groups were 4. 11/10 000 person-years,3. 78/10 000 person-years,and 2. 84/10 000 person-years,respectively. The 10-year cumulative incidence rates of the three groups were 4. 43‰,3. 61‰,and 2. 84‰,respectively,and there was a significant difference in the cumulative incidence rate between the three groups( χ2= 8. 29,P =0. 016). The Cox proportional hazards model showed that after adjustment for confounding factors( age,sex,alanine aminotransferase,hypersensitive C-reactive protein,drinking,family income,educational level,positive HBs Ag,liver cirrhosis,fatty liver disease,and family history of cancer),compared with the first quartile group,the second quartile group had a hazard ratio( HR) of 0. 87( 95% confidence interval [CI]: 0. 67-1. 13) and the third quartile group had an HR of 0. 74( 95% CI: 0. 56-0. 98)( P for trend < 0. 05). Conclusion The higher scores of ideal cardiovascular health behaviors and factors play a protective role in the onset of primary liver cancer,and the risk of primary liver cancer decreases with the increase in cardiovascular score.
-
Key words:
- liver neoplasms /
- healthy lifestyle /
- cohort studies
-
慢性HBV感染的自然史划分为4个期,即免疫耐受期、免疫清除期、免疫控制期和再活动期[1]。目前,对于处于免疫清除期以及再活动期的慢性乙型肝炎(CHB)患者,各大指南均推荐抗病毒治疗,对于免疫耐受期则不推荐抗病毒治疗,建议长期随访[1-4]。然而,有研究[5-11]表明,10%~49%免疫耐受期CHB (Immune-tolerant CHB,IT-CHB) 患者经肝组织病理学检查证实存在明显的肝脏炎症和/或纤维化,若不积极治疗,发展至肝硬化及肝癌的风险增加。IT-CHB患者是否抗病毒治疗尚存在争议[12-18],而评估肝组织学显著肝脏炎症及纤维化对于抗病毒治疗具有重要意义,肝活检仍然是金标准,但其有创性及不易重复等缺点限制了临床应用。本研究通过分析IT-CHB患者显著肝损伤(≥G2/S2)的高危因素,构建无创的个体化列线图预测模型,旨在为指导IT-CHB抗病毒治疗提供参考依据。
1. 资料和方法
1.1 研究对象
回顾性选取2002年8月—2017年12月在解放军总医院第五医学中心住院的IT-CHB患者。免疫耐受期的诊断标准符合2018年版美国肝病学会CHB指南[2]中的定义。纳入标准:(1)年龄>18岁;(2)HBsAg阳性及HBeAg阳性>1年;(3)ALT水平持续正常(男性35 U/L,女性25 U/L)>1年;(4)HBV DNA>1×106 IU/ml;(5)接受肝活检。排除标准:(1)合并其他病毒感染;(2)其他类型肝脏疾病;(3)失代偿期肝硬化;(4)肝癌或其他恶性肿瘤病史;(5)严重的心脏、肾脏或者其他脏器的原发疾病或精神系统疾病。
1.2 肝组织学检查
采用16G活检针进行超声引导下经皮肝活检,要求肝组织长度≥15 mm,至少包括11个汇管区[19]。由2名经验丰富的病理医师进行双盲法阅片,肝组织炎症分级和纤维化分期标准参照《慢性乙型肝炎防治指南(2015年版)》[20]。显著肝损伤(≥G2/S2)定义为肝组织学存在明显的肝脏炎症(≥G2)或纤维化(≥S2)。
1.3 血清学检测
采用贝克曼库尔特AU5421全自动生化仪检测血清ALT、AST、TBil、PLT等。乙型肝炎血清学标志物采用罗氏E170电化学发光法检测。计算APRI指数和FIB-4指数,APRI = (AST/正常值上限×100)/PLT,FIB-4=(年龄×AST)/(PLT×ALT1/2)[21]。
1.4 伦理学审查
本研究通过解放军总医院第五医学中心伦理委员会审批,批号:2020056D。
1.5 统计学方法
采用SPSS 22.0进行统计分析。正态分布的计量数据以x±s表示,2组间比较采用独立样本t检验;非正态分布数据以M(P25~P75)表示,2组间比较采用Mann- Whitney U检验; 多组比较采用Kruskal-Wallis H检验;计数资料2组间比较采用χ2检验。相关性分析采用Spearman秩相关。通过多因素logistic回归模型进入法筛选显著肝损伤的相关因素,采用R语言(3.6.1)的RMS(Regression Modeling Strategies)程序包构建列线图模型,通过Bootstrap重抽样法对模型进行内部验证,用一致性指数(C-指数)、ROC曲线、校准曲线来评价列线图的区分度及校准度。P<0.05为差异有统计学意义。
2. 结果
2.1 一般资料
共纳入382例IT-CHB患者,其中82例(21.5%)存在显著肝损伤。肝组织炎症活动度分级: G0 29例(7.6%)、G1 301例(78.8%)、G2 50例(13.1%)、G3 2例(0.5%);肝组织纤维化分期: S0 57例(14.9%)、S1 251例(65.7%)、S2 39例(10.2%)、S3 23例(6.0%)、S4 12例(3.1%)。按照是否存在显著肝损伤(≥G2/S2)分为2组,2组年龄、HBV DNA载量、ALT、AST、PLT比较差异均有统计学意义(P值均<0.001)(表 1)。
表 1 患者基线的一般资料指标 总体(n=382) 非显著肝损伤组(n=300) 显著肝损伤组(n=82) 统计值 P值 男性[例(%)] 261(68.3) 201(67.0) 60(73.2) χ2=1.133 0.287 年龄(岁) 33.3±10.2 31.5±9.1 39.9±11.2 t=-7.071 <0.001 年龄段[例(%)] χ2=56.472 <0.001 <30岁 161(42.1) 147(49.0) 14(17.1) 30~39岁 130(34.0) 106(35.3) 24(29.3) 40~49岁 64(16.8) 35(11.7) 29(35.4) ≥50岁 27(7.1) 12(4.0) 15(18.3) 乙型肝炎家族史[例(%)] 221(57.9) 173(57.7) 48(58.5) χ2=0.020 0.888 BMI(kg/m2) 23.2±3.53 23.0±3.4 23.7±3.9 t=-1.021 0.308 HBV DNA(log10IU/ml) 8.4(7.8~8.8) 8.4(8.0~8.8) 7.9(6.9~8.5) Z=-4.924 <0.001 ALT(U/L) 23.0(18.0~28.0) 23.0(18.0~28.0) 25.5(21.0~32.0) Z=-3.693 <0.001 AST(U/L) 23.0(19.0~27.0) 21.0(19.0~26.0) 28.0(23.0~34.0) Z=-6.945 <0.001 TBil(μmol/L) 11.1(8.3~15.3) 10.9(8.3~15.3) 11.5(8.6~15.4) Z=-0.585 0.559 PLT(×109/L) 202(164~234) 208(176~239) 161(137~209) Z=-5.723 <0.001 2.2 年龄与肝组织损伤病理学的关系
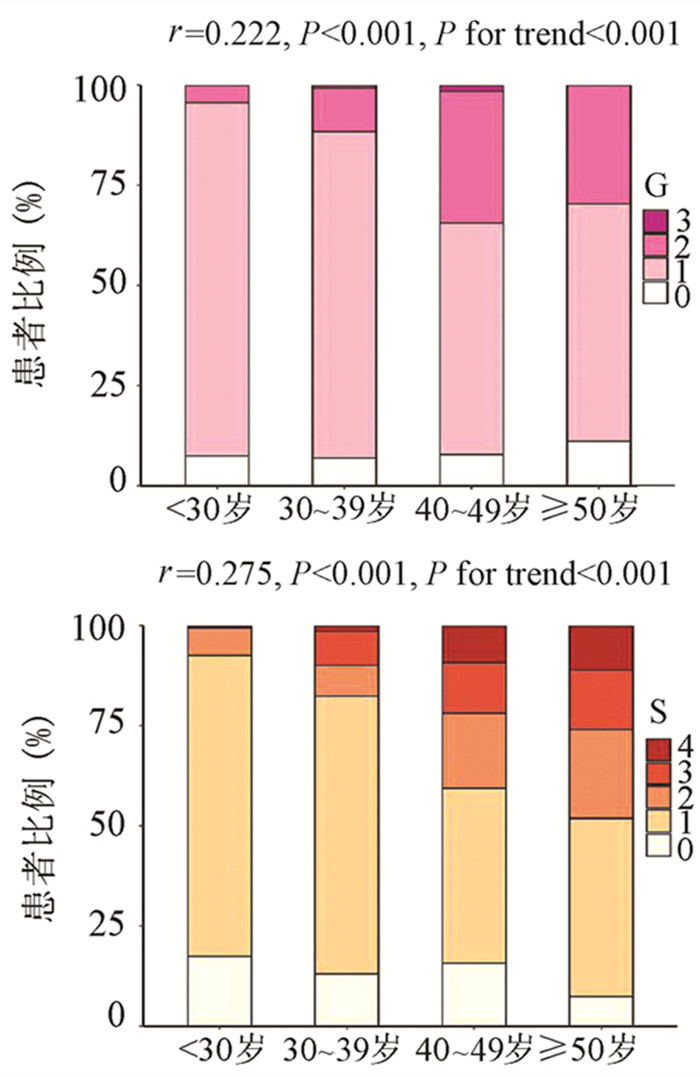
为了评估年龄对IT-CHB显著肝损伤的影响,将患者分为4个年龄段,即<30岁、30~39岁、40~49岁和≥50岁。随年龄的增加,肝组织炎症及纤维化程度逐渐升高,趋势性检验结果表明差异均具有统计学意义(P值均<0.001)。Spearman等级相关分析显示,两者呈正相关(r值分别为0.222、0.275,P值均<0.001)(图 1)。Logistic单因素分析结果显示,较年龄<30岁组,30~39岁组、40~49岁组、年龄≥50岁组出现显著肝损伤的可能性分别为2.4倍(95%CI: 1.175~4.811)、8.7倍(95%CI: 4.165~18.175)、13.1倍(95%CI: 5.146~33.477)(P值均<0.05)。
2.3 HBV DNA与肝组织损伤病理学的关系
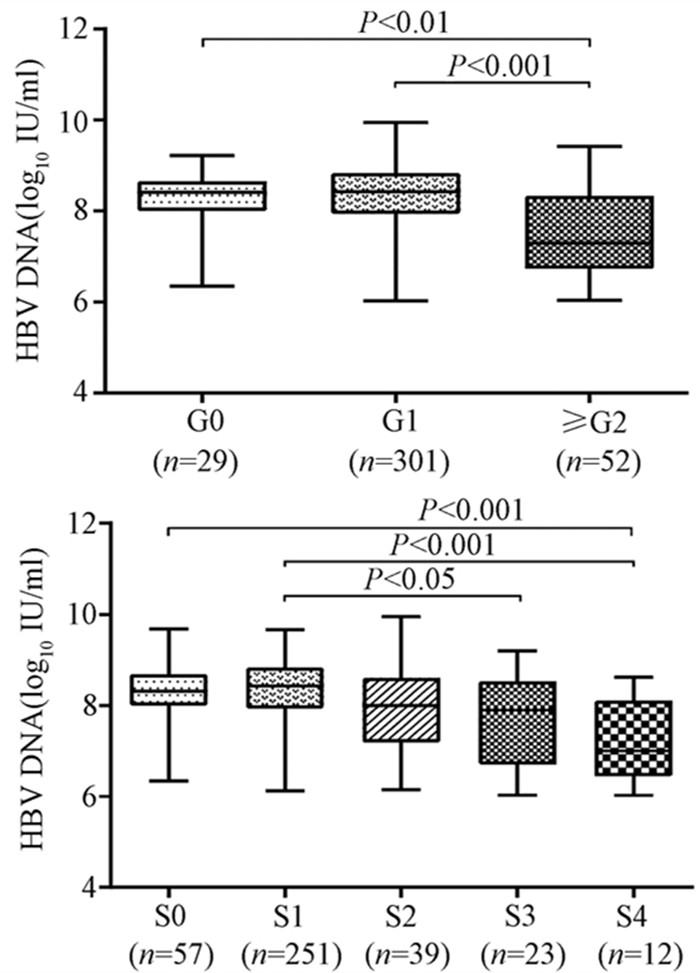
随着肝脏坏死性炎症的加剧,HBV DNA水平呈下降趋势(H=34.161,P<0.001),组间两两比较结果显示:G0组、G1组与≥G2组之间差异有统计学意义(H值分别为80.688、96.903,P值均<0.05),而GO组与G1组无差异(图 2)。伴随肝纤维化的进展,HBV DNA同样表现出下降的趋势(H=26.627,P<0.001),组间两两比较显示,S0与S4、S1与S4、S1与S3之间差异均有统计学意义(H值分别为112.287、125.953、74.354,P值均<0.05)(图 2)。
2.4 显著肝损伤的单因素及多因素分析
为进一步构建无创预测模型,基于无创参数中单因素分析P<0.05的变量作为自变量,以显著肝损伤作为因变量进行logistic回归分析。结果显示,年龄、HBV DNA水平、AST以及PLT是显著肝损伤的独立影响因素(P值均<0.01)(表 2)。
表 2 显著肝损伤的logistic回归分析因素 单因素分析 多因素分析 OR(95%CI) P值 OR(95%CI) P值 年龄 1.084 (1.057~1.113) <0.001 1.074(1.043~1.107) <0.001 HBV DNA 0.437 (0.324~0.589) <0.001 0.442(0.314~0.624) <0.001 ALT 1.076(1.036~1.119) <0.001 1.009(0.959~1.060) 0.736 AST 1.132 (1.089~1.177) <0.001 1.096(1.051~1.142) <0.001 PLT 0.985 (0.98~0.991) <0.001 0.992(0.986~0.998) 0.006 2.5 列线图的制作与检验
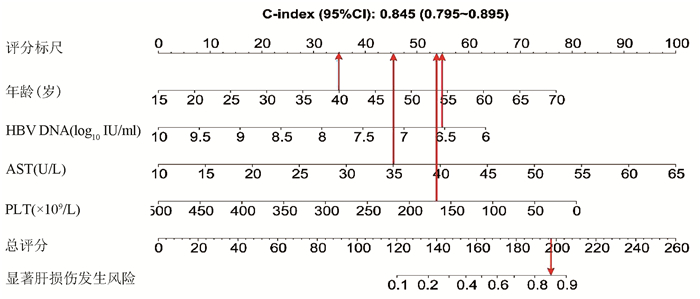
基于logistic回归分析结果,将独立影响因素引入R软件建立预测显著肝损伤的个体化列线图预测模型,并绘制校准曲线和ROC曲线。结果显示,列线图模型预测IT-CHB发生显著肝损伤的C-指数的ROC曲线下面积(AUC)为0.845(95%CI: 0.795~0.895), 明显优于单独使用APRI(AUC=0.781, 95%CI: 0.723~0.840)以及FIB-4(AUC=0.802, 95%CI: 0.746~0.859),差异有统计学意义。校正曲线贴近于理想曲线(对角线),斜率为1.017,Hosmer-Lemeshow拟合优度检验χ2=8.224,P=0.412,提示模型预测值与实际观测值之间的差异无统计学意义,预测模型有良好的校准度。ROC曲线分析显示,列线图的AUC高于APRI、FIB-4,预测IT-CHB患者显著肝损伤的最佳界值为141.4,其敏感度、特异度分别为74.4%、84.7%,差异有统计学意义(P<0.05)(表 3, 图 3)。
表 3 列线图、APRI、FIB-4诊断显著肝损伤的效能比较诊断参数 AUC 95%CI 界值 敏感度(%) 特异度(%) 阳性预测值(%) 阴性预测值(%) Youden指数 列线图 0.845 0.795 ~ 0.895 141.4 74.4 84.7 57.0 92.4 0.59 APRI 0.781 0.723 ~ 0.840 0.338 70.7 77.7 46.4 90.7 0.48 FIB-4 0.802 0.746 ~ 0.859 0.882 78.1 72.3 43.5 92.3 0.50 3. 讨论
全球慢性HBV感染者约2.92亿人,其中约5940万处于免疫耐受期,我国的IT-CHB患者约有1584万例[22]。目前国内外指南对于免疫耐受期的定义尚存在争议[1-4, 23-25],ALT正常上限的标准亦不同, 按照美国肝病学会的标准意味我国IT-CHB患者并非全部处于免疫耐受阶段。单纯用病毒学、ALT水平评估免疫耐受可能存在临床误判,“真正”的免疫耐受需在肝活检基础上进一步确诊,目前多项研究[5-9]表明,10%~49% IT-CHB患者存在明显的肝细胞炎症坏死和肝纤维化病理学改变, 此类患者是否应抗病毒治疗逐渐成为热点问题。
本研究发现IT-CHB患者中21.5%(82/382)存在显著肝损伤,19.4%(74/382)呈显著肝纤维化,其中12例患者(3.1%)处于S4期,提示并不是全部IT-CHB患者均不需要治疗,如何筛选出需要治疗的患者尤为重要。本研究筛选出4个显著肝损伤的高危因素,包括年龄、HBV DNA水平、AST以及PLT,其中AST、PLT作为APRI、FIB-4的参数之一,已被充分证实与肝纤维化程度有关[21, 26]。既往研究[27-28]表明,年龄是CHB患者疾病进展的独立危险因素,尤其年龄>30岁时,HBV相关性肝纤维化、肝硬化、肝癌患者的比例显著增加。Xing等[6]发现年龄是影响肝组织炎症及纤维化的独立预测因子,这一点与本研究结果一致,将IT-CHB患者的年龄分为4个年龄亚组,结果表明,随年龄的增加,肝组织炎症及纤维化程度逐渐升高。关于HBV DNA,我国台湾的大样本研究[29]发现高HBV DNA水平CHB患者进展至肝硬化的风险增加,但其中81.6%(2923/3582) 为HBeAg阴性患者,不属于IT-CHB患者,因此该研究无法准确反映高HBV DNA水平与IT-CHB患者肝纤维化的关系。而本研究发现,IT-CHB患者随着肝脏炎症及纤维化程度的加重,HBV DNA呈下降趋势;并且轻度肝损伤(<G2/S2)的IT- CHB患者中位HBV DNA水平更高(8.4 log10 IU/ml),因此单纯HBV DNA水平并不能准确反映出IT-CHB患者纤维化程度。基于上述分析,本研究建立了无创的列线图模型用于预测IT-CHB患者的显著肝损伤,该模型具有无创的优势,并将多因素分析结果可视化、量化、个体化,具有可重复性,可作为肝活检的有效替代方式。根据该列线图模型,假设某40岁的IT-CHB患者,HBV DNA水平为6.56 log10 IU/ml,AST 35 U/L,PLT 166×109/L,则该患者总得分为188.6分,发生显著肝损伤的概率高达85%,需积极抗病毒治疗。
综上所述,免疫耐受期具有显著肝损伤的患者比例并不少见,基于年龄、HBV DNA、AST、PLT 4个因素构建的列线图模型具有良好的预测准确性,可用于个体化预测IT-CHB患者的显著肝损伤,减少肝活检,为抗病毒的精准治疗提供参考。
-
[1] FERLAY J,SOERJOMATARAM I,DIKSHIT R,et al. Cancer incidence and mortality worldwide:Sources, methods and major patterns in GLOBOCAN 2012[J]. Int J Cancer,2015,136(5):e359-e386. [2] Prevention of Infection Related Cancer(PIRCA)Group,Specialized Committee of Cancer Prevention and Control,Chinese Preventive Medicine Association; Non-communicable&Chronic Disease Control and Prevention Society,Chinese Preventive Medicine Association; Health Communication Society,Chinese Preventive Medicine Association. Strategies of primary prevention of liver cancer in China:Expert Consensus(2018)[J]. J Clin Hepatol,2018,34(10):2090-2097.(in Chinese)中华预防医学会肿瘤预防与控制专业委员会感染相关肿瘤防控学组,中华预防医学会慢病预防与控制分会,中华预防医学会健康传播分会.中国肝癌一级预防专家共识(2018)[J].临床肝胆病杂志,2018,34(10):2090-2097. [3] ZHU NB,ZHOU M,YU CQ,et al. Prevalence of‘healthy lifestyle’in Chinese adults[J]. Chin J Epidemiol,2019,40(2):136-141.(in Chinese)祝楠波,周密,余灿清,等.中国成年人健康生活方式状况分析[J].中华流行病学杂志,2019,40(2):136-141. [4] YANG WS,GAO J,GAO S,et al. A prospective study on cigarette smoking and liver cancer risk:A Meta-analysis[J].Tumor,2010,30(3):247-252.(in Chinese)杨万水,高静,高姗,等.吸烟与肝癌前瞻性研究的荟萃分析[J].肿瘤,2010,30(3):247-252. [5] TURATI F,GALEONE C,ROTA M,et al. Alcohol and liver cancer:A systematic review and meta-analysis of prospective studies[J]. Ann Oncol,2014,25(8):1526-1535. [6] SUNG H,SIEGEL RL,TORRE LA,et al. Global patterns in excess body weight and the associated cancer burden[J]. CA Cancer J Clin,2019,69(2):88-112. [7] MA Y,YANG W,SIMON TG,et al. Dietary patterns and risk of hepatocellular carcinoma among U. S. men and women[J].Hepatology,2019,70(2):577-586. [8] KERR J,ANDERSON C,LIPPMAN SM. Physical activity,sedentary behaviour,diet,and cancer:An update and emerging new evidence[J]. Lancet Oncol,2017,18(8):e457-e471. [9] WILD SH,WALKER JJ,MORLING JR,et al. Cardiovascular disease,cancer,and mortality among people with type 2 diabetes and alcoholic or nonalcoholic fatty liver disease hospital admission[J]. Diabetes Care,2018,41(2):341-347. [10] LIU Y,WARREN ANDERSEN S,WEN W,et al. Prospective cohort study of general and central obesity,weight change trajectory and risk of major cancers among Chinese women[J]. Int J Cancer,2016,139(7):1461-1470. [11] McCORMACK VA,BOFFETTA P. Today’s lifestyles,tomorrow’s cancers:Trends in lifestyle risk factors for cancer in low-and middle-income countries[J]. Ann Oncol,2011,22(11):2349-2357. [12] LLOYD-JONES DM,HONG Y,LABARTHE D,et al. Defining and setting national goals for cardiovascular health promotion and disease reduction:The American Heart Association’s strategic Impact Goal through 2020 and beyond[J]. Circulation,2010,121(4):586-613. [13] WANG YX,WU SL,GAO JS,et al. Relationship between ideal cardiovascular health behaviors and factors with new-onset ischemic stroke[J]. Chin J Hypertension,2012,20(4):342-346.(in Chinese)王艳秀,吴寿岭,高竞生,等.理想心血管健康行为和因素对新发缺血性脑卒中的影响[J].中华高血压杂志,2012,20(4):342-346. [14] ZHANG CF,SHI JH,HUANG Z,et al. Relationship between‘ideal’ cardiovascular behaviors and factors and the incidence of hypertension[J]. Chin J Epidemiol,2014,35(5):494-499.(in Chinese)张彩凤,施继红,黄喆,等.理想心血管健康行为和因素对新发高血压的影响[J].中华流行病学杂志,2014,35(5):494-499. [15] Ministry of Health of the People’s Republic of China. Diagnosis,management,and treatment of hepatocellular carcinoma(V2011)[J]. J Clin Hepatol,2011,27(11):1141-1159.(in Chinese)中华人民共和国卫生部.原发性肝癌诊疗规范(2011年版)[J].临床肝胆病杂志,2011,27(11):1141-1159. [16] HU DY,MA CS. Cardiology practice-standardized treatment(2010)[M]. Beijing:People’s Health Publishing House,2010:10-14.(in Chinese)胡大一,马长生.心脏病学实践2010—规范化治疗[M].北京:人民卫生出版社,2010:10-14. [17] SUN MM,CAO LY,SUN WD,et al. Association of serum high-density lipoprotein cholesterol with new-onset cholelithiasis[J]. J Clin Hepatol,2019,35(8):1745-1750.(in Chinese)孙苗苗,曹立瀛,孙卫东,等.血清高密度脂蛋白胆固醇与新发胆石症的关系[J].临床肝胆病杂志,2019,35(8):1745-1750. [18] SHI JH,HAO YH,WU SL,et al. The prevalence and distribution of ideal cardiovascular health behavior in employees of Kailuan Group cohort[J]. Chin J Cardiol,2012,40(1):62-67.(in Chinese)施继红,郝雁红,吴寿岭,等.开滦研究人群理想心血管健康行为和因素分布调查[J].中华心血管病杂志,2012,40(1):62-67. [19] ZUO TT,ZHENG RS,ZENG HM,et al. Analysis of liver cancer incidence and trend in China[J]. Chin J Oncol,2015,37(9):691-696.(in Chinese)左婷婷,郑荣寿,曾红梅,等.中国肝癌发病状况与趋势分析[J].中华肿瘤杂志,2015,37(9):691-696. [20] World Health Organization. World Cancer Report 2014[EB/OL]. https://www. who. int/cancer/publications/WRC_2014/en/.Accessed December 20,2018. [21] RASMUSSEN-TORVIK LJ,SHAY CM,ABRAMSON JG,et al. Ideal cardiovascular health is inversely associated with incident cancer:The Atherosclerosis Risk In Communities study[J]. Circulation,2013,127(12):1270-1275. [22] ALEKSANDROVA K,PISCHON T,JENAB M,et al. Combined impact of healthy lifestyle factors on colorectal cancer:A large European cohort study[J]. BMC Med,2014,12:168. [23] WANG X,YANG X,LI J,et al. Impact of healthy lifestyles on cancer risk in the Chinese population[J]. Cancer,2019,125(12):2099-2106. [24] Chinese Center of Disease Control and Prevention. Global Adults Tobacco Survey(GATS)China 2010 Country Report[EB/OL]. 2011. https://www. who. int/health-topics/tobacco. [25] LEE YC,COHET C,YANG YC,et al. Meta-analysis of epidemiologic studies on cigarette smoking and liver cancer[J].Int J Epidemiol,2009,38(6):1497-1511. [26] LIU X,BAECKER A,WU M,et al. Interaction between tobacco smoking and hepatitis B virus infection on the risk of liver cancer in a Chinese population[J]. Int J Cancer,2018,142(8):1560-1567. [27] CHUANG SC,LEE YC,HASHIBE M,et al. Interaction between cigarette smoking and hepatitis B and C virus infection on the risk of liver cancer:A meta-analysis[J]. Cancer Epidemiol Biomarkers Prev,2010,19(5):1261-1268. [28] STAPLIN N,HAYNES R,HERRINGTON WG,et al. Smoking and adverse outcomes in patients with CKD:The study of heart and renal protection(SHARP)[J]. Am J Kidney Dis,2016,68(3):371-380. [29] BANKS E,JOSHY G,KORDA RJ,et al. Tobacco smoking and risk of 36 cardiovascular disease subtypes:Fatal and non-fatal outcomes in a large prospective Australian study[J]. BMC Med,2019,17(1):128. [30] YAO KF,MA M,DING GY,et al. Meta-analysis reveals gender difference in the association of liver cancer incidence and excess BMI[J]. Oncotarget,2017,8(42):72959-72971. [31] TIAN Y,JIANG C,WANG M,et al. BMI,leisure-time physical activity,and physical fitness in adults in China:Results from a series of national surveys,2000-14[J]. Lancet Diabetes Endocrinol,2016,4(6):487-497. [32] WANG L,GAO P,ZHANG M,et al. Prevalence and ethnic pattern of diabetes and prediabetes in China in 2013[J]. JAMA,2017,317(24):2515-2523. [33] Investigation and Research Group of National Cooperative Group of Diabetes Research. Investigation report of diabetes among 300thousand people from 14 provinces and cities of China[J]. Chin J Intern Med,1981,20(11):678-683.(in Chinese)全国糖尿病研究协作组调查研究组.全国14省市30万人口中糖尿病调查报告[J].中华内科杂志,1981,20(11):678-683. [34] LIU T,LIU H,JIN PF,et al. Correlation between fasting blood glucose and hepatocarcinogenesis:A multicentre retrospective study(A report of 94 264 cases)[J]. Chin J Dig Surg,2019,18(4):348-357.(in Chinese)刘通,刘海,金鹏飞,等.空腹血糖与肝癌发病关系的多中心回顾性研究(附94264例报告)[J].中华消化外科杂志,2019,18(4):348-357. [35] HAN H,ZHANG T,JIN Z,et al. Blood glucose concentration and risk of liver cancer:Systematic review and meta-analysis of prospective studies[J]. Oncotarget,2017,8(30):50164-50173. 期刊类型引用(9)
1. 李晓蓉,姚家喜,施志斌. SAA、GRP78、miR-21-3p与老年急性胰腺炎Ranson和APACHEⅡ评分的关联性. 中国老年学杂志. 2025(05): 1092-1095 .  百度学术
百度学术2. 赵永红,陈爱荣,胡梦茹,王燚鑫,衣桂荣. 急性胰腺炎伴代谢综合征的临床特点和危险因素分析. 现代消化及介入诊疗. 2024(06): 664-669 .  百度学术
百度学术3. 宋小利,陈璐. 大剂量维生素C联合乌司他丁、生长抑素治疗急性胰腺炎的效果及对肝肾功能的影响. 临床医学研究与实践. 2024(28): 39-42 .  百度学术
百度学术4. 卢景涛,彭琼. 非酒精性脂肪性肝病诊断联合BISAP评分对急性胰腺炎严重程度的预测价值. 医学信息. 2023(04): 118-122 .  百度学术
百度学术5. 黄雯雪,陈春洁,孙艳. 急性胰腺炎相关危险因素、严重程度评估及临床护理研究进展. 中国基层医药. 2022(03): 473-476 .  百度学术
百度学术6. 刘国雄,匡桥贵,喻欣荷,刘访,王宇,俞洋,陈杨. 加味大承气汤治疗湿热蕴结型高脂血症性急性胰腺炎的疗效及作用机制. 中国实验方剂学杂志. 2021(05): 91-97 .  百度学术
百度学术7. 王婷婷,何家俊,杨楚婷,李圆浩,陈炜炜,刘军. 非酒精性脂肪性肝病与急性胰腺炎的关系. 临床肝胆病杂志. 2021(03): 729-732 .  本站查看
本站查看8. 赵冬雨,成丽娅,邵伟,马程,沈宏. 胰胆舒胶囊联合乌司他丁治疗急性胰腺炎的临床研究. 现代药物与临床. 2021(04): 712-716 .  百度学术
百度学术9. 黄莹,苗雨,林晚,刘昊,张飞雄,阮继刚. 急性复发性胰腺炎合并代谢综合征的临床特点及预后分析. 宁夏医学杂志. 2021(11): 968-971 .  百度学术
百度学术其他类型引用(7)
-




 PDF下载 ( 2213 KB)
PDF下载 ( 2213 KB)

 下载:
下载:



 百度学术
百度学术
 下载:
下载: