益生菌在食管胃静脉曲张破裂出血初级预防中的作用
DOI: 10.3969/j.issn.1001-5256.2021.02.017
利益冲突声明:本研究不存在研究者、伦理委员会成员、受试者监护人以及与公开研究成果有关的利益冲突,特此声明。
作者贡献声明:王宪波负责课题设计;张群、牛帅帅参与数据收集,数据分析;张群负责论文撰写及修改;王宪波负责拟定写作思路,指导撰写文章并最后定稿。
Role of probiotics in primary prevention of esophagogastric variceal bleeding
-
摘要:
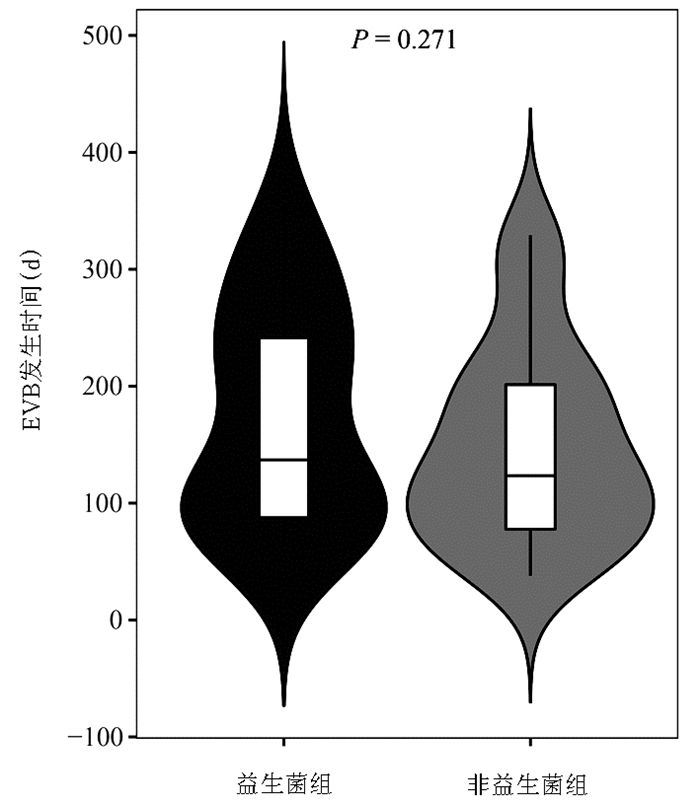
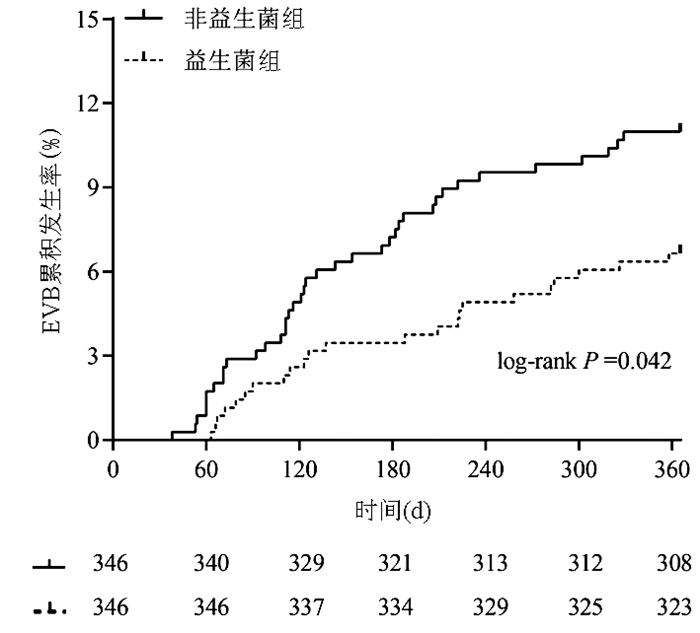
目的 探讨益生菌对肝硬化食管胃静脉曲张患者1年内出血风险的影响。 方法 选取2008年2月—2017年2月于首都医科大学附属北京地坛医院住院且随访时间超过1年的肝硬化食管胃静脉曲张患者692例,其中346例患者在1年的随访期内接受了益生菌治疗(益生菌组)队列,随后采用1:1倾向评分的方法通过校正Child-Pugh分级、静脉曲张分度、红色征为其匹配346例未接受益生菌治疗的患者(非益生菌组)。所有入选患者均按照指南推荐的初级预防策略进行管理,而益生菌队列则在此基础上辅助了益生菌治疗,观察两个队列1年内静脉曲张出血发生率的差异。计量资料两组间比较采用t检验或Mann-Whitney U检验;计数资料两组间比较采用χ2检验;食管胃静脉曲张破裂出血影响因素的筛选采用向后的Cox单因素和多因素回归分析;Kaplan-Meier对两个队列EVB的累积发生率进行分析,并用log-rank进行比较。 结果 益生菌治疗是肝硬化食管胃静脉曲张破裂出血的独立保护因子(校正危险比=0.510,95%CI:0.299~0.870,P=0.013)。共61例患者在1年的随访期内发生了EVB事件,其中益生菌组23例,非益生菌组38例, 益生菌组1年内EVB的累积发生率明显低于非益生菌组(6.6% vs 11.0%,χ2=4.045,P=0.042),且益生菌组基线时至发生出血的中位时间晚于非益生菌组[137.0(85.0~258.0)d vs 123.0(72.5~206.5)d, Z=-1.101, P=0.271]。 结论 益生菌能有效降低肝硬化食管胃静脉曲张患者1年内出血事件的发生率,并有延缓出血事件发生时间的趋势。 Abstract:Objective To investigate the effect of probiotics on the risk of esophagogastric variceal bleeding (EVB) within 1 year in cirrhotic patients with gastroesophageal varices. Methods A retrospective analysis was performed for the clinical data of 692 cirrhotic patients with gastroesophageal varices who were hospitalized in Beijing Ditan Hospital, Capital Medical University, from February 2008 to February 2017 and were followed up for more than 1 year. Among these patients, 346 patients who received probiotics during the 1-year follow-up were enrolled as probiotics cohort (probiotics group), and then, by using the 1:1 propensity score method, 346 patients who did not receive probiotics treatment were enrolled as non-probiotics group after adjustment for Child-Pugh class, degree of varices, and red color sign. All patients were managed according to the primary prevention strategy recommended by related guidelines, and in addition, the patients in the probiotics group were given probiotic therapy. The incidence rate of EVB within 1 year was compared between the two groups. The t-test or the Mann-Whitney U test was used for comparison of continuous data between two groups, and the chi-square test was used for comparison of categorical data between two groups. Univariate and multivariate backward Cox regression analyses were used to screen out the influencing factors for EVB. The Kaplan-Meier analysis was used to investigate the cumulative incidence rate of EVB in both groups, and the log-rank test was used for comparison. Results Probiotic therapy was an independent protective factor against EVB in cirrhotic patients (adjusted hazard ratio=0.510, 95% confidence interval: 0.299-0.870, P=0.013). A total of 61 patients experienced EVB during the 1-year follow-up, with 23 patients in the probiotics group and 38 in the non-probiotics group, and the probiotics group had a significantly lower cumulative incidence rate of EVB within 1 year than the non-probiotics group (6.6% vs 11.0%, χ2=4.045, P=0.042). The probiotics group had a significantly longer median time from baseline to the occurrence of EVB than the non-probiotics group [137.0 (85.0-258.0) days vs 123.0(72.5-206.5) days, Z=-1.101, P=0.271]. Conclusion Probiotics can effectively reduce the incidence rate of EVB within 1 year in cirrhotic patients with gastroesophageal varices, with a tendency to delay the occurrence of bleeding events. -
Key words:
- Liver Cirrhosis /
- Esophageal and Gastric Varices /
- Lactobacillus
-
表 1 两组患者基线特征比较
项目 所有患者
(n=692)益生菌组
(n=346)非益生菌组
(n=346)统计值1) P值1) 年龄(岁) 52.0 (44.0~60.0) 52.0 (44.0~60.0) 52.0 (45.0~59.0) Z=-0.137 0.891 男/女(例) 477/215 240/106 237/109 χ2=0.061 0.805 病因(HBV/HCV/ALD/其他,例) 476/62/79/75 236/29/43/38 240/33/36/37 χ2=0.925 0.819 腹水(有/无,例) 406/286 205/141 201/145 χ2=0.095 0.757 细菌感染(有/无,例) 141/551 74/272 67/279 χ2=0.436 0.509 肝性脑病(有/无,例) 30/662 19/327 11/335 χ2=2.230 0.135 静脉曲张位置(食管/胃/同时,例) 382/25/285 191/11/144 191/14/141 χ2=0.392 0.822 静脉曲张分度(轻/中/重,例) 324/180/188 164/87/95 160/93/93 χ2=0.271 0.873 红色征(有/无,例) 228/464 109/237 119/227 χ2=0.654 0.419 ALT(U/L) 36.6 (24.4~63.6) 36.2 (25.0~62.0) 37.7 (24.1~66.7) Z=-0.663 0.508 AST(U/L) 49.8 (33.1~82.9) 48.7 (32.1~77.0) 51.2 (34.0~90.7) Z=-1.194 0.232 GGT(U/L) 53.3 (29.0~111.2) 52.4 (28.8~109.4) 54.0 (30.3~113.1) Z=-0.376 0.707 TBil(μmol/L) 29.3 (18.8~46.6) 27.6 (17.4~44.8) 30.1 (19.7~49.8) Z=-2.154 0.031 Alb(g/L) 31.9 (27.7~37.0) 32.0 (27.8~36.7) 31.8 (27.7~37.3) Z=-0.123 0.902 WBC(×109/L) 3.3 (2.6~4.5) 3.3 (2.6~4.4) 3.3 (2.5~4.6) Z=-0.435 0.664 RBC(×1012/L) 3.7±0.7 3.7±0.7 3.7±0.7 t=0.236 0.813 NLR 1.9 (1.3~2.8) 1.8 (1.3~2.8) 1.9 (1.3~2.7) Z=-0.421 0.673 Hb(g/L) 120.2 (106.4~133.6) 119.0 (105.8~133.3) 121.0 (108.0~133.7) Z=-1.069 0.285 HCT(%) 35.1 (31.2~39.1) 34.9 (31.2~39.5) 35.5 (31.3~38.9) Z=-0.666 0.505 PLT(×109/L) 61.5 (44.0~85.0) 61.7 (45.0~88.1) 61.5 (43.3~82.9) Z=-0.405 0.685 Cr(μmol/L) 64.0 (55.0~73.7) 64.0 (56.0~74.3) 63.6 (55.0~72.6) Z=-1.467 0.142 Glu(mmol/L) 5.5 (4.9~6.8) 5.5 (4.9~6.8) 5.5 (4.9~7.0) Z=-0.402 0.688 PTA(%) 66.0 (54.5~78.0) 67.0 (55.0~79.0) 64.7 (54.0~77.0) Z=-1.213 0.225 INR 1.1 (1.1~1.4) 1.2 (1.1~1.3) 1.2 (1.1~1.4) Z=-0.098 0.922 脾脏厚度(mm) 48.0 (42.0~55.8) 48.0 (42.0~56.0) 48.0 (42.0~55.3) Z=-0.134 0.894 门静脉宽度(mm) 12.0 (11.0~13.0) 12.0 (11.0~13.0) 12.0 (11.0~13.0) Z=-1.005 0.316 Child-Pugh分级(A/B/C,例) 214/345/133 105/175/66 109/170/67 χ2=0.155 0.926 初级预防 NSBB(有/无,例) 19/673 11/335 8/338 χ2=0.487 0.485 EVL(有/无,例) 86/606 45/301 41/305 χ2=0.212 0.645 注:1)益生菌组与非益生菌组进行比较。ALD,酒精性肝病;NLR,中性粒细胞淋巴细胞比值;Hb,血红蛋白;HCT,红细胞压积;Cr,肌酐;Glu,葡萄糖。 表 2 EVB影响因素Cox回归分析
因素 单因素分析 多因素分析 aHR(95%CI) P值 aHR(95%CI) P值 性别(女性=0;男性=1) 1.890(1.005~3.553) 0.048 病因(HBV=1;HCV=2;ALD=3;其他=4) 0.302(0.151~0.603) 0.001 0.357 (0.183~0.695) 0.002 腹水(无=0;有=1) 2.192(1.224~3.926) 0.008 静脉曲张位置(食管=1;胃=2;食管和胃=3) 1.581(1.211~2.065) 0.001 静脉曲张分度(轻度=1;中度=2;重度=3) 2.111(1.547~2.879) <0.001 红色征(无=0;有=1) 4.832(2.810~8.308) <0.001 3.997(2.260~7.071) <0.001 GGT 1.001(1.000~1.002) 0.013 1.001(1.001~1.002) <0.001 Alb 0.958(0.918~1.000) 0.049 RBC 0.628(0.446~0.883) 0.007 NLR 1.092(1.029~1.159) 0.003 Hb 0.984(0.975~0.993) 0.001 0.984(0.974~0.994) 0.001 HCT 0.950(0.919~0.981) 0.002 脾脏厚度 1.044(1.023~1.066) <0.001 1.034(1.011~1.058) 0.004 益生菌治疗(无=0;有=1) 0.587(0.350~0.986) 0.044 0.510(0.299~0.870) 0.013 -
[1] KUMAR A, SHARMA P, ARORA A. A new prognostic algorithm based on stage of cirrhosis and hvpg to improve risk-stratification after variceal bleeding[J]. Hepatology, 2020.[Epub ahead of print]. [2] HAQ I, TRIPATHI D. Recent advances in the management of variceal bleeding[J]. Gastroenterol Rep (Oxf), 2017, 5(2): 113-126. DOI: 10.1093/gastro/gox007 [3] SHUKLA R, KRAMER J, CAO Y, et al. Risk and predictors of variceal bleeding in cirrhosis patients receiving primary prophylaxis with non-selective beta-blockers[J]. Am J Gastroenterol, 2016, 111(12): 1778-1787. DOI: 10.1038/ajg.2016.440 [4] O'BRIEN J, TRIANTOS C, BURROUGHS AK. Management of varices in patients with cirrhosis[J]. Nat Rev Gastroenterol Hepatol, 2013, 10(7): 402-412. DOI: 10.1038/nrgastro.2013.51 [5] HOLSTER IL, TJWA ET, MOELKER A, et al. Covered transjugular intrahepatic portosystemic shunt versus endoscopic therapy + β-blocker for prevention of variceal rebleeding[J]. Hepatology, 2016, 63(2): 581-589. DOI: 10.1002/hep.28318 [6] Chinese Society of Spleen And Portal Hypertension Surgery, Chinese Society of Surgery, Chinese Medical Association. Expert consensus on diagnosis and treatment of esophagogastric variceal bleeding in cirrhotic portal hypertension (2019 edition)[J]. Chin J Surg, 2019, 57(12): 885-892. (in Chinese)中华医学会外科学分会脾及门静脉高压外科学组. 肝硬化门静脉高压症食管、胃底静脉曲张破裂出血诊治专家共识(2019版)[J]. 中华外科杂志, 2019, 57(12): 885-892. [7] REVERTER E, TANDON P, AUGUSTIN S, et al. A MELD-based model to determine risk of mortality among patients with acute variceal bleeding[J]. Gastroenterology, 2014, 146(2): 412-419. DOI: 10.1053/j.gastro.2013.10.018 [8] BETRAPALLY NS, GILLEVET PM, BAJAJ JS. Gut microbiome and liver disease[J]. Transl Res, 2017, 179: 49-59. DOI: 10.1016/j.trsl.2016.07.005 [9] ALBILLOS A, de LA HERA A, GONZÁLEZ M, et al. Increased lipopolysaccharide binding protein in cirrhotic patients with marked immune and hemodynamic derangement[J]. Hepatology, 2003, 37(1): 208-217. DOI: 10.1053/jhep.2003.50038 [10] QUAN M, XING HC. Research progress on intestinal flora and chronic liver diseases[J/CD]. Chin J Liver Dis (Electronic Version), 2019, 11(3): 26-30. (in Chinese)全敏, 邢卉春. 肠道菌群与慢性肝病相关研究进展[J/CD]. 中国肝脏病杂志(电子版), 2019, 11(3): 26-30. [11] SAAB S, SURAWEERA D, AU J, et al. Probiotics are helpful in hepatic encephalopathy: A meta-analysis of randomized trials[J]. Liver Int, 2016, 36(7): 986-993. DOI: 10.1111/liv.13005 [12] ZHOU LP, LIU SZ. Effect of probiotics in the prevention of spontaneous bacterial peritonitis in patients with cirrhosis[J]. Chin J Mod Drug Appl, 2013, 7(10): 6-7. (in Chinese) DOI: 10.3969/j.issn.1673-9523.2013.10.004周立平, 刘尚忠. 益生菌在肝硬化自发性腹膜炎中的预防效果[J]. 中国现代药物应用, 2013, 7(10): 6-7. DOI: 10.3969/j.issn.1673-9523.2013.10.004 [13] GARCIA-TSAO G, SANYAL AJ, GRACE ND, et al. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis[J]. Hepatology, 2007, 46(3): 922-938. DOI: 10.1002/hep.21907 [14] Chinese Society of Hepatology, Chinese Medical Association; Chinese Society of Gastroenterology, Chinese Medical Association; Chinese Society of Endoscopy, Chinese Medical Association. Guidelines for the diagnosis and treatment of esophageal and gastric variceal bleeding in cirrhotic portal hypertension[J]. J Clin Hepatol, 2016, 32(2): 203-219. (in Chinese) DOI: 10.3969/j.issn.1001-5256.2016.02.002中华医学会肝病学分会, 中华医学会消化病学分会, 中华医学会内镜学分会. 肝硬化门静脉高压食管胃静脉曲张出血的防治指南[J]. 临床肝胆病杂志, 2016, 32(2): 203-219. DOI: 10.3969/j.issn.1001-5256.2016.02.002 [15] WIEST R, ALBILLOS A, TRAUNER M, et al. Targeting the gut-liver axis in liver disease[J]. J Hepatol, 2017, 67(5): 1084-1103. DOI: 10.1016/j.jhep.2017.05.007 [16] MORATALLA A, GÓMEZ-HURTADO I, SANTACRUZ A, et al. Protective effect of Bifidobacterium pseudocatenulatum CECT7765 against induced bacterial antigen translocation in experimental cirrhosis[J]. Liver Int, 2014, 34(6): 850-858. DOI: 10.1111/liv.12380 [17] CAPLAN MS, MILLER-CATCHPOLE R, KAUP S, et al. Bifidobacterial supplementation reduces the incidence of necrotizing enterocolitis in a neonatal rat model[J]. Gastroenterology, 1999, 117(3): 577-583. DOI: 10.1016/S0016-5085(99)70450-6 [18] RUSELER-van EMBDEN JG, van LIESHOUT LM, GOSSELINK MJ, et al. Inability of Lactobacillus casei strain GG, L. acidophilus, and Bifidobacterium bifidum to degrade intestinal mucus glycoproteins[J]. Scand J Gastroenterol, 1995, 30(7): 675-680. DOI: 10.3109/00365529509096312 [19] SCHIFFRIN EJ, ROCHAT F, LINK-AMSTER H, et al. Immunomodulation of human blood cells following the ingestion of lactic acid bacteria[J]. J Dairy Sci, 1995, 78(3): 491-497. DOI: 10.3168/jds.S0022-0302(95)76659-0 [20] BERNET MF, BRASSART D, NEESER JR, et al. Lactobacillus acidophilus LA 1 binds to cultured human intestinal cell lines and inhibits cell attachment and cell invasion by enterovirulent bacteria[J]. Gut, 1994, 35(4): 483-489. DOI: 10.1136/gut.35.4.483 [21] QUAN M, XING HC. Progress on Lactobacillus and liver diseases[J/CD]. Chin J Exp Clin Infect Dis (Electronic Edition), 2019, 13(6): 467-471. (in Chinese)全敏, 邢卉春. 乳酸杆菌与肝病研究进展[J/CD]. 中华实验和临床感染病杂志(电子版), 2019, 13(6): 467-471. [22] de SANTIS A, FAMULARO G, de SIMONE C. Probiotics for the hemodynamic alterations of patients with liver cirrhosis[J]. Am J Gastroenterol, 2000, 95(1): 323-324. DOI: 10.1111/j.1572-0241.2000.01726.x [23] GUPTA N, KUMAR A, SHARMA P, et al. Effects of the adjunctive probiotic VSL#3 on portal haemodynamics in patients with cirrhosis and large varices: A randomized trial[J]. Liver Int, 2013, 33(8): 1148-1157. DOI: 10.1111/liv.12172 [24] RINCÓN D, VAQUERO J, HERNANDO A, et al. Oral probiotic VSL#3 attenuates the circulatory disturbances of patients with cirrhosis and ascites[J]. Liver Int, 2014, 34(10): 1504-1512. DOI: 10.1111/liv.12539 [25] North Italian Endoscopic Club for the Study and Treatment of Esophageal Varices. Prediction of the first variceal hemorrhage in patients with cirrhosis of the liver and esophageal varices. A prospective multicenter study[J]. N Engl J Med, 1988, 319(15): 983-989. DOI: 10.1056/NEJM198810133191505 -



 PDF下载 ( 1939 KB)
PDF下载 ( 1939 KB)

 下载:
下载: