肝切除术和肝移植术治疗的肝细胞癌患者3年随访结局比较
DOI: 10.3969/j.issn.1001-5256.2021.02.019
Three-year follow-up outcomes of hepatocellular carcinoma patients undergoing liver resection versus liver transplantation
-
摘要:
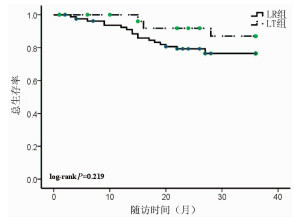
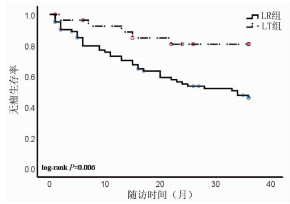
目的 比较肝切除术(LR)和肝移植术(LT)两种方法治疗的肝细胞癌(HCC)患者3年的随访结局。 方法 回顾性分析2009年3月—2014年3月于首都医科大学附属北京佑安医院接受手术治疗的171例HCC患者临床资料,根据治疗方法分为LR组(n=83)和LT组(n=88),比较两组患者的临床资料差异。分类资料组间比较使用χ2检验。采用Kaplan-Meier生存曲线和log-rank检验分析两组之间无瘤生存期和总生存期的差异;用Cox比例风险模型分别对无瘤生存期和总生存期进行单因素和多因素分析。 结果 与LR组对比,LT组的单发肿瘤比例(45.78% vs 85.23%)、直径<3 cm的肿瘤比例(15.66% vs 67.05%)、高Child-Pugh分期比例(9.64% vs 26.14%)明显偏高,LT组的肿瘤复发率明显偏低(48.19% vs 32.95%),且差异具有统计学意义(χ2值分别为29.649、46.383、7.833、4.121,P值分别为<0.001、<0.001、0.005、0.042);LR治疗患者的无瘤生存率是46.02%,而LT治疗患者的无瘤生存率为80.71%,两者比较具有统计学差异(P=0.006);LR治疗患者的总生存率是76.44%,而LT治疗患者的总生存率为86.99%,差异无统计学意义(P=0.219);Cox单因素和多因素分析均显示治疗方法是无瘤生存期的独立危险因素[RR(95% CI)分别为3.383(1.334~8.579)、0.239(0.093~0.612), P值均<0.05],而治疗方法对于总生存期的预测未达到统计学差异(P=0.232)。 结论 LT更倾向于选择肝功能储备较差的早期肝癌患者,3年无瘤生存率较好。 Abstract:Objective To investigate the three-year follow-up outcomes of hepatocellular carcinoma patients undergoing liver resection (LR) versus liver transplantation (LT). Methods A retrospective analysis was performed for 171 patients with hepatocellular carcinoma who underwent surgical treatment in Beijing YouAn Hospital, Capital Medical University, from March 2009 to March 2014, and according to the treatment method, they were divided into LR group(n=83) and LT group(n=88). Related clinical data were compared between the two groups. The chi-square test was used for comparison of categorical data between two groups; the Kaplan-Meier survival curve and the log-rank test were used for comparison of disease-free survival and overall survival between two groups, and the Cox proportional hazards model was used for the univariate and multivariate analyses of disease-free survival and overall survival. Results Compared with the LR group, the LT group had a significantly higher proportion of patients with single tumor [45.78% (38/83) vs 85.23% (75/88), χ2=29.649, P < 0.001], tumor size < 3 cm [15.66% (13/83) vs 67.05% (59/88), χ2=46.383, P < 0.001], or high Child-Pugh class [9.64% (8/83) vs 26.14% (23/88), χ2=7.833, P=0.005] and a significantly lower recurrence rate of tumor [48.19%(40/83) vs 32.95%(29/88), χ2=4.121, P=0.042]. There was a significant difference in disease-free survival rate between the LR group and the LT group (46.02% vs 80.71%, P=0.006); the LT group had a higher overall survival rate than the LR group (86.99% vs 76.44%, P=0.219). Both univariate and multivariate analyses showed that treatment method was an independent risk factor for disease-free survival (risk ratio [RR] =3.383, 95% confidence interval[CI]: 1.334-8.579;RR=0.239, 95%CI:0.093-0.612, both P < 0.05), but the prediction of overall survival by treatment method did not reach statistical significance(P=0.232). Conclusion LT is recommended for patients with early-stage hepatocellular carcinoma and can achieve a satisfactory three-year disease-free survival rate. -
Key words:
- Carcinoma, Hepatocellular /
- Hepatectomy /
- Liver Transplantation /
- Follow-Up Studies
-
急性胰腺炎(AP)是临床常见急症之一,病死率较高,近年来,高脂血症已成为引起AP的第二大常见病因[1-2],与胆源性胰腺炎相比,高甘油三酯血症性急性胰腺炎(hypertriglyceridemia acute pancreatitis,HTGAP)患者趋向年轻化,重症化倾向更明显,并发症多并且病死率高[3]。为了更好地判断AP的严重程度及预后,国内外提出了许多评分系统,但少有研究对HTGAP的严重程度进行相对全面的比较。本研究回顾性分析HTGAP患者的临床资料,探讨五种评分系统对HTGAP病情和预后的预测价值。
1. 资料与方法
1.1 研究对象
本研究收集了宁夏医科大学总医院2016年1月— 2022年1月收治的HTGAP患者。纳入标准:(1)AP诊断标准符合2019年发布的中国急性胰腺炎诊治指南[4];(2) HTGAP诊断标准为血甘油三酯(TG)>11.3 mmol/L,或血TG水平在5.56~11.3 mmol/L且血清呈乳糜状。排除其他如酒精性、自身免疫性、胆源性、药物性等病因所致的AP。
1.2 研究方法
收集患者的临床病历资料,记录如下信息。(1)一般资料:年龄、性别、BMI等;(2)既往史、个人史、合并症、药物服用史等;(3)入院24 h实验室检查结果;(4)根据患者入院24 h内的病历资料进行HAPS评分、BISAP评分和APACHE-Ⅱ评分,根据48 h内的病历资料进行Ranson评分,根据患者临床资料进行PASS评分,进而根据患者病历资料评估病情严重程度及预后[5],每项指标均选择最为异常的数据进行评分。
1.3 统计学方法
采用SPSS 24.0软件对数据进行统计学分析。符合正态分布的计量资料以x±s表示,组间比较采用单因素方差分析;偏态资料以M(P25~P75)表示,三组间比较采用Kruskal-Wallis H秩和检验。计数资料组间比较采用χ2检验。并绘制受试者工作特征曲线(ROC曲线),计算敏感度、特异度、约登指数、95%CI、标准误,以最大约登指数对应的值为临界值(cut-off值),比较指标的ROC曲线下面积(AUC)。P<0.05为差异有统计学意义。
2. 结果
2.1 一般情况
共收集300例患者,其中男247例,女53例,年龄19~70岁,平均(36.8±8.7)岁。根据患者病情程度分为轻症急性胰腺炎(MAP)、中度重症急性胰腺炎(MSAP)和重症急性胰腺炎(SAP),三组患者分别占比为66.3%(199例)、16.1%(48例)和17.6%(53例),经比较三组间性别、年龄、BMI等基线资料差异均无统计学意义,对入院患者的生命体征进行比较,结果提示SAP组和MSAP患者呼吸频率明显高于MAP组,差异均有统计学意义(P值均<0.01),但三组患者心率差异无统计学意义;其次,本研究针对三组患者的个人史(吸烟史、饮酒史)、既往药物服用史、合并症(脂肪肝、代谢综合征及腹腔积液)进行比较,差异均无统计学意义,但经比较,SAP组患者合并呼吸衰竭、SIRS、代谢性酸中毒、脓毒症、MODS及胸腔积液的比例明显升高,且差异均有统计学意义(P值均<0.01)(表 1)。
表 1 3组患者一般情况比较Table 1. Comparison of the general information among the three groups指标 MAP(n=199) MSAP(n=48) SAP(n=53) 统计值 P值 年龄(岁) 35.0(30.0~40.0) 37.0(29.5~45.0) 36.0(31.3~42.8) χ2=2.518 0.284 BMI(kg/m2) 26.29(23.86~29.27) 27.34(25.47~28.52) 26.74(24.13~29.42) χ2=2.180 0.336 呼吸(次/min) 20(20~21) 21(20~21) 21(20~21) χ2=15.989 <0.001 心率(次/min) 26.74±4.48 26.50±4.46 36.21±8.61 F=0.608 0.545 性别[例(%)] χ2=1.263 0.540 男 167(83.9) 36(75.0) 44(83.0) 女 32(16.1) 12(25.0) 9(17.0) 吸烟[例(%)] 93(46.7) 23(47.9) 20(37.7) χ2=2.906 0.241 饮酒[例(%)] 80(40.2) 23(47.9) 21(39.6) χ2=2.180 0.349 药物服用史[例(%)] 39(19.6) 5(10.4) 13(24.5) χ2=2.531 0.286 合并脂肪肝[例(%)] 145(72.9) 38(79.2) 38(71.7) χ2=3.701 0.160 合并糖尿病[例(%)] 57(28.6) 16(33.3) 27(50.9) χ2=7.507 0.024 合并呼吸衰竭[例(%)] 0(0.0) 1(2.1) 4(7.5) χ2=11.241 0.002 合并高血压病[例(%)] 19(9.5) 5(10.4) 6(11.3) χ2=0.300 0.880 合并代谢性酸中毒[例(%)] 0(0.0) 1(2.1) 4(7.5) χ2=11.241 0.002 合并SIRS[例(%)] 0(0.0) 0(0.0) 4(7.5) χ2=11.139 0.002 合并脓毒症[例(%)] 0(0.0) 0(0.0) 4(7.5) χ2=11.139 0.002 合并MODS[例(%)] 0(0.0) 0(0.0) 4(7.5) χ2=11.139 0.002 合并胸腔积液[例(%)] 1(0.5) 3(6.3) 8(15.1) χ2=19.961 <0.001 合并腹腔积液[例(%)] 2(1.0) 0(0.0) 2(3.8) χ2=2.331 0.265 代谢综合征[例(%)] 5(2.5) 2(4.2) 1(1.9) χ2=0.958 0.749 注:SIRS,全身炎症反应综合征;MODS,多器官功能障碍综合征。 2.2 临床资料比较
本研究回顾性分析患者入院24 h的实验室检查资料,根据统计分析结果提示三组间白细胞计数(WBC)、中性粒细胞绝对值(NEUT#)、D-二聚体(D-dimer)、国际标准化比值(INR)、凝血酶原时间(PT)、空腹血糖(GLU)、血钙(Ca)、血尿素(BUN)、白蛋白(Alb)、乳酸脱氢酶(LDH)、血淀粉酶(AMY)、血脂肪酶(LIP)、C反应蛋白(CRP)、淋巴细胞绝对值(LYM) 差异均有统计学意义(P值均<0.05),提示上述指标为重症HTGAP发生的危险因素(表 2)。
表 2 三组患者实验室检验结果比较Table 2. Comparison of laboratory results among the three groups指标 MAP(n=199) MSAP(n=48) SAP(n=53) 统计值 P值 WBC(×109/L) 110.41±18.41 20.78±1.09 22.05±3.69 F=9.424 <0.001 NEUT#(%) 100.44±74.12 20.90±2.36 20.61±1.97 F=10.758 <0.001 LYM(×109/L) 1.520(1.180~2.210) 1.410(1.115~1.920) 1.250(0.800~1.620) χ2=11.328 0.003 MXD(×109/L) 0.705(0.520~0.900) 0.700(0.570~1.000) 0.690(0.553~0.983) χ2=1.486 0.476 PTL(×109/L) 7.35±0.09 105.09±15.74 110.41±18.42 F=1.544 0.215 HCT(%) 45.70(42.80~48.40) 46.70(43.30~49.20) 46.95(41.55~50.60) χ2=1.959 0.376 D-dimer(μg/mL) 0.30(0.20~0.64) 0.32(0.20~0.76) 0.82(0.34~1.96) χ2=25.235 <0.001 PT(s) 11.00(10.00~11.00) 11.20(10.15~11.75) 11.80(10.80~13.00) χ2=19.045 <0.001 INR 0.95(0.89~1.00) 0.960(0.865~1.025) 1.02(0.94~1.12) χ2=25.617 <0.001 GLU(mmol/L) 8.235(6.190~12.163) 9.440(6.895~14.325) 12.770(9.325~17.588) χ2=27.509 <0.001 Ca(mmol/L) 2.310(2.210~2.390) 2.250(2.090~2.360) 2.060(1.785~2.218) χ2=45.766 <0.001 K(mmol/L) 4.165(3.948~4.445) 4.210(3.910~4.350) 4.150(3.905~4.810) χ2=0.613 0.736 BUN(mmol/L) 4.275(3.450~5.393) 4.320(3.645~5.285) 5.390(3.915~6.635) χ2=11.603 0.003 CREA(μmol/L) 61.900(54.100~71.300) 58.600(51.350~68.950) 62.000(50.025~83.750) χ2=2.224 0.329 UA(μmol/L) 405.50(346.75~484.25) 375.00(329.50~480.50) 414.00(307.00~493.00) χ2=0.516 0.773 Alb(g/L) 43.850(40.780~46.930) 42.800(39.500~46.900) 38.700(34.350~43.025) χ2=24.657 <0.001 LDH(U/L) 531.00(432.25~633.25) 659.00(513.50~819.00) 780.00(480.75~1 268.75) χ2=39.743 <0.001 TC(mmol/L) 6.880(5.770~8.520) 7.460(6.200~10.425) 7.000(6.268~9.540) χ2=2.885 0.236 TG(mmol/L) 12.635(10.770~21.683) 11.860(11.850~24.975) 13.910(8.503~27.740) χ2=0.669 0.716 AMY(U/L) 196.00(90.75~358.00) 292.00(140.50~440.00) 411.00(190.00~607.50) χ2=17.024 <0.001 LIP(U/L) 1 161.5(434.0~3 641.0) 922.0(554.0~3 109.5) 2 283.0(1 016.0~5 589.0) χ2=9.880 0.007 CRP(mg/L) 89.00(45.00~136.00) 136.00(79.75~273.75) 154.50(90.00~255.50) χ2=28.317 <0.001 2.3 五种评分系统及临床结局比较
本研究结果显示,三组间PASS评分、Ranson评分、APACHE-Ⅱ评分和BISAP评分系统差异均有统计学意义(P值均<0.01);对三组患者的疾病转归进行比较,根据统计分析结果提示三组间住院天数、住院费用、入住ICU率和复发率差异均有统计学意义(P值均<0.05),但三组间死亡率差异均无统计学意义(P值均>0.05)(表 3)。
表 3 三组患者评分系统和疾病转归及预后比较Table 3. Comparison of scoring systems, disease outcome, and prognosis among the three groups of patients指标 MAP(n=199) MSAP(n=48) SAP(n=53) χ2值 P值 PASS评分 90.0(90.0~90.0) 140.0(115.0~140.0) 200.0(152.5~220.0) 219.351 <0.001 Ranson评分 1(1~2) 2(2~2) 2(2~2) 83.084 <0.001 HAPS评分 1(1~1) 1(1~1) 1(0~1) 0.480 0.799 APACHE-Ⅱ评分 1(1~1) 1(1~2) 2(1~2) 43.388 <0.001 BISAP评分 0(0~0) 0(0~0) 0(0~1) 50.785 <0.001 住院天数(d) 7.00(4.00~9.00) 11.00(8.00~14.50) 10.00(6.25~15.75) 48.281 <0.001 住院费用(元) 10 713(7 200~17 224) 17 027(11 800~24 020) 31 189(21 395~47 700) 93.894 <0.001 ICU[例(%)] 0(0.0) 0(0.0) 6(11.3) 17.317 <0.001 死亡[例(%)] 0(0.0) 0(0.0) 1(1.9) 3.662 0.338 复发[例(%)] 91(45.7) 14(29.2) 36(67.9) 11.357 0.003 2.4 五种评分对HTGAP病情严重程度、并发症和死亡的评估
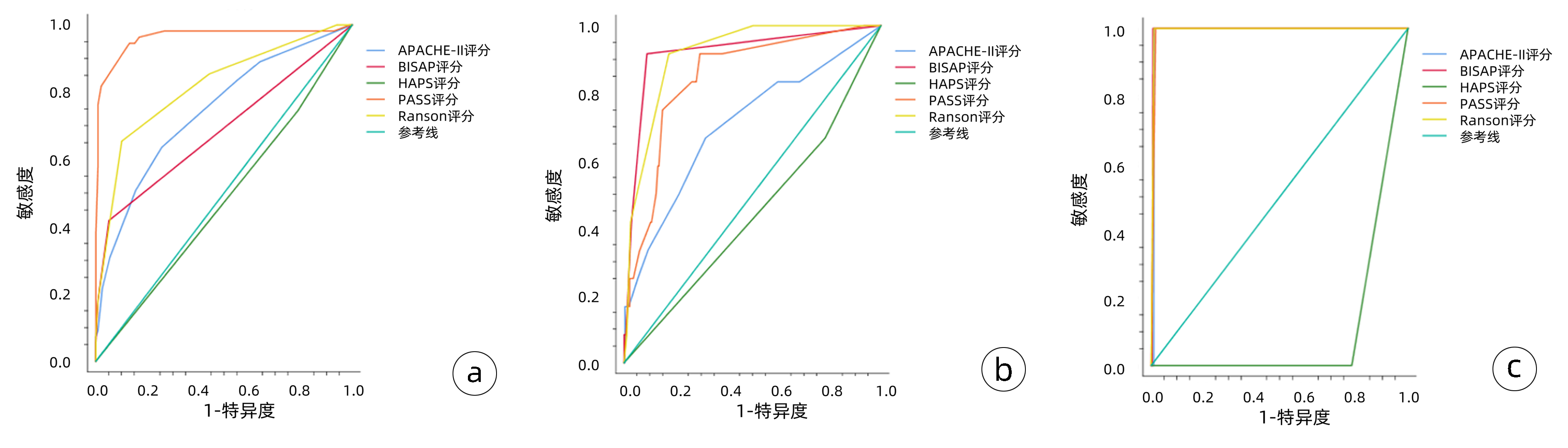
(1) 对病情严重程度(MSAP、SAP) 的预测: PASS评分的敏感度(0.945)和AUC(0.963)高于其他四种评分系统,Ranson评分的敏感度(0.655)和AUC(0.819)次之,HAPS评分AUC仅为0.478;(2)对并发症的预测:对于胸腔积液评估的AUC比较,BISAP评分>Ranson评分>PASS评分>APACHE-Ⅱ评分;(3)对于死亡的预测:BISAP评分和Ranson评分的AUC最高,均为0.995(表 4)。
表 4 五种评分系统对HTGAP患者病情严重程度、并发症和死亡的评估准确性比较Table 4. Comparison of the accuracy of the five scoring systems in evaluating patients' severity of disease, complications, and mortality评分系统及预后指标 AUC P值 敏感度 特异度 阳性预测值 阳性似然比 约登指数 APACHE-Ⅱ MSAP、SAP 0.744 <0.001 0.636 0.743 0.712 2.472 0.379 胸腔积液 0.704 0.016 0.683 0.350 0.678 2.105 0.350 死亡 0.990 <0.001 1.000 0.990 0.990 97.333 0.990 BISAP MSAP、SAP 0.687 <0.001 0.418 0.949 0.892 8.259 0.368 胸腔积液 0.919 <0.001 0.917 0.911 0.912 10.303 0.828 死亡 0.995 <0.001 1.000 0.993 0.993 146.000 0.993 PASS MSAP、SAP 0.963 <0.001 0.945 0.869 0.878 7.288 0.815 胸腔积液 0.846 <0.001 0.917 0.705 0.756 3.103 0.621 死亡 0.991 <0.001 1.000 0.983 0.983 58.400 0.983 Ranson MSAP、SAP 0.819 <0.001 0.655 0.899 0.866 6.464 0.553 胸腔积液 0.916 <0.001 0.917 0.826 0.840 5.257 0.742 死亡 0.995 <0.001 1.000 0.990 0.990 97.333 0.990 HAPS MSAP、SAP 0.418 0.619 0.745 0.211 0.486 0.945 -0.044 胸腔积液 0.442 0.512 0.512 0.217 0.460 0.852 -0.016 死亡 0.110 <0.001 0.000 0.219 0.000 0.000 -0.781 五种评分系统预测AP患者病情严重程度、并发症和死亡的ROC曲线见图 1,图 1a中ROC曲线对五种评分系统预测病情严重程度的准确度进行了比较,其中PASS评分预测病情严重程度的敏感度最高,其次是Ranson评分,HAPS评分对预测病情严重程度无统计学意义。图 1b中ROC曲线对五种评分系统预测并发症的准确度进行了比较,BISAP评分预测并发症的敏感度和特异度最高,其次是Ranson评分,HAPS评分对预测并发症无统计学意义。图 1c中ROC曲线对五种评分系统预测死亡的准确度进行了比较,除外HAPS评分,另外四种评分系统对预测死亡的敏感度、特异度均较高(均>0.90)。
3. 讨论
多个研究[6-7]表明,相较于其他病因所致的AP,HTGAP患者多为年轻人,病情进展更快更重,预后差且复发率高,正因为HTGAP特殊的临床表现,要求临床医师准确并高效的确定疾病的严重程度,对于潜在的重症患者尽早给予特殊的监护措施及治疗方案。目前虽无完美的预测HTGAP病情的工具,但存在一些多因素评分系统(基于临床、实验室、影像学证据)以及单因素评价指标(多为生物标志物),其侧重点和临床价值各不相同[8]。
HTGAP病程具有高度可变的特点, 早期患者可能表现为轻症, 但会迅速发展为危急重症状态, 为了更好地研究、评估和预测疾病发展,2017年国际专家提出了新的胰腺炎活动评分系统(PASS)[9-10],本研究结果显示对于HTGAP病情严重程度的预测: PASS评分的敏感度和AUC均高于其他四种评分系统。既往多数评分系统,大部分聚焦于早期评估HTGAP患者的病情严重程度,PASS评分的提出旨在对患者病程中以12 h为增量进行一次评分,不仅客观评估患者实验室指标,还加入了患者主观感受(如疼痛耐受程度、经口进食耐受程度),从理论上来说更能综合全面评估患者病情[11-12],动态预测不同时间点患者的病情严重程度等能力更优,综上,PASS可能对HTGAP患者的病情预测和干预具有更重要的临床意义,是一项很有前景的定量测量HTGAP患者疾病活动的评分系统。
Ranson评分纳入了11项临床和实验室参数,最初主要用于评估酒精性AP患者的病情。有些研究认为,Ranson评分耗时较长,内容相对繁琐,对临床应用价值不大,但随着对HTGAP发病机制的进一步了解,以及对于HTGAP的规范化治疗,近年来多项临床研究[13-14]证实了Ranson评分系统对于AP的病情严重程度评估的准确性和有效性。本研究发现SAP组的Ranson评分值显著高于其余两组, 其次,Ranson评分对于胸腔积液和死亡的预测能力也较高,这说明采用Ranson评分系统水平能够对HTGAP严重程度及预后进行一定的评价,但不足之处在于第2次评分需在入院48 h后进行,故难以早期预测HTGAP病情的走势。
同多数研究结果一致,BISAP在预测HTGAP严重程度、局部并发症等方面具有较高的准确性,且本研究提示BISAP评分对HTGAP的病情严重程度的预测特异度达94.5%。同时,BISAP评分系统临床数据易获取,操作相对简便,有利于早期指导临床治疗决策[15-17]。因此BISAP评分系统目前仍广泛在临床应用,但该评分系统在是否需要介入或手术干预等方面预测价值有限[18]。
HAPS评分是由Lankisch等经过一项前瞻性研究于2009年提出,该评分将无反跳痛和肌紧张、正常红细胞压积水平和正常血清肌酐水平这3项对非严重病程有最强预测的参数结合起来[8],多数研究提示入院时HAPS评分预测MAP的效能较高[19],但国内外鲜有关于HAPS评分对于HTGAP的大样本评价,本研究结果显示HAPS评分对于HTGAP严重程度的预测AUC仅为0.478,提示HAPS评分对于识别非重症急性胰腺炎有较高的临床价值,但其预测SAP的可靠性较低,对于重症HTGAP的预测价值有待于进一步研究。
本研究存在一定的局限性,单中心研究且样本量有限,回顾性的研究分析数据可能存在偏差,所以目前还需要大样本的、前瞻性、多中心的研究来验证以上评分系统对HTGPA患者病情严重程度及预后的预测作用。
综上所述,对于HTGAP患者,相较于其他四种评分系统,PASS评分可以更准确地评估HTGAP患者的病情严重程度,有望在临床中更好的推广应用。临床医师需要多结合各评分系统的优点,灵活使用每种评分系统的优势,以便及时、有效地评估病情,指导临床医师采取积极的治疗措施,从而降低HTGAP的病死率、改善预后。
-
表 1 肝癌患者的基本资料
指标 例数(n=171) 手术类型 χ2值 P值 LR组(n=83) LT组(n=88) 性别(例) 0.192 0.661 男 142 70 72 女 29 13 16 年龄(例) 0.117 0.732 ≤50岁 95 45 50 >50岁 76 38 38 潜在肝病(例) 2.333 0.311 HBV 153 76 77 HCV 17 6 11 其他 1 1 0 肿瘤位置(例) 1.161 0.281 右叶 119 61 58 非右叶或多叶 52 22 30 肿瘤数目(例) 29.649 <0.001 单发 113 38 75 多发 58 45 13 肿瘤大小(例) 46.383 <0.001 <3 cm 72 13 59 3~5 cm 62 43 19 >5 cm 37 27 10 AFP (例) 3.350 0.187 <20 ng/ml 82 42 40 20~400 ng/ml 52 20 32 >400 ng/ml 37 21 16 TNM分期(例) 0.174 0.677 Ⅰ+Ⅱ 117 57 63 Ⅲ+Ⅳ 54 26 25 BCLC肝癌分期(例) 0.057 0.972 A 87 42 45 B 44 22 22 C 40 19 21 Child-Pugh分级(例) 7.833 0.005 C 140 75 65 B+C 31 8 23 病理分级(例) 2.573 0.276 低分化 29 18 11 中分化 113 52 61 高分化 29 13 16 肿瘤复发(例) 4.121 0.042 否 102 43 59 是 69 40 29 HCC所致死亡(例) 0.937 0.333 否 139 65 74 是 32 18 14 表 2 肝癌患者无瘤生存期和总生存期的单因素分析
指标 无瘤生存期 总生存期 RR 95%CI P值 RR 95%CI P值 性别 男 1.000 1.000 女 0.539 0.213~1.367 0.193 0.474 0.110~2.034 0.315 年龄 ≤50岁 1.000 1.000 >50岁 1.023 0.570~1.838 0.939 0.678 0.281~1.636 0.387 肝病 HBV 1.000 1.000 HCV/其他 0.380 0.092~1.569 0.181 0.872 0.203~3.747 0.854 肿瘤位置 肝右叶 1.000 1.000 其他位置 0.816 0.422~1.581 0.548 0.693 0.254~1.893 0.475 肿瘤数目 单发 1.000 1.000 多发 1.513 0.833~2.751 0.174 1.491 0.628~3.542 0.365 肿瘤大小 <3 cm 1.000 1.000 <3 cm 1.000 1.000 3~5 cm 1.360 0.647~2.860 0.418 2.956 0.890~9.819 0.077 >5 cm 3.877 1.924~7.812 <0.001 5.595 1.721~18.189 0.004 AFP <20 ng/ml 1.000 1.000 20~400 ng/ml 1.862 0.861~4.025 0.114 0.982 1.699~12.123 0.003 >400 ng/ml 3.625 1.804~7.285 <0.001 4.539 1.699~12.123 0.003 TNM分期 Ⅰ-Ⅱ 1.000 1.000 Ⅲ 4.084 2.237~7.455 <0.001 4.985 2.058~12.076 <0.001 BCLC HCC分期 A 1.000 1.000 B 1.778 0.887~3.564 0.003 1.235 0.349~4.378 0.001 C 3.008 1.453~6.230 0.105 0.003 5.566 2.052~15.101 0.001 Child-Pugh分级 A 1.000 1.000 B+C 0.446 0.160~1.245 0.123 1.886 0.731~4.864 0.189 病理分期 低分化 1.000 1.000 中/高分化 0.813 0.378~1.750 0.597 0.524 0.203~1.350 0.181 治疗方法 LR 1.000 1.000 LT 3.383 1.334~8.579 0.010 0.474 0.140~1.610 0.232 -
[1] Bureau of Medical Administration, National Health Commission of the People's Republic of China. Guidelines for diagnosis and treatment of primary liver cancer in China (2019 edition)[J]. J Clin Hepatol, 2020, 36(2): 277-292. (in Chinese) DOI: 10.3969/j.issn.1001-5256.2020.02.007中华人民共和国国家卫生健康委员会医政医管局.原发性肝癌诊疗规范(2019年版)[J].临床肝胆病杂志, 2020, 36(2): 277-292. DOI: 10.3969/j.issn.1001-5256.2020.02.007 [2] YANG JD, HAINAUT P, GORES GJ, et al. A global view of hepatocellular carcinoma: Trends, risk, prevention and management[J]. Nat Rev Gastroenterol Hepatol, 2019, 16(10): 589-604. DOI: 10.1038/s41575-019-0186-y [3] WAN CD, WANG GB. Advances in treatments for primary liver cancer[J]. J Abdominal Surg, 2019, 32(1): 1-6, 22. (in Chinese) http://www.cnki.com.cn/Article/CJFDTotal-FBWK201901001.htm万赤丹, 王国斌.原发性肝癌治疗进展[J].腹部外科, 2019, 32(1): 1-6, 22. http://www.cnki.com.cn/Article/CJFDTotal-FBWK201901001.htm [4] LIU AX, WANG HQ, BO WT, et al. Clinical efficacy and prognostic factors analysis of hepatectomy for hepatocellular carcinoma[J]. Chin J Dig Surg, 2019, 18(4): 368-374. (in Chinese) DOI: 10.3760/cma.j.issn.1673-9752.2019.04.012刘爱祥, 王海清, 薄文滔, 等.肝细胞癌肝切除术的临床疗效及预后因素分析[J].中华消化外科杂志, 2019, 18(4): 368-374. DOI: 10.3760/cma.j.issn.1673-9752.2019.04.012 [5] LU L, QIN LX. Advances and challenges in multimodality surgical therapy for liver cancer[J]. Chin J Gen Surg, 2019, 34(11): 913-915. (in Chinese) http://d.wanfangdata.com.cn/periodical/zhptwk201911001陆录, 钦伦秀.肝癌外科综合治疗的进展与挑战[J].中华普通外科杂志, 2019, 34(11): 913-915. http://d.wanfangdata.com.cn/periodical/zhptwk201911001 [6] AKOAD ME, POMFRET EA. Surgical resection and liver transplantation for hepatocellular carcinoma [J]. Clin Liver Dis, 2015, 19(2): 381-399. DOI: 10.1016/j.cld.2015.01.007 [7] JIAO XL, CHEN Y, LI X, et al. Clinical effect of resection, radiofrequency ablation and transplantation for small hepatocellular carcinoma: Comparative study[J]. Prac J Med Pharm, 2018, 35(3): 193-196. (in Chinese) http://www.cnki.com.cn/Article/CJFDTotal-QEYY201803003.htm矫学黎, 陈燚, 李霞, 等.肝切除、射频消融和肝移植三种方案治疗小肝癌的临床疗效比较[J].实用医药杂志, 2018, 35(3): 193-196. http://www.cnki.com.cn/Article/CJFDTotal-QEYY201803003.htm [8] JIN ZZ, JIN FF, LIU X, et al. The association between coexistence of HBsAg/anti-HBs and risk of hepatocellular carcinoma in patients with chronic hepatitis B[J]. Beijing Med J, 2019, 41(6): 455-459. (in Chinese) http://www.cnki.com.cn/Article/CJFDTotal-BJYX201906005.htm金子铮, 金方方, 刘新, 等.慢性乙肝患者HBsAg/抗-HBs共存与肝癌发生风险的研究[J].北京医学, 2019, 41(6): 455-459. http://www.cnki.com.cn/Article/CJFDTotal-BJYX201906005.htm [9] SHEN JY, LI C, WEN TF, et al. Liver transplantation versus surgical resection for HCC meeting the Milan criteria: A propensity score analysis [J]. Medicine (Baltimore), 2016, 95(52): e5756. DOI: 10.1097/MD.0000000000005756 [10] MENAHEM B, LUBRANO J, DUVOUX C, et al. Liver transplantation versus liver resection for hepatocellular carcinoma in intention to treat: An attempt to perform an ideal meta-analysis[J]. Liver Transpl, 2017, 23(6): 836-844. DOI: 10.1002/lt.24758 [11] PINNA AD, YANG T, MAZZAFERRO V, et al. Liver transplantation and hepatic resection can achieve cure for hepatocellular carcinoma [J]. Ann Surg, 2018, 268(5): 868-875. DOI: 10.1097/SLA.0000000000002889 [12] XIA YJ, JIANG Y, CAI QC, et al. Comparison of efficacies of hepatectomy and liver transplantation for patients with hepatocellular carcinoma fulfilling the Milan criteria[J]. Chin J Dig Surg, 2012, 11(6): 526-529.(in Chinese) DOI: 10.3760/cma.j.issn.1673-9752.2012.06.009夏玉健, 江艺, 蔡秋程, 等.肝切除和肝移植治疗符合米兰标准肝癌患者的疗效比较[J].中华消化外科杂志, 2012, 11(6): 526-529. DOI: 10.3760/cma.j.issn.1673-9752.2012.06.009 [13] WANG ZS, LI N, LIN DD, et al. Research advances in the association between quality of life and osteoporosis in patients after liver transplantation[J]. Beijing Med J, 2015, 37(9): 876-878. (in Chinese) http://www.cnki.com.cn/Article/CJFDTotal-BJYX201509021.htm王振顺, 李宁, 林栋栋, 等.肝移植术后患者生存质量与骨质疏松关系的研究进展[J].北京医学, 2015, 37(9): 876-878. http://www.cnki.com.cn/Article/CJFDTotal-BJYX201509021.htm [14] CHEN QY, JIANG SF, XIA RP, et al. Research progress on immunosuppressants and new drugs for liver transplantation[J]. Organ Transplantation, 2020, 11(6): 663-670. (in Chinese) DOI: 10.3969/j.issn.1674-7445.2020.06.003陈泉余, 蒋师放, 夏仁培, 等.肝移植临床免疫抑制剂及新药研究进展[J].器官移植, 2020, 11(6): 663-670. DOI: 10.3969/j.issn.1674-7445.2020.06.003 -




 PDF下载 ( 2202 KB)
PDF下载 ( 2202 KB)

 下载:
下载:

 下载:
下载: