非肥胖型非酒精性脂肪性肝病的病因及治疗进展
DOI: 10.3969/j.issn.1001-5256.2021.02.043
作者贡献声明:李洋洋负责参与收集数据,资料分析,撰写论文,修改论文;谢正元负责拟定写作思路,指导撰写文章并最后定稿。
Advances in the etiology and treatment of non-obese nonalcoholic fatty liver disease
-
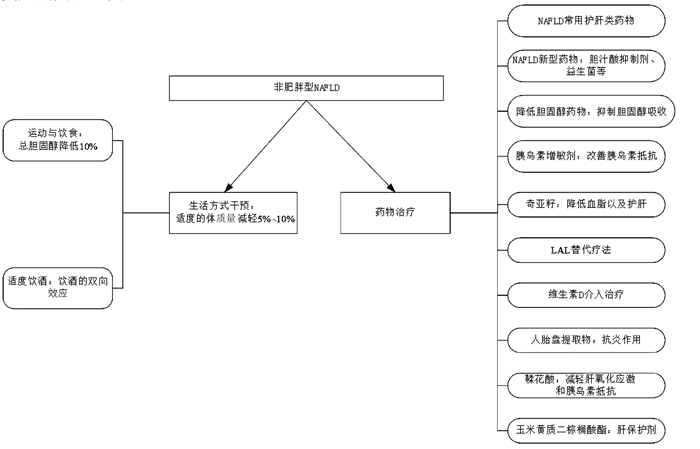
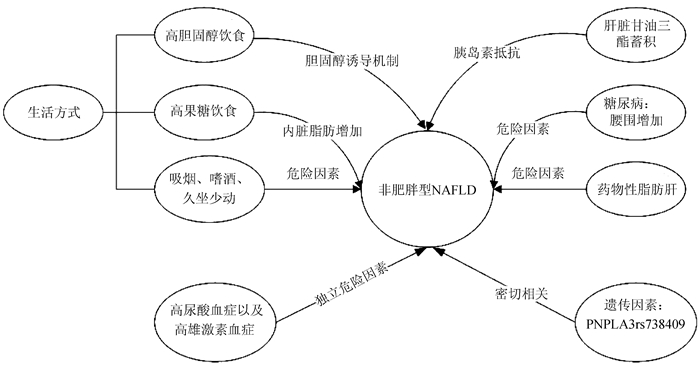
摘要: 随着非酒精性脂肪性肝病(NAFLD)在非肥胖人群中的流行,越来越多的研究探讨了NAFLD在非肥胖人群中的意义。与肥胖型NAFLD患者相比,非肥胖型NAFLD患者虽缺乏肥胖表型,但仍存在代谢紊乱,其发生代谢性疾病和心血管疾病的风险更大。目前针对非肥胖型NAFLD尚无治疗相关的有效药物,且现有的治疗方式各有优势,但都存在一定的局限性。从非肥胖型NAFLD的病因及治疗进展方面进行综述,为指导非肥胖型NAFLD临床治疗提供参考。Abstract: With the prevalence of nonalcoholic fatty liver disease (NAFLD) in the non-obese population, more and more studies have explored the significance of NAFLD in such population. Compared with the patients with obese NAFLD, the patients with non-obese NAFLD lack the phenotype of obesity, but they still have metabolic disorders and higher risk of metabolic and cardiovascular diseases. At present, there are no effective drugs for the treatment of non-obese NAFLD, and the existing treatment methods have their own advantages and limitations in clinical practice. This article reviews the advances in the etiology and treatment of non-obese NAFLD, in order to provide a reference for guiding the clinical treatment of non-obese NAFLD.
-
Key words:
- Non-alcoholic Fatty Liver Disease /
- Risk Factors /
- Therapeutics /
- Prognosis
-
[1] LONARDO A, NASCIMBENI F, MAURANTONIO M, et al. Nonalcoholic fatty liver disease: Evolving paradigms[J]. World J Gastroenterol, 2017, 23(36): 6571-6592. DOI: 10.3748/wjg.v23.i36.6571 [2] NADERIAN M, KOLAHDOOZAN S, SHARIFI AS, et al. Assessment of lean patients with non-alcoholic fatty liver disease in a middle income country; Prevalence and its association with metabolic disorders: A cross-sectional study[J]. Arch Iran Med, 2017, 20(4): 211-217. [3] ZENG J, YANG RX, SUN C, et al. Prevalence, clinical characteristics, risk factors, and indicators for lean Chinese adults with nonalcoholic fatty liver disease[J]. World J Gastroenterol, 2020, 26(15): 1792-1804. DOI: 10.3748/wjg.v26.i15.1792 [4] YE Q, ZOU B, YEO YH, et al. Global prevalence, incidence, and outcomes of non-obese or lean non-alcoholic fatty liver disease: A systematic review and meta-analysis[J]. Lancet Gastroenterol Hepatol, 2020, 5(8): 739-752. DOI: 10.1016/S2468-1253(20)30077-7 [5] WANG AY, DHALIWAL J, MOUZAKI M. Lean non-alcoholic fatty liver disease[J]. Clin Nutr, 2019, 38(3): 975-981. DOI: 10.1016/j.clnu.2018.08.008 [6] KIM SH, PARK HY, LEE HS, et al. Association between non-alcoholic fatty liver disease and coronary calcification depending on sex and obesity[J]. Sci Rep, 2020, 10(1): 1025. DOI: 10.1038/s41598-020-57894-y [7] AHMED M. Non-alcoholic fatty liver disease in 2015[J]. World J Hepatol, 2015, 7(11): 1450-1459. DOI: 10.4254/wjh.v7.i11.1450 [8] TOBARI M, HASHIMOTO E, TANIAI M, et al. Characteristics of non-alcoholic steatohepatitis among lean patients in Japan: Not uncommon and not always benign[J]. J Gastroenterol Hepatol, 2019, 34(8): 1404-1410. DOI: 10.1111/jgh.14585 [9] GONZALEZ-CANTERO J, MARTIN-RODRIGUEZ JL, GONZALEZ-CANTERO A, et al. Insulin resistance in lean and overweight non-diabetic Caucasian adults: Study of its relationship with liver triglyceride content, waist circumference and BMI[J]. PLoS One, 2018, 13(2): e0192663. DOI: 10.1371/journal.pone.0192663 [10] HONDA Y, YONEDA M, KESSOKU T, et al. Characteristics of non-obese non-alcoholic fatty liver disease: Effect of genetic and environmental factors[J]. Hepatol Res, 2016, 46(10): 1011-1018. DOI: 10.1111/hepr.12648 [11] NISHIOJI K, MOCHIZUKI N, KOBAYASHI M, et al. The impact of PNPLA3 rs738409 genetic polymorphism and weight gain ≥10 kg after age 20 on non-alcoholic fatty liver disease in non-obese Japanese individuals[J]. PLoS One, 2015, 10(10): e0140427. DOI: 10.1371/journal.pone.0140427 [12] LU FB, HU ED, XU LM, et al. The relationship between obesity and the severity of non-alcoholic fatty liver disease: Systematic review and meta-analysis[J]. Expert Rev Gastroenterol Hepatol, 2018, 12(5): 491-502. DOI: 10.1080/17474124.2018.1460202 [13] TU LN, SHOWALTER MR, CAJKA T, et al. Metabolomic characteristics of cholesterol-induced non-obese nonalcoholic fatty liver disease in mice[J]. Sci Rep, 2017, 7(1): 6120. DOI: 10.1038/s41598-017-05040-6 [14] BASARANOGLU M, BASARANOGLU G, BUGIANESI E. Carbohydrate intake and nonalcoholic fatty liver disease: Fructose as a weapon of mass destruction[J]. Hepatobiliary Surg Nutr, 2015, 4(2): 109-116. [15] LI C, GUO P, OKEKUNLE AP, et al. Lean non-alcoholic fatty liver disease patients had comparable total caloric, carbohydrate, protein, fat, iron, sleep duration and overtime work as obese non-alcoholic fatty liver disease patients[J]. J Gastroenterol Hepatol, 2019, 34(1): 256-262. DOI: 10.1111/jgh.14360 [16] KIM D, KIM WR. Nonobese fatty liver disease[J]. Clin Gastroenterol Hepatol, 2017, 15(4): 474-485. DOI: 10.1016/j.cgh.2016.08.028 [17] SUN YY, LIANG L, WANG XY, et al. Improvement effect of dapagliflozin on liver function in patients with type 2 diabetes mellitus complicated with non-alcoholic fatty liver disease and its mechanism[J]. J Jilin Univ (Med Edit), 2020, 46(1): 116-120. (in Chinese) https://www.cnki.com.cn/Article/CJFDTOTAL-BQEB202001022.htm孙媛媛, 梁丽, 王笑烨, 等. 达格列净对2型糖尿病并发非酒精性脂肪性肝病患者肝功能的改善作用及其机制[J]. 吉林大学学报(医学版), 2020, 46(1): 116-120. https://www.cnki.com.cn/Article/CJFDTOTAL-BQEB202001022.htm [18] YANG CW, LIU X, LIU XR, et al. The relationship between waist circumference and new-onset non-alcoholic fatty liver disease in non-obese patients with diabetes mellitus[J]. Tianjin Med J, 2015, 43(1): 74-77. (in Chinese) https://www.cnki.com.cn/Article/CJFDTOTAL-TJYZ201501021.htm杨春伟, 刘星, 刘秀荣, 等. 糖尿病非肥胖人群腰围与新发非酒精性脂肪肝的关系[J]. 天津医药, 2015, 43(1): 74-77. https://www.cnki.com.cn/Article/CJFDTOTAL-TJYZ201501021.htm [19] ZHENG X, GONG L, LUO R, et al. Serum uric acid and non-alcoholic fatty liver disease in non-obesity Chinese adults[J]. Lipids Health Dis, 2017, 16(1): 202. DOI: 10.1186/s12944-017-0531-5 [20] KIM JJ, KIM D, YIM JY, et al. Polycystic ovary syndrome with hyperandrogenism as a risk factor for non-obese non-alcoholic fatty liver disease[J]. Aliment Pharmacol Ther, 2017, 45(11): 1403-1412. DOI: 10.1111/apt.14058 [21] WONG VW, WONG GL, CHAN RS, et al. Beneficial effects of lifestyle intervention in non-obese patients with non-alcoholic fatty liver disease[J]. J Hepatol, 2018, 69(6): 1349-1356. DOI: 10.1016/j.jhep.2018.08.011 [22] JIN YJ, KIM KM, HWANG S, et al. Exercise and diet modification in non-obese non-alcoholic fatty liver disease: Analysis of biopsies of living liver donors[J]. J Gastroenterol Hepatol, 2012, 27(8): 1341-1347. DOI: 10.1111/j.1440-1746.2012.07165.x [23] TAKAHASHI H, ONO M, HYOGO H, et al. Biphasic effect of alcohol intake on the development of fatty liver disease[J]. J Gastroenterol, 2015, 50(11): 1114-1123. DOI: 10.1007/s00535-015-1058-z [24] ZHOU Q, SU J, JI MY. Progress in the treatment of nonalcoholic fatty liver disease[J]. China Med Herald, 2020, 17(6): 26-29. (in Chinese) https://www.cnki.com.cn/Article/CJFDTOTAL-YYCY202006008.htm周谦, 苏娟, 季梦遥. 非酒精性脂肪性肝病的治疗研究进展[J]. 中国医药导报, 2020, 17(6): 26-29. https://www.cnki.com.cn/Article/CJFDTOTAL-YYCY202006008.htm [25] ATTIA SL, SOFTIC S, MOUZAKI M. Evolving role for pharmacotherapy in NAFLD/NASH[J]. Clin Transl Sci, 2020.[Epub ahead of print] [26] FIORUCCI S, BIAGIOLI M, SEPE V, et al. Bile acid modulators for the treatment of nonalcoholic steatohepatitis (NASH)[J]. Expert Opin Investig Drugs, 2020, 29(6): 623-632. DOI: 10.1080/13543784.2020.1763302 [27] TANG Y, HUANG J, ZHANG WY, et al. Effects of probiotics on nonalcoholic fatty liver disease: A systematic review and meta-analysis[J]. Therap Adv Gastroenterol, 2019, 12: 1756284819878046. [28] ZHOU Y, ZHENG T, CHEN H, et al. Microbial intervention as a novel target in treatment of non-alcoholic fatty liver disease progression[J]. Cell Physiol Biochem, 2018, 51(5): 2123-2135. DOI: 10.1159/000495830 [29] XU RH, XIN QF. Efficacy of Ezetimibe in the treatment of non-obese patients with non-alcoholic fatty liver disease[J]. Chin J Convalescent Med, 2017, 26(7): 760-762. (in Chinese) https://www.cnki.com.cn/Article/CJFDTOTAL-ZGLX201707041.htm许瑞华, 辛庆锋. 依折麦布治疗非肥胖的非酒精性脂肪肝患者疗效观察[J]. 中国疗养医学, 2017, 26(7): 760-762. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGLX201707041.htm [30] ENJOJI M, MACHIDA K, KOHJIMA M, et al. NPC1L1 inhibitor ezetimibe is a reliable therapeutic agent for non-obese patients with nonalcoholic fatty liver disease[J]. Lipids Health Dis, 2010, 9: 29. DOI: 10.1186/1476-511X-9-29 [31] SUN GP, CHEN YM, MENG J. Clinical observation on rosiglitazone in the treatment of non-obese type 2 diabetic mellitus with fatty liverr[J]. Clin J Chin Med, 2014, 6(15): 63-64, 67. (in Chinese) DOI: 10.3969/j.issn.1674-7860.2014.15.029孙广平, 陈奕名, 孟君. 罗格列酮对非肥胖2型糖尿病合并脂肪肝的疗效观察[J]. 中医临床研究, 2014, 6(15): 63-64, 67. DOI: 10.3969/j.issn.1674-7860.2014.15.029 [32] FERNÁNDEZ-MARTÍNEZ E, LIRA-ISLAS IG, CARIÑO-CORTÉS R, et al. Dietary chia seeds (Salvia hispanica) improve acute dyslipidemia and steatohepatitis in rats[J]. J Food Biochem, 2019, 43(9): e12986. [33] BURTON BK, BALWANI M, FEILLET F, et al. A phase 3 trial of sebelipase alfa in lysosomal acid lipase deficiency[J]. N Engl J Med, 2015, 373(11): 1010-1020. DOI: 10.1056/NEJMoa1501365 [34] QU YL, WANG YC, WAN JX. Association of nonalcoholic fatty liver disease with vitamin D and bone mineral density[J]. J Clin Hepatol, 2019, 35(9): 2021-2025. (in Chinese) DOI: 10.3969/j.issn.1001-5256.2019.09.027曲玉蕾, 王迎春, 万金鑫. 非酒精性脂肪性肝病与血清维生素D及骨密度的关系[J]. 临床肝胆病杂志, 2019, 35(9): 2021-2025. DOI: 10.3969/j.issn.1001-5256.2019.09.027 [35] ZHAI HL, WANG NJ, HAN B, et al. Low vitamin D levels and non-alcoholic fatty liver disease, evidence for their independent association in men in East China: A cross-sectional study (Survey on Prevalence in East China for Metabolic Diseases and Risk Factors (SPECT-China))[J]. Br J Nutr, 2016, 115(8): 1352-1359. DOI: 10.1017/S0007114516000386 [36] DABBAGHMANESH MH, DANAFAR F, ESHRAGHIAN A, et al. Vitamin D supplementation for the treatment of non-alcoholic fatty liver disease: A randomized double blind placebo controlled trial[J]. Diabetes Metab Syndr, 2018, 12(4): 513-517. DOI: 10.1016/j.dsx.2018.03.006 [37] DASARATHY J, VARGHESE R, FELDMAN A, et al. Patients with nonalcoholic fatty liver disease have a low response rate to vitamin D supplementation[J]. J Nutr, 2017, 147(10): 1938-1946. DOI: 10.3945/jn.117.254292 [38] SHIMOKOBE H, SUMIDA Y, TANAKA S, et al. Human placental extract treatment for non-alcoholic steatohepatitis non-responsive to lifestyle intervention: A pilot study[J]. Hepatol Res, 2015, 45(9): 1034-1040. DOI: 10.1111/hepr.12432 [39] POLCE SA, BURKE C, FRANÇA LM, et al. Ellagic acid alleviates hepatic oxidative stress and insulin resistance in diabetic female rats[J]. Nutrients, 2018, 10(5): 531. DOI: 10.3390/nu10050531 [40] LI JJ, GAO H, LV Y, et al. Zeaxanthin dipalmitate alleviates hepatic injury induced by superimposed chronic hepatitis B and non-alcoholic steatohepatitis in non-obese mice[J]. J Asian Nat Prod Res, 2017, 19(9): 910-923. DOI: 10.1080/10286020.2017.1349759 [41] CRUZ ACD, BUGIANESI E, GEORGE J, et al. Characteristics and long-term prognosis of lean patients with nonalcoholic fatty liver disease[J]. Gastroenterology, 2014, 146(Suppl 1): s909. [42] NIRIELLA MA, KASTURIRATNE A, PATHMESWARAN A, et al. Lean non-alcoholic fatty liver disease (lean NAFLD): Characteristics, metabolic outcomes and risk factors from a 7-year prospective, community cohort study from Sri Lanka[J]. Hepatol Int, 2019, 13(3): 314-322. DOI: 10.1007/s12072-018-9916-4 [43] KUMAR R, RASTOGI A, SHARMA MK, et al. Clinicopathological characteristics and metabolic profiles of non-alcoholic fatty liver disease in Indian patients with normal body mass index: Do they differ from obese or overweight non-alcoholic fatty liver disease?[J]. Indian J Endocrinol Metab, 2013, 17(4): 665-671. DOI: 10.4103/2230-8210.113758 -



 PDF下载 ( 2502 KB)
PDF下载 ( 2502 KB)

 下载:
下载: