PALBI评分对肝硬化合并急性上消化道出血患者短期预后的预测价值
DOI: 10.3969/j.issn.1001-5256.2021.07.020
Value of platelet-albumin-bilirubin score in predicting the short-term prognosis of patients with liver cirrhosis and acute upper gastrointestinal bleeding
-
摘要:
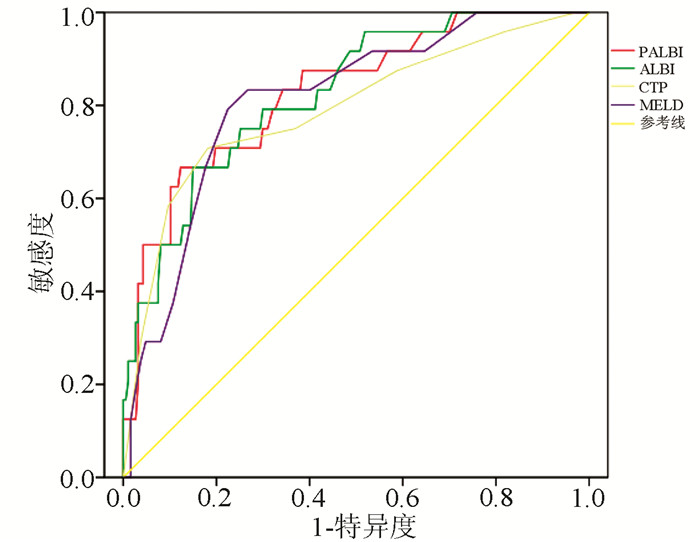
目的 评估血小板-白蛋白-胆红素评分(PALBI)对肝硬化合并急性上消化道出血患者30 d内死亡的预测价值。 方法 回顾性收集2016年1月—2020年2月在复旦大学附属金山医院因急性上消化道出血入院的211例肝硬化患者,根据30 d内生存情况分为死亡组(n=24)和生存组(n=187),收集患者的流行病学资料(年龄、性别等)和实验室检查资料(血常规、肝肾功能、凝血功能等),计算入院时的PALBI、ALBI、CTP和MELD评分,比较两组间评分是否存在差异。计量资料两组间比较采用t检验;计数资料两组间比较采用χ2检验。通过受试者工作特征曲线(ROC曲线)及曲线下面积(AUC)衡量模型的预测能力。AUC的比较采用DeLong检验。 结果 死亡组PALBI、ALBI、CTP和MELD评分分别为-1.47± 0.35、-0.74±0.49、10.25±1.98、17.25±4.68,生存组PALBI、ALBI、CTP和MELD分值分别为-1.94±0.36、-1.38±0.51、8.06±1.70、11.63±4.83,死亡组各项评分均明显高于生存组(P值均<0.001)。PALBI、ALBI、CTP和MELD评分的ROC曲线下面积分别为0.827、0.824、0.790、0.811,AUC两两比较差异均无统计学意义(P值均>0.05)。 结论 PALBI评分对肝硬化合并急性上消化道出血30 d内死亡的预测表现良好,与CTP和MELD评分相当。 Abstract:Objective To investigate the value of platelet-albumin-bilirubin score (PALBI) in predicting the 30-day mortality of patients with liver cirrhosis and acute upper gastrointestinal bleeding (AUGIB). Methods A retrospective analysis was performed for the clinical data of 211 patients with liver cirrhosis who were admitted to Jinshan Hospital of Fudan University due to AUGIB from January 2016 to February 2020, and according to the survival status within 30 days, they were divided into death group with 24 patients and survival group with 187 patients. Epidemiological data (including age and sex) and laboratory examination results (including routine blood test results, hepatic and renal function, and coagulation function) were collected, and the scores of PALBI, albumin-bilirubin (ALBI), Child-Turcotte-Pugh (CTP), and Model for End-Stage Liver Disease (MELD) on admission were calculated and compared between the two groups. The t-test was used for comparison of continuous data between groups, and the chi-square test was used for comparison of categorical data between groups. With the application of 95% confidence interval, the receiver operating characteristic (ROC) curve and the area under the ROC curve (AUC) were used to evaluate the predictive ability of the model. The DeLong test was used for comparison of ROC curve. Results Compared with the survival group, the death group had significantly higher PALBI score (-1.47±0.35 vs -1.94±0.36, P < 0.001), ALBI score (-0.74±0.49 vs -1.38±0.51, P < 0.001), CTP score (10.25±1.98 vs 8.06±1.70, P < 0.001), and MELD score (17.25±4.68 vs 11.63±4.83, P < 0.001). PALBI, ALBI, CTP, and MELD scores had an AUC of 0.827, 0.824, 0.790, and 0.811, respectively, and there was no significant difference in AUC between any two scores (P > 0.05). Conclusion PALBI score has good performance in predicting the 30-day mortality of patients with liver cirrhosis and AUGIB and is comparable to CTP and MELD scores. -
Key words:
- Liver Cirrhosis /
- Hemorrhage /
- Platelet-albumin-bilirubin Score /
- Prognosis
-
表 1 CTP评分计算方式[7]
指标 1分 2分 3分 总胆红素(μmol/L) <34 34~51 >51 白蛋白(g/L) >35 28~35 <28 凝血酶原时间延长(s) <4 4~6 >6 腹水 无 轻度 中度 肝性脑病(级) 无 1~2 3~4 表 2 死亡组与生存组一般情况及生化指标比较
指标 死亡组(n=24) 生存组(n=187) 统计值 P值 男/女(例) 16/8 100/87 χ2=1.495 0.221 年龄(岁) 68.96±16.95 68.42±12.68 t=0.151 0.881 休克指数(心率/收缩压) 0.88±0.29 0.77±0.21 t=1.834 0.078 合并原发性肝细胞癌[例(%)] 5(20.8) 44(23.5) χ2=0.087 0.768 合并糖尿病[例(%)] 7(29.2) 51(27.3) χ2=0.038 0.845 红细胞计数(×1012/L) 2.50±0.67 2.66±0.82 t=-0.908 0.365 血红蛋白(g/L) 82.3±27.5 76.2±20.0 t=1.035 0.310 胃镜检查[例(%)] 16(66.7) 140(74.9) 有门静脉高压性出血 13(81.3) 110(78.6) 无门静脉高压性出血 3(18.7) 30(21.4) 表 3 两组四种评分的比较
评分类型 死亡组(n=24) 生存组(n=187) t值 P值 PALBI评分 -1.47±0.35 -1.94±0.36 6.138 <0.001 1级[例(%)] 0 5(2.7) 2级[例(%)] 1(4.2) 56(29.9) 3级[例(%)] 23(95.8) 126(67.4) ALBI评分 -0.74±0.49 -1.38±0.51 5.850 <0.001 1级[例(%)] 0 1(0.5) 2级[例(%)] 2(8.3) 91(48.7) 3级[例(%)] 22(91.7) 95(50.8) CPT评分 10.25±1.98 8.06±1.70 5.799 <0.001 A级[例(%)] 1(4.2) 35(18.7) B级[例(%)] 6(25) 118(63.1) C级[例(%)] 17(70.8) 34(18.2) MELD评分 17.25±4.68 11.63±4.83 5.381 <0.001 表 4 四种评分系统预测肝硬化合并上消化道出血患者30天内死亡的ROC曲线结果
评分类型 AUC(95%CI) 最佳截断值 敏感度(%) 特异度(%) PALBI评分 0.827(0.739~0.915) -1.535 66.7 87.7 ALBI评分 0.824(0.740~0.908) -0.855 66.7 85.0 CTP评分 0.790(0.683~0.898) 9.5 70.8 81.8 MELD评分 0.811(0.725~0.897) 14.5 79.2 77.5 -
[1] XAVIER SA, VILAS-BOAS R, BOAL CARVALHO P, et al. Assessment of prognostic performance of Albumin-Bilirubin, Child-pugh, and Model for End-stage Liver Disease scores in patients with liver cirrhosis complicated with acute upper gastrointestinal bleeding[J]. Eur J Gastroenterol Hepatol, 2018, 30(6): 652-658. DOI: 10.1097/MEG.0000000000001087. [2] ROAYAIE S, JIBARA G, BERHANE S, et al. 851 PALBI-An objective score based on platelets, albumin bilirubin stratifies HCC patients undergoing resection & ablation better than child's classification[J]. Hepatology, 2015, 62(Suppl 1): 624A-690A. DOI: 10.1002/hep.28219. [3] JOHNSON PJ, BERHANE S, KAGEBAYASHI C, et al. Assessment of liver function in patients with hepatocellular carcinoma: A new evidence-based approach-the ALBI grade[J]. J Clin Oncol, 2015, 33(6): 550-558. DOI: 10.1200/JCO.2014.57.9151. [4] ZOU DL, QI XS, ZHU CH, et al. Albumin-bilirubin score for predicting the in-hospital mortality of acute upper gastrointestinal bleeding in liver cirrhosis: A retrospective study[J]. Turk J Gastroenterol, 2016, 27(2): 180-186. DOI: 10.5152/tjg.2016.15502. [5] OIKONOMOU T, GOULIS L, DOUMTSIS P, et al. ALBI and PALBI grades are associated with the outcome of patients with stable decompensated cirrhosis[J]. Ann Hepatol, 2019, 18(1): 126-136. DOI: 10.5604/01.3001.0012.7904. [6] FREEMAN RB Jr, WIESNER RH, HARPER A, et al. The new liver allocation system: Moving toward evidence-based transplantation policy[J]. Liver Transpl, 2002, 8(9): 851-858. DOI: 10.1053/jlts.2002.35927. [7] CHILD ⅢCG, TURCOTTE JG. Surgery and portal hypertension[M]//In Child ⅢCG, ed. The liver and portal hypertension. Philadelphia: Saunders. 1964: 50. [8] PENG Y, QI XS, DAI JN, et al. Child-Pugh versus MELD score for predicting the in-hospital mortality of acute upper gastrointestinal bleeding in liver cirrhosis[J]. Int J Clin Exp Med, 2015, 8(1): 751-757. https://europepmc.org/articles/PMC4358508 [9] LISMAN T, van LEEUWEN Y, ADELMEIJER J, et al. Interlaboratory variability in assessment of the Model of End-stage Liver Disease score[J]. Liver Int, 2008, 28(10): 1344-1351. DOI: 10.1111/j.1478-3231.2008.01783.x. [10] TROTTER JF, OLSON J, LEFKOWITZ J, et al. Changes in international normalized ratio (INR) and model for endstage liver disease (MELD) based on selection of clinical laboratory[J]. Am J Transplant, 2007, 7(6): 1624-1628. DOI: 10.1111/j.1600-6143.2007.01822.x. [11] HANSMANN J, EVERS MJ, BUI JT, et al. Albumin-bilirubin and platelet-albumin-bilirubin grades accurately predict overall survival in high-risk patients undergoing conventional transarterial chemoembolization for hepatocellular carcinoma[J]. J Vasc Interv Radiol, 2017, 28(9): 1224-1231. e2. DOI: 10.1016/j.jvir.2017.05.020. [12] LIU PH, HSU CY, HSIA CY, et al. ALBI and PALBI grade predict survival for HCC across treatment modalities and BCLC stages in the MELD Era[J]. J Gastroenterol Hepatol, 2017, 32(4): 879-886. DOI: 10.1111/jgh.13608. [13] LEE SK, SONG MJ, KIM SH, et al. Comparing various scoring system for predicting overall survival according to treatment modalities in hepatocellular carcinoma focused on Platelet-albumin-bilirubin (PALBI) and albumin-bilirubin (ALBI) grade: A nationwide cohort study[J]. PLoS One, 2019, 14(5): e0216173. DOI: 10.1371/journal.pone.0216173. [14] CHAN AWH, CHAN RCK, WONG GLH, et al. New simple prognostic score for primary biliary cirrhosis: Albumin-bilirubin score[J]. J Gastroenterol Hepatol, 2015, 30(9): 1391-1396. DOI: 10.1111/jgh.12938. [15] ITO T, ISHIGAMI M, MOROOKA H, et al. The albumin-bilirubin score as a predictor of outcomes in Japanese patients with PBC: An analysis using time-dependent ROC[J]. Sci Rep, 2020, 10(1): 17812. DOI: 10.1038/s41598-020-74732-3. [16] CHEN RC, CAI YJ, WU JM, et al. Usefulness of albumin-bilirubin grade for evaluation of long-term prognosis for hepatitis B-related cirrhosis[J]. J Viral Hepat, 2017, 24(3): 238-245. DOI: 10.1111/jvh.12638. [17] KOJI F, KYOKO O, HIROHITO Y, et al. Albumin-bilirubin score indicates liver fibrosis staging and prognosis in patients with chronic hepatitis C[J]. Hepatol Res, 2019, 49(7): 731-742. DOI: 10.1111/hepr.13333. [18] ELSHAARAWY O, ALLAM N, ABDELSAMEEA E, et al. Platelet-albumin-bilirubin score - a predictor of outcome of acute variceal bleeding in patients with cirrhosis[J]. World J Hepatol, 2020, 12(3): 99-107. DOI: 10.4254/wjh.v12.i3.99. [19] ROBERTSON M, NG J, SHAWISH WA, et al. Risk stratification in acute variceal bleeding: Comparison of the AIMS65 score to established upper gastrointestinal bleeding and liver disease severity risk stratification scoring systems in predicting mortality and rebleeding[J]. Dig Endosc, 2020, 32(5): 761-768. DOI: 10.1111/den.13577. -



 PDF下载 ( 2087 KB)
PDF下载 ( 2087 KB)

 下载:
下载:


