性别差异对自身免疫性肝炎患者临床特征及预后的影响
DOI: 10.3969/j.issn.1001-5256.2021.07.031
Clinical features and prognosis of autoimmune hepatitis patients with different sexes
-
摘要:
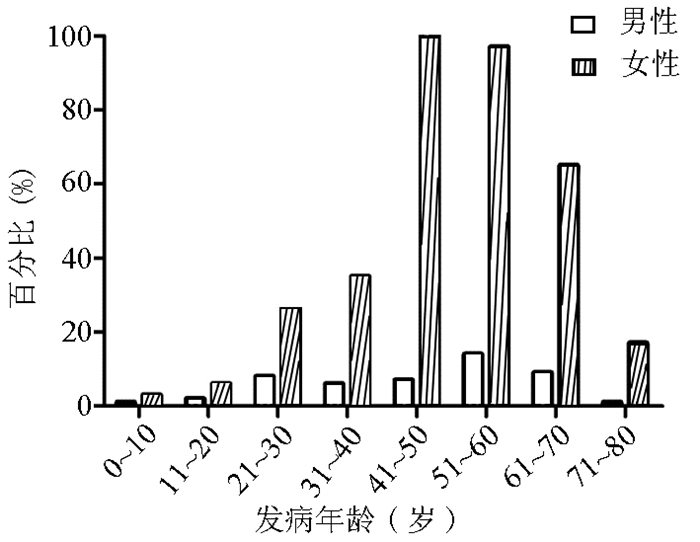
目的 自身免疫性肝炎(AIH)主要发生在女性,目前对男性AIH患者的研究甚少,本研究比较不同性别AIH之间的临床差异。 方法 收集2009年10月—2019年10月在北京佑安医院住院并确诊为AIH的患者398例进行回顾性研究,分为男(n=48)、女(n=350)两组,对一般情况、临床特点及预后等影响因素进行分析。主要研究终点为死亡或肝移植治疗。正态分布的计量资料2组间比较采用t检验,非正态分布计量资料2组间比较采用Mann-Whitney U检验。计数资料2组间比较采用χ2检验或Fisher精确概率法。采用Cox比例风险模型进行单变量和多变量分析。 结果 年龄方面,51~60岁是两组的发病高峰,但是男性在21~30岁时段确诊率明显高于女性(8/48 vs 24/334,χ2=4.915,P=0.027),而在41~50岁时段则低于女性(7/48 vs 97/334,χ2=4.428,P=0.035)。AIH分类方面,男性特发性AIH占比更高(31/48 vs 170/350,χ2=4.329,P=0.037),但男性合并其他自身免疫性疾病尤其是甲状腺功能亢进比例低于女性(0/48 vs 39/348,P=0.008)。实验室检查方面,男性ANA≥1∶ 100(42/48 vs 325/340,χ2=5.375,P=0.020) 和SSA/SSB(2/48 vs 76/340,χ2=7.566,P=0.006)阳性率显著低于女性患者;男性ANA ≥1∶ 1000的比率显著低于女性(P<0.000 1)。预后方面,男性出现死亡或接受肝移植的年龄要远小于女性[(31.5±15.9)岁vs (53.9±12.6)岁,t=3.798,P=0.001],男性失代偿期肝硬化及肝细胞癌发生更多见(P值均<0.05)。与生存期下降有关的高危因素,男性: 糖尿病、肝硬化以及血Alb<31.4 g/L,女性: 肝衰竭、肝硬化、ANA≥1∶ 1000、DBil>42 μmol/L、淋巴细胞计数<1.2×109/L以及补体C3<0.588 g/L(P值均<0.05)。 结论 性别差异对AIH患者临床表现和预后有一定影响,主要表现在男性患者更年轻、预后更差。 Abstract:Objective To investigate the differences between autoimmune hepatitis (AIH) patients with different sexes, since AIH is more common in female individuals and there are few studies on male AIH patients. Methods A retrospective analysis was performed for 398 patients who were hospitalized in Beijing YouAn Hospital from October 2009 to October 2019 and were diagnosed with AIH, and the patients were divided into female group and male group according to sex. General status, clinical features, and prognosis were analyzed. The primary outcome measure was death or liver transplantation. The t-test was used for comparison of normally distributed continuous data between two groups, and the Mann-Whitney U test was used for comparison of non-normally distributed continuous data between two groups; the chi-square test or the Fisher's exact test was used for comparison of categorical data between two groups. The Cox proportional hazards model was used to perform univariate and multivariate analyses. Results As for age, the peak of disease onset was observed in patients aged 51-60 years in both male and female groups, and compared with the female group, the male group had a significantly higher rate of confirmed diagnosis at the age of 21-30 years (8/48 vs 24/334, χ2=4.915, P=0.027) and a significantly lower rate of confirmed diagnosis at the age of 41-50 years (7/48 vs 97/334, χ2=4.428, P=0.035). As for AIH, compared with the female group, the male group had a significantly higher proportion of patients with idiopathic AIH (31/48 vs 170/350, χ2=4.329, P=0.037) and a significantly lower proportion of patients with other autoimmune diseases, especially hyperthyroidism (0/48 vs 39/348, P=0.008). As for laboratory examination, compared with the female group, the male group had significantly lower positive rates of anti-nuclear antibody (ANA)≥1∶ 100(42/48 vs 325/340, χ2=5.375, P=0.020) and SSA/SSB (2/48 vs 76/340, χ2=7.566, P=0.006), as well as a significantly lower proportion of patients with ANA ≥1∶ 1000 (P < 0.000 1). As for prognosis, compared with the female group, the male group had a significantly younger age at the time of death or liver transplantation (31.5±15.9 years vs 53.9±12.6 years, t=3.798, P=0.001) and a significantly higher proportion of patients with decompensated liver cirrhosis or hepatocellular carcinoma (both P < 0.05). Diabetes, liver cirrhosis, and blood albumin < 31.4 g/L were high-risk factors for reduced survival time in male patients, and liver failure, liver cirrhosis, ANA ≥1∶ 1000, direct bilirubin > 42 μmol/L, lymphocyte count < 1.2×109/L, and C3 < 0.588 g/L were high-risk factors for reduced survival time in female patients. Conclusion Sex difference has certain influence on the clinical manifestations and prognosis of AIH patients, and male patients tend to have a younger age and a poorer prognosis. -
Key words:
- Hepatitis, Autoimmune /
- Gender /
- Signs and Symptoms /
- Prognosis
-
表 1 不同性别患者一般资料比较
指标 例数 男性 女性 统计值 P值 随访时间(月) 367 60.3±46.4 74.2±54.0 t=1.658 0.098 发病年龄(岁) 392 46.8(6.0~79.0) 50.1(3.0~85.0) Z=1.195 0.115 发病年龄段[例(%)] 0~10岁 4 1/48(2.1) 3/334(0.9) χ2=0.000 1.000 11~20岁 8 2/48(4.2) 6/334(1.8) χ2=0.284 0.594 21~30岁 32 8/48(16.7) 24/334(7.2) χ2=4.915 0.027 31~40岁 40 6/48(12.5) 34/334(10.2) χ2=0.241 0.623 41~50岁 104 7/48(14.6) 97/334(29.0) χ2=4.428 0.035 51~60岁 105 14/48(29.2) 91/334(27.2) χ2=0.078 0.780 61~70岁 71 9/48(18.8) 62/334(18.6) χ2=0.001 0.975 >70岁 18 1/48(2.1) 17/334(5.1) χ2=0.308 0.579 诊断年龄(岁) 392 48.0(6.0~79.0) 51.0(3.0~85.0) Z=-0.491 0.623 诊断用时(月) 374 9.0(0~126.0) 13.9(0~241.0) Z=-1.940 0.052 无症状体检发现[例(%)] 83 4/45(8.9) 79/334(30.0) χ2=3.897 0.048 AIH分类[例(%)] I-AIH 201 31/48(64.6) 170/350(48.6) χ2=4.329 0.037 DI-AIH 115 9/48(18.8) 106/350(30.3) χ2=2.734 0.098 OS 77 8/48(16.7) 69/350(27.6) χ2=0.251 0.616 DI-AIH合并OS 5 0/48(0) 5/350(1.4) 1.000 肝硬化[例(%)] 168 20/47(42.6) 148/339(43.7) χ2=0.020 0.886 失代偿 78 14/20(70.0) 64/148(43.2) χ2=5.071 0.024 糖尿病[例(%)] 55 6/45(13.3) 49/316(15.5) χ2=0.144 0.704 肝衰竭[例(%)] 57 6/48(12.5) 51/350(14.6) χ2=0.148 0.701 合并其他免疫病[例(%)] 169 14/48(29.2) 155/348(44.5) χ2=4.075 0.044 自身免疫性甲状腺疾病 45 1/48(2.2) 44/348(12.6) χ2=3.681 0.055 甲状腺功能亢进 39 0/48(0) 39/348(11.2) 0.008 甲状腺功能减弱 6 1/48(2.1) 5/348(1.4) χ2=0.000 1.000 PBC 70 6/48(13.3) 64/348(18.4) χ2=1.006 0.316 PSC 3 1/48(2.2) 2/348(0.6) χ2=0.059 0.809 SLE 10 1/48(2.2) 9/348(2.6) χ2=0.000 1.000 干燥综合征 36 2/48(4.2) 34/348(9.8) χ2=0.996 0.318 表 2 男性和女性AIH患者实验室检查结果
指标 例数 男性 女性 统计值 P值 ALT(U/L) 390 514(12~2255) 372(4~2270) Z=-1.058 0.290 AST(U/L) 389 342(21~1725) 380(16~2094) Z=-0.568 0.570 TBil(μmol/L) 385 88.1(8.3~535.1) 100.2(5.8~765.7) Z=-0.696 0.486 DBil(μmol/L) 378 61.8(1.9~383.0) 65.4(0.9~603.0) Z=-0.191 0.849 GGT(U/L) 375 209(24~951) 174(11~1357) Z=-1.034 0.306 ALP(U/L) 373 176(64~966) 182(27~1189) Z=-0.555 0.579 TBA(μmol/L) 365 82.7(2.7~368.8) 80.0(1.3~319.0) Z=-0.417 0.676 Alb(g/L) 379 35.30±8.31 35.10±6.28 t=-0.124 0.902 GLOB(g/L) 375 40.6±13.2 38.8±9.2 t=-0.838 0.407 ChE(U/L) 364 4642±2382 4785±2073 t=0.395 0.693 WBC(×109) 374 5.7(2.2~12.5) 4.8(1.4~12.0) Z=-2.476 0.013 NE(×109) 363 2.70(2.07~3.85) 2.35(1.68±3.18) Z=-2.500 0.012 LY(×109) 360 1.80±0.77 1.60±0.66 t=-1.460 0.151 Hb(g/L) 371 131.0±24.6 118.0±17.0 t=-3.427 0.001 PLT(×109) 370 163±75 161±77 t=-0.193 0.847 IgG(g/L) 377 25.6±11.5 24.6±8.9 t=-0.634 0.527 IgM(g/L) 371 1.39(0.89~2.53) 1.72(1.19~2.63) Z=-1.609 0.108 C3(g/L) 365 0.96±0.34 0.94±0.38 t=-0.417 0.677 C4(g/L) 365 0.16(0.10~0.25) 0.15(0.10~0.21) Z =-0.815 0.415 注:TBA,总胆汁酸;GLOB,球蛋白;ChE,胆碱酯酶;LY,淋巴细胞。 表 3 男性和女性AIH患者血清自身抗体及核型
指标 例数 男性 女性 χ2值 P值 自身抗体阳性[例(%)] 388 48/48(100) 340/350(97.1) 0.617 ANA≥1∶100 367 42/48(87.5) 325/340(95.6) 5.375 0.020 ANA≥1∶1000 217 11/48(22.9) 206/340(60.6) 24.217 <0.001 SMA≥1∶100 54 5/48(10.4) 49/340(14.4) 0.560 0.454 SMA≥1∶1000 8 1/48(2.1) 7/340(2.1) 0.000 1.000 AMA≥1∶320 84 7/48(14.6) 77/340(22.6) 1.612 0.204 LKM-1 12 3/48(6.3) 9/340(2.6) 0.818 0.366 SLA/LP 24 1/48(2.1) 23/340(6.8) 0.884 0.347 SSA/SSB 78 2/48(4.2) 76/340(22.4) 7.566 0.006 GP210 23 3/48(6.3) 20/340(5.9) 0.000 1.000 Sp100 15 1/48(2.1) 14/340(4.1) 0.081 0.776 ANA核型[例(%)] 核颗粒型 109 9/13(69.2) 100/154(64.9) 0.098 0.775 胞浆颗粒型 65 5/13(38.5) 60/154(39.0) 0.001 0.972 核均质型 59 4/13(30.8) 55/154(35.7) 0.003 0.955 核膜型 12 1/13(7.7) 11/154(7.1) 0.000 1.000 着丝点型 5 1/13(7.7) 4/154(2.6) 0.035 0.851 核仁型 9 0/13(0) 9/154(5.8) 0.000 1.000 表 4 男性和女性AIH嗜肝病毒感染情况
指标 例数 男性 女性 χ2值 P值 HAV-IgG[例(%)] 333 35/35(100.0) 297/298(99.7) 1.000 抗-HBc阳性且HBsAg阴性[例(%)] 155 21/31(67.7) 134/291(46.0) 5.281 0.022 肝硬化 80 10/21(47.6) 70/134(52.2) 0.155 0.694 死亡或肝移植 18 4/21(19.0) 14/70(20.0) 0.000 1.000 HCV-IgG[例(%)] 6 0/35(0) 6/264(2.3) 1.000 HEV-IgG[例(%)] 55 3/16(18.8) 52/221(23.5) 0.017 0.896 EBV-IgG[例(%)] 30 0/17(0) 30/211(14.2) 0.138 CMV-IgG[例(%)] 115 13/19(68.4) 102/209(48.8) 2.681 0.102 PVB19-IgG[例(%)] 47 3/15(20.0) 44/126(34.9) 0.755 0.385 表 5 男性和女性AIH治疗及预后情况
指标 例数 男性 女性 统计值 P值 治疗[例(%)] 224 28/48(56.3) 196/350(56.0) χ2=0.093 0.974 单用皮质醇激素 156 15/28(55.6) 141/196(71.9) χ2=3.910 0.048 单用硫唑嘌呤 5 1/28(3.7) 4/196(2.0) χ2=0.000 1.000 皮质醇激素和硫唑嘌呤 62 11/28(40.7) 51/196(26.0) χ2=2.154 0.142 二线药物 6 2/28(7.4) 4/196(2.0) χ2=0.881 0.348 治疗有效[例(%)] 214 28/28(82.4) 186/196(92.1) 0.618 停药或减量后反弹 84 13/28(38.2) 71/196(36.2) χ2=1.088 0.297 依从性好 214 27/28(92.9) 187/196(94.9) χ2=0.000 1.000 药物不良反应[例(%)] 111 15/28(53.6) 96/196(49.0) χ2=0.207 0.649 感染 68 10/28(35.7) 58/196(29.6) χ2=0.434 0.510 骨质疏松 13 4/28(14.3) 9/196(4.6) χ2=2.625 0.105 其他 35 6/28(21.4) 29/196(14.7) χ2=0.818 0.366 结局[例(%)] HCC 10 4/48(8.3) 6/350(1.7) χ2=5.090 0.024 肝移植 17 2/48(4.2) 15/350(4.3) χ2=0.052 0.820 肝病相关死亡 36 7/48(14.6) 29/350(8.3) χ2=2.035 0.154 死亡或接受肝移植年龄(岁) 36 31.5±15.9 53.9±12.6 t=3.798 0.001 死亡或肝移植患者总生存期(月) 36 41.8±37.2 44.9±53.9 t=0.137 0.891 表 6 影响AIH患者预后的高危因素
因素 HR 95%CI P值 男性 肝硬化 3.250 1.356~7.793 0.008 糖尿病 17.532 1.638~18.611 0.018 Alb<31.4 g/L 32.518 2.264~46.109 0.010 女性 肝硬化 2.923 1.251~6.828 0.013 肝衰竭 3.355 1.340~8.397 0.010 ANA≥1∶1000 0.045 0.003~0.625 0.021 DBil>42 μmol/L 0.344 0.128~0.926 0.035 LY<1.2×109/L 5.408 1.776~16.464 0.003 C3<0.588 g/L 4.043 1.559~10.480 0.004 -
[1] European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Autoimmune hepatitis[J]. J Hepatol, 2015, 63(4): 971-1004. DOI: 10.1016/j.jhep.2015.06.030. [2] TAUBERT R, JAECKEL E. Autoimmunhepatitis-Standard- und Zweitlinientherapie [Autoimmune hepatitis-standard and second-line therapy][J]. Internist (Berl), 2018, 59(6): 536-543. DOI: 10.1007/s00108-018-0434-1. [3] PUUSTINEN L, BOYD S, MUSTONEN H, et al. Prognostic value of clinical variables and liver histology for development of fibrosis and cirrhosis in autoimmune hepatitis[J]. Scand J Gastroenterol, 2017, 52(3): 321-327. DOI: 10.1080/00365521.2016.1253768. [4] ∅RSTAVIK KH. Why are autoimmune diseases more prevalent in women?[J]. Tidsskr Nor Laegeforen, 2017, 137(12-13): 866-868. DOI: 10.4045/tidsskr.16.0935. [5] LIBERT C, DEJAGER L, PINHEIRO I. The X chromosome in immune functions: When a chromosome makes the difference[J]. Nat Rev Immunol, 2010, 10(8): 594-604. DOI: 10.1038/nri2815. [6] MOULTON VR. Sex hormones in acquired Immunity and autoimmune disease[J]. Front Immunol, 2018, 9: 2279. DOI: 10.3389/fimmu.2018.02279. [7] RIBBONS KA, MCELDUFF P, BOZ C, et al. Male sex is independently associated with faster disability accumulation in relapse-onset MS but not in primary progressive MS[J]. PLoS One, 2015, 10(6): e0122686. DOI: 10.1371/journal.pone.0122686. [8] ABDULKARIM M, ZENOUZI R, SEBODE M, et al. Sex differences in clinical presentation and prognosis in patients with primary biliary cholangitis[J]. Scand J Gastroenterol, 2019, 54(11): 1391-1396. DOI: 10.1080/00365521.2019.1683226. [9] LUCEY MR, NEUBERGER JM, WILLIAMS R. Primary biliary cirrhosis in men[J]. Gut, 1986, 27(11): 1373-1376. DOI: 10.1136/gut.27.11.1373. [10] SAYINER M, GOLABI P, STEPANOVA M, et al. Primary biliary cholangitis in medicare population: The impact on mortality and resource use[J]. Hepatology, 2019, 69(1): 237-244. DOI: 10.1002/hep.30174. [11] SHAHARIR SS, KADIR WDA, NORDIN F, et al. Systemic lupus erythematosus among male patients in Malaysia: How are we different from other geographical regions?[J]. Lupus, 2019, 28(1): 137-144. DOI: 10.1177/0961203318812676. [12] AL-CHALABI T, UNDERHILL JA, PORTMANN BC, et al. Impact of gender on the long-term outcome and survival of patients with autoimmune hepatitis[J]. J Hepatol, 2008, 48(1): 140-147. DOI: 10.1016/j.jhep.2007.08.013. [13] MONTANO-LOZA AJ, CARPENTER HA, CZAJA AJ. Predictive factors for hepatocellular carcinoma in type 1 autoimmune hepatitis[J]. Am J Gastroenterol, 2008, 103(8): 1944-1951. DOI: 10.1111/j.1572-0241.2008.01922.x. [14] DONET JA, PERLINI EF, GILINSKY D, et al. Impact of gender on clinical presentation, response to treatment, and long-term outcomes in an ethnically diverse population of patients with autoimmune hepatitis[J]. J Hepatol, 2016, 64(2): s439. http://www.researchgate.net/publication/308577254_Impact_of_Gender_on_Clinical_Presentation_Response_to_Treatment_and_Long-Term_Outcomes_in_an_Ethnically_Diverse_Population_of_Patients_with_Autoimmune_Hepatitis [15] HENNES EM, ZENIYA M, CZAJA AJ, et al. Simplified criteria for the diagnosis of autoimmune hepatitis[J]. Hepatology, 2008, 48(1): 169-176. DOI: 10.1002/hep.22322. [16] ALVAREZ F, BERG PA, BIANCHI FB, et al. International Autoimmune Hepatitis Group Report: Review of criteria for diagnosis of autoimmune hepatitis[J]. J Hepatol, 1999, 31(5): 929-938. DOI: 10.1016/s0168-8278(99)80297-9. [17] WEILER-NORMANN C, SCHRAMM C. Drug induced liver injury and its relationship to autoimmune hepatitis[J]. J Hepatol, 2011, 55(4): 747-749. DOI: 10.1016/j.jhep.2011.02.024. [18] YEONG TT, LIM KH, GOUBET S, et al. Natural history and outcomes in drug-induced autoimmune hepatitis[J]. Hepatol Res, 2016, 46(3): e79-e88. DOI: 10.1111/hepr.12532. [19] CHAZOUILLÈRES O, WENDUM D, SERFATY L, et al. Primary biliary cirrhosis-autoimmune hepatitis overlap syndrome: Clinical features and response to therapy[J]. Hepatology, 1998, 28(2): 296-301. DOI: 10.1002/hep.510280203. [20] BOBERG KM, CHAPMAN RW, HIRSCHFIELD GM, et al. Overlap syndromes: The International Autoimmune Hepatitis Group (IAIHG) position statement on a controversial issue[J]. J Hepatol, 2011, 54(2): 374-385. DOI: 10.1016/j.jhep.2010.09.002. [21] FUKUI H, SAITO H, UENO Y, et al. Evidence-based clinical practice guidelines for liver cirrhosis 2015[J]. J Gastroenterol, 2016, 51(7): 629-650. DOI: 10.1007/s00535-016-1216-y. [22] GRR∅NBAK L, VILSTRUP H, JEPSEN P. Autoimmune hepatitis in Denmark: Incidence, prevalence, prognosis, and causes of death. A nationwide registry-based cohort study[J]. J Hepatol, 2014, 60(3): 612-617. DOI: 10.1016/j.jhep.2013.10.020. [23] XUE M, SHEN Y, SHEN MY, et al. Autoimmune hepatitis-related autoantibodies and their clinical significance[J]. J Clin Hepatol, 2019, 35(6): 1392-1396. DOI: 10.3969/j.issn.1001-5256.2019.06.048.雪梅, 沈怡, 沈梦益, 等. 自身免疫性肝炎相关自身抗体及临床意义[J]. 临床肝胆病杂志, 2019, 35(6): 1392-1396. DOI: 10.3969/j.issn.1001-5256.2019.06.048. [24] ZHANG WC, ZHAO FR, CHEN J, et al. Meta-analysis: Diagnostic accuracy of antinuclear antibodies, smooth muscle antibodies and antibodies to a soluble liver antigen/liver pancreas in autoimmune hepatitis[J]. PLoS One, 2014, 9(3): e92267. DOI: 10.1371/journal.pone.0092267. [25] CZAJA AJ. Behavior and significance of autoantibodies in type 1 autoimmune hepatitis[J]. J Hepatol, 1999, 30(3): 394-401. DOI: 10.1016/s0168-8278(99)80096-8. [26] DINSER R, BRAUN A, JENDRO MC, et al. Increased titres of anti-nuclear antibodies do not predict the development of associated disease in the absence of initial suggestive signs and symptoms[J]. Scand J Rheumatol, 2007, 36(6): 448-451. DOI: 10.1080/03009740701406577. [27] VALGEIRSSON KB, HREINSSON JP, BJÖRNSSON ES. Increased incidence of autoimmune hepatitis is associated with wider use of biological drugs[J]. Liver Int, 2019, 39(12): 2341-2349. DOI: 10.1111/liv.14224. [28] FLOREANI A, DE MARTIN S, SECCHI MF, et al. Extrahepatic autoimmunity in autoimmune liver disease[J]. Eur J Intern Med, 2019, 59: 1-7. DOI: 10.1016/j.ejim.2018.10.014. [29] MURATORI P, FABBRI A, LALANNE C, et al. Autoimmune liver disease and concomitant extrahepatic autoimmune disease[J]. Eur J Gastroenterol Hepatol, 2015, 27(10): 1175-1179. DOI: 10.1097/MEG.0000000000000424. [30] WONG GW, YEONG T, LAWRENCE D, et al. Concurrent extrahepatic autoimmunity in autoimmune hepatitis: Implications for diagnosis, clinical course and long-term outcomes[J]. Liver Int, 2017, 37(3): 449-457. DOI: 10.1111/liv.13236. [31] GOWER E, ESTES C, BLACH S, et al. Global epidemiology and genotype distribution of the hepatitis C virus infection[J]. J Hepatol, 2014, 61(1 Suppl): S45-S57. DOI: 10.1016/j.jhep.2014.07.027. [32] REZAEE ZAVAREH MS, ALAVIAN SM, KARIMISARI H, et al. Occult hepatitis C virus infection in patients with autoimmune hepatitis[J]. Hepat Mon, 2014, 14(8): e16089. DOI: 10.5812/hepatmon.16089. [33] MENG J. Epidemiological survey of hepatitis B virus infection in hospitals: A cross-sectional study[D]. Changchun: Jilin University, 2016.孟静. 乙型肝炎病毒感染医院流行病学调查: 一项横断面研究y[D]. 长春: 吉林大学, 2016. [34] TAUBERT R, DIESTELHORST J, JUNGE N, et al. Increased seroprevalence of HAV and parvovirus B19 in children and of HEV in adults at diagnosis of autoimmune hepatitis[J]. Sci Rep, 2018, 8(1): 17452. DOI: 10.1038/s41598-018-35882-7. [35] PARKER R, OO YH, ADAMS DH. Management of patients with difficult autoimmune hepatitis[J]. Therap Adv Gastroenterol, 2012, 5(6): 421-437. DOI: 10.1177/1756283X12450251. [36] TANSEL A, KATZ LH, EL-SERAG HB, et al. Incidence and determinants of hepatocellular carcinoma in autoimmune hepatitis: A systematic review and meta-analysis[J]. Clin Gastroenterol Hepatol, 2017, 15(8): 1207-1217.e4. DOI: 10.1016/j.cgh.2017.02.006. -



 PDF下载 ( 2040 KB)
PDF下载 ( 2040 KB)

 下载:
下载:


