Application of transjugular liver biopsy in the diagnosis and treatment of complicated and severe liver diseases
-
摘要:
目的 探讨经颈静脉肝穿刺活检(TJLB)在疑难重症肝病诊断及治疗中应用的意义。 方法 回顾性分析2016年1月-2021年5月在解放军总医院第五医学中心接受TJLB的31例患者的临床资料,对穿刺的适应证、成功率、最终诊断结果进行分析。 结果 31例患者中男15例,女16例。8例因肝衰竭凝血机制障碍、13例因肝硬化合并腹水、10例因肝硬化合并血小板减少(<50×109/L)不宜行经皮肝穿刺活检,符合实施TJLB适应证。TJLB穿刺成功率100%,穿刺条数2~4条。无严重不良事件。患者出院明确诊断26例(83.87%)。其中特发性门静脉高压5例,药物性肝衰竭或肝硬化9例,自身免疫性肝病5例,其他原因肝硬化或肝衰竭7例,尚不能明确病因者5例,此外,为证实诊断及决策是否肝移植患者3例。 结论 TJLB在疑难重症肝病诊治中发挥重要作用,但尚有一定局限性,临床上应注意筛选适宜患者实施。 Abstract:Objective To investigate the application value of transjugular liver biopsy (TJLB) in the diagnosis and treatment of complicated and severe liver diseases. Methods A retrospective analysis was performed for the clinical data of 31 patients who underwent TJLB in The Fifth Medical Center of Chinese PLA General Hospital, including indication for puncture, success rate, and final diagnosis. Results Among the 31 patients, there were 15 male patients and 16 female patients. Percutaneous liver biopsy was unsuitable for 8 patients with liver failure and disturbances of blood coagulation, 13 with liver cirrhosis and ascites, and 10 with liver cirrhosis and thrombocytopenia (< 50×109/L), which were the indications for TJLB. The success rate of TJLB puncture was 100%, with 2-4 passes for puncture. No serious adverse event was observed. Of all 31 patients, 26 (83.87%) had a definite diagnosis at discharge, among whom there were 5 patients with idiopathic portal hypertension, 9 patients with drug-induced liver failure or liver cirrhosis, 5 patients with autoimmune liver disease, and 7 patients with liver cirrhosis or liver failure due to other causes, and 5 patients had unknown etiology. In addition, 3 patients underwent biopsy to confirm the diagnosis and decision of whether liver transplantation should be performed. Conclusion TJLB plays an important role in the diagnosis and treatment of complicated and severe liver diseases and still has certain limitations, and therefore, suitable patients should be selected in clinical practice. -
Key words:
- Liver Diseases /
- Biopsy, Needle /
- Diagnosis /
- Therapeutics
-
肝组织病理学检查是疑难肝病诊治的关键技术,获得肝组织的活检方法常规为经皮肝穿刺活检(percutaneous liver biopsy, PLB),此外,在一些特殊患者中,还可以通过经颈静脉肝穿刺活检(transjugular liver biopsy, TJLB)、腹腔镜下肝活检等方式获得。对于凝血机制障碍或肝硬化腹水患者,TJLB是一种更安全的选择[1]。本研究拟通过对实施TJLB患者的临床资料进行回顾性分析,探讨TJLB在疑难重症肝病诊治中的应用。
1. 资料和方法
1.1 研究对象
收集2016年1月-2021年5月在本院实施TJLB患者的临床资料。所有患者在入院后行血常规、凝血酶原活动度(PTA)、国际标准化比值(INR)、肝脏生化指标、肝炎病毒学指标等化验,行肝胆脾彩超或CT/MRI检查。所有患者因肝衰竭或肝硬化合并腹水不宜行PLB检查,符合TJLB适应证[2-3]。
1.2 仪器与设备
LABS-200肝内穿刺活检针套装购自美国Cook公司; Fogarty 5.5F球囊导管购自美国爱德华公司; 10F血管鞘组、0.035inch-183超滑导丝、Terumo 5F导管购自日本Terumo公司; 心电测压仪购自美国飞利浦公司。
1.3 TJLB检测过程
术前充分询问病史,排除既往心脏病史患者,仔细阅览患者影像资料,确认肝静脉及下腔静脉无明显狭窄或阻塞。告知患者手术适应证及可能风险,签署知情同意书。按照TJLB标准操作流程实施肝穿刺[2, 4],并行肝静脉压力梯度测定。每次穿刺后观察组织标本完整程度,必要时反复穿刺,直至获取到满意组织标本。术中均行心电监护。所有肝穿刺标本直接放入4%甲醛溶液中,送至病理科进行组织病理检查。
2. 结果
2.1 一般资料
共纳入31例患者,男15例,女16例,中位年龄44(22~74)岁。其中8例因肝衰竭凝血机制障碍、13例因肝硬化合并腹水、10例因肝硬化合并血小板减少(<50×109/L)不宜行PLB,符合实施TJLB适应证。相关化验指标见表 1。
表 1 患者相关化验指标指标 数值 Alb(g/L) 33.00(28.00~37.00) ALT(U/L) 33.00(18.00~63.00) AST(U/L) 49.00(35.00~140.00) ALP(U/L) 149.00(84.00~266.00) GGT(U/L) 98.00(27.00~156.00) TBil(μmol/L) 57.30(18.10~164.60) PTA(%) 52.90(42.90~70.60) INR 1.37(1.13~1.58) WBC(×109/L) 3.38(2.14~5.30) Hb(g/L) 105.00(93.00~124.00) PLT(×109/L) 68.00(47.00~118.00) 注:数据描述方式为M (P25~P75)。 2.2 行TJLB的情况
30例患者顺利实施TJLB,1例因肝静脉与下腔静脉夹角过小,穿刺进针阻力较大,击发困难,手术时间延长。穿刺针次为2~4次不等,获取肝组织2~4条,其中最长单条长度为20 mm,满足完整汇管区数量>6个的病理检测要求[5]。术中患者疼痛表现,按长海痛尺评分,5分以下的15例(48.39%),5~8分16例(51.61%),无高于8分或不可耐受患者。术中一过性心律失常8例(25.81%)。所有患者给予肝穿刺术后常规护理,监测生命体征及血氧饱和度未见异常。术后复查血常规、凝血、生化指标与术前相比没有明显变化。术后穿刺部位无瘀斑、血肿情况发生,肝区不适5例(16.13%),一周内均可自行恢复。
22例(70.97%)患者在穿刺前进行肝静脉压力梯度测定,肝静脉楔压为15.0~52.8 cmH2O,肝静脉自由压为7.0~23 cmH2O,计算肝静脉压力梯度(hepatic venous pressure gradient,HVPG)为8.2~34.3 cmH2O。
2.3 疾病诊断情况
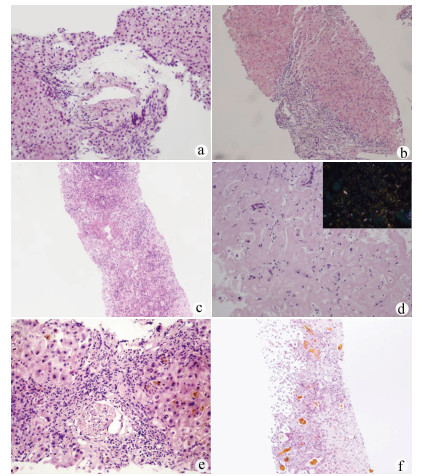
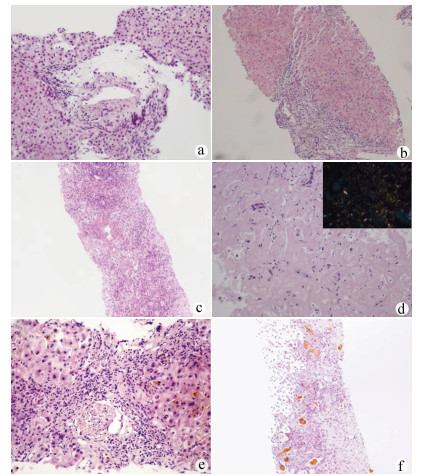
在肝穿刺病理诊断辅助下,患者出院明确诊断26例(83.87%),其中特发性门静脉高压(idiopathic portal hypertension,IPH)5例,代表病例1:女,39岁,入院诊断“门静脉高压、腹水”(图 1a),结合临床诊断IPH。药物性肝衰竭或肝硬化9例,代表病例2:男,34岁,入院诊断“肝硬化失代偿期”(图 1b),结合临床诊断药物性肝衰竭肝损伤。自身免疫性肝脏疾病包括原发性胆汁性胆管炎(PBC)、自身免疫性肝炎(AIH)、重叠综合征,以及小胆管型原发性硬化性胆管炎(PSC)共5例,代表病例3:女,33岁,入院诊断“乙型肝炎肝衰竭”(图 1c),结合临床诊断AIH慢加急性肝衰竭、乙型肝炎肝硬化。其他原因肝硬化或肝衰竭患者7例,包括肝豆状核变性1例、甲状腺功能减退相关肝硬化1例、肝淀粉样变2例、阻塞性胆管炎1例、酒精性肝衰竭合并溶血性疾病1例,辅助排除肝脏肿瘤1例,代表病例4:男,74岁,入院诊断“肝硬化,布加综合征?”(图 1d),结合临床诊断肝淀粉样变性。尚不能明确病因患者5例(16.13%),代表病例5:男,72岁,入院诊断“肝功能异常,原因待查,腹水”,无明确药物应用史(图 1e)。病理会诊不能明确病因,治疗无效。临床诊断不明原因肝衰竭。此外,为证实诊断及决策是否肝移植患者3例,代表病例6:男,23岁,入院诊断“急性肝衰竭”。结合临床诊断急性药物性肝衰竭,3次人工肝治疗,病情无好转拟行肝移植,肝穿刺后结合病理结果决定保守治疗(图 1f),后经治疗病情好转。
3. 讨论
临床工作中约有20%的肝衰竭或肝硬化患者由于凝血机制障碍或腹水不能实施经PLB获取肝组织行病理检查[6],从而影响疾病的诊治。全球范围内不明原因肝衰竭的占比为10%~50%[7-8]。随着我国人民生活水平的提高,乙型肝炎肝衰竭占比逐年下降,不明原因肝衰竭的占比呈逐年升高趋势,迫切需要病理检查辅助提高疑难重症肝病的确诊率。TJLB因其可克服出血的优势,提供了重症肝病患者病理检测手段。
本研究纳入的31例患者中5例明确诊断IPH。IPH的发病机制目前未完全清楚,缺乏特异的检测指标,临床诊断较困难,肝活检对于IPH的诊断尤为重要[9-11]。IPH患者一般以肝硬化致门静脉高压合并腹水、消化道出血等起病,失去实施PLB时机,而临床无病理检查诊断较为困难。该组患者16.13%明确诊断为IPH,提示TJLB为隐源性肝硬化患者中IPH的诊断提供了重要手段。药物性肝炎诊断中,肝脏病理检查并不是必要条件,但需要排除其他疾病,特别是需与自身免疫性肝病进行鉴别,而非典型AIH的诊断,肝脏病理检查是必需的[12],因此对于药物性肝损伤的患者病理检查有时格外重要。该组9例患者经病理协助明确诊断药物性肝炎(29.03%),为后续治疗提供帮助。非典型自身免疫性肝脏疾病包括PBC、AIH、重叠综合征、PSC等,这类疾病的诊断依赖病理检查,同时,相关重症患者是否启用激素治疗是救治成功的关键,而激素治疗方案的制订需要病理辅助。该组患者协助明确诊断2例非典型PBC、2例非典型AIH及1例小胆管型PSC,并指导治疗获得较好的临床疗效。肝衰竭的早期精准预后相当重要,特别是指导选择内科保守治疗还是肝移植方面对患者尤为关键,且肝移植的时机也是术后良好恢复的重要参考指标。虽然临床上有较多的模型及指标进行预后判定,但肝脏病理在肝衰竭精准预后方面发挥重要作用,该组患者经过检查有3例患者改变了治疗方式的选择,精准指导肝移植治疗方案的制定。另外,通过肝穿刺病理检查可协助肝硬化晚期或肝衰竭患者确诊罕见病例,包括肝豆状核变性、甲状腺功能减退相关肝硬化、肝淀粉样变性等。
TJLB在获取肝组织行病理检查协助诊断的同时,可进行HVPG测定,获得血液动力学参数,对于确定是否存在门静脉高压,以及属于窦前、窦性、窦后哪一种类型,有较好的提示意义[13]。本组患者进行HVPG测量对门静脉高压的诊断起到了辅助作用,但HVPG的测量受体位、管路、肝内分流、导管位置等因素影响[14],测量数据可能欠精确,因此测量数值偏差较大,在今后的扩大研究中应注意对同类患者探索对应的分级标准,以便更好的协助诊断和评估预后。
病理检查在评价肝脏病理严重程度方面较为精准,在医学诊断中俗有“金标准”的地位[15],但是在病因确认方面尚有一定的局限性。一方面缘于病理损害缺乏特征性改变,对于某些肝硬化患者,肝组织病理检查可明确肝纤维化及肝脏炎症程度,但可能无法观察到疾病典型病理特征,不能提出明确的临床诊断。另一方面可能与临床医师及病理医师的知识面不够全面有关。有时肝组织病理检查只是起到排除诊断和提供诊断线索的作用,因此,病理检查只是提供诊断依据的辅助手段,而非临床最终诊断。疑难肝病的诊断需要临床医师具有全面的医学知识和丰富的临床经验,提供病理科医师更全面的信息,并结合其他检查方法,如骨髓穿刺、基因检测、血管成像等才能最终明确。TJLB费用相对较高,且也许不能获得良好预期,临床医师应严格掌握适应证,避免医疗纠纷。
该组患者肝组织获取成功率为100%,无明显不良反应,且获取肝组织基本符合病理检测要求,提示TJLB手术成功率较高。据文献[16-17]报道,仍有少数患者组织获取质量欠佳。一方面,实施TJLB的患者部分为肝衰竭患者,肝组织炎症水肿明显,获取肝组织过程中容易破碎; 另一方面,部分为肝硬化患者,肝组织纤维化严重,获取肝组织时受纤维组织的牵拉,组织容易断裂,获取的肝组织有时难以达到病理检测的要求,影响病理医师的判定,因此术中应注意观察获取的组织质量,必要时需反复穿刺。
TJLB为肝硬化合并腹水、肝衰竭及凝血机制障碍的肝病患者提供了肝组织获取的方法,同时可进行HVPG测定,对协助疑难重症肝病诊断及评估预后发挥重要作用,但尚有一定局限性,临床上应注意筛选适宜患者实施。
-
表 1 患者相关化验指标
指标 数值 Alb(g/L) 33.00(28.00~37.00) ALT(U/L) 33.00(18.00~63.00) AST(U/L) 49.00(35.00~140.00) ALP(U/L) 149.00(84.00~266.00) GGT(U/L) 98.00(27.00~156.00) TBil(μmol/L) 57.30(18.10~164.60) PTA(%) 52.90(42.90~70.60) INR 1.37(1.13~1.58) WBC(×109/L) 3.38(2.14~5.30) Hb(g/L) 105.00(93.00~124.00) PLT(×109/L) 68.00(47.00~118.00) 注:数据描述方式为M (P25~P75)。 -
[1] BRAVO AA, SHETH SG, CHOPRA S. Liver biopsy[J]. N Engl J Med, 2001, 344(7): 495-500. DOI: 10.1056/NEJM200102153440706. [2] DOHAN A, GUERRACHE Y, BOUDIAF M, et al. Transjugular liver biopsy: Indications, technique and results[J]. Diagn Interv Imaging, 2014, 95(1): 11-15. DOI: 10.1016/j.diii.2013.08.009. [3] CADRANEL JF, NOUSBAUM JB, GOUILLOU M, et al. Major changes in the number and indications of liver biopsy for chronic liver diseases over one decade in France[J]. Eur J Gastroenterol Hepatol, 2016, 28(9): e26-e32. DOI: 10.1097/MEG.0000000000000683. [4] LYU S, YOU SL, YU Q, et al. Feasibility and significance of transjugular liver biopsy in diagnosis and treatment of complicated and severe liver diseases: A single-center analysis of 5 cases[J]. Chin J Hepatol, 2017, 25(10): 772-774. DOI: 10.3760/cma.j.issn.1007-3418.2017.10.011.吕飒, 游绍莉, 余强, 等. 经颈静脉肝穿刺活组织检查在疑难重症肝病诊治中的可行性及意义: 单中心5例患者分析[J]. 中华肝脏病杂志, 2017, 25(10): 772-774. DOI: 10.3760/cma.j.issn.1007-3418.2017.10.011. [5] CRAWFORD AR, LIN XZ, CRAWFORD JM. The normal adult human liver biopsy: A quantitative reference standard[J]. Hepatology, 1998, 28(2): 323-331. DOI: 10.1002/hep.510280206. [6] YOU SL, ZHU B, RONG YH, et al. Diagnosis analysis of 9453 cases with liver diseases[J]. Chin J Health Care Med, 2012, 14(6): 459-462. DOI: 10.3969/j.issn.1674-3245.2012.06.017.游绍莉, 朱冰, 荣义辉, 等. 9453例待查肝病的诊断分析[J]. 中华保健医学杂志, 2012, 14(6): 459-462. DOI: 10.3969/j.issn.1674-3245.2012.06.017. [7] BERNAL W, WENDON J. Acute liver failure[J]. N Engl J Med, 2013, 369(26): 2525-2534. DOI: 10.1056/NEJMra1208937. [8] YOU S, RONG Y, ZHU B, et al. Changing etiology of liver failure in 3, 916 patients from northern China: A 10-year survey[J]. Hepatol Int, 2013, 7(2): 714-720. DOI: 10.1007/s12072-013-9424-5. [9] European Association for the Study of the Liver. EASL clinical practice guidelines: Vascular diseases of the liver[J]. J Hepatol, 2016, 64(1): 179-202. DOI: 10.1016/j.jhep.2015.07.040. [10] KHANNA R, SARIN SK. Non-cirrhotic portal hypertension-diagnosis and management[J]. J Hepatol, 2014, 60(2): 421-441. DOI: 10.1016/j.jhep.2013.08.013. [11] REN Y, ZHENG SJ. Progress of idiopathic portal hypertension[J]. Chin J Gastroenterol Hepatol, 2019, 28(6): 708-710. DOI: 10.3969/j.issn.1006-5709.2019.06.025.任艳, 郑素军. 特发性门脉高压研究现状[J]. 胃肠病学和肝病学杂志, 2019, 28(6): 708-710. DOI: 10.3969/j.issn.1006-5709.2019.06.025. [12] MACK CL, ADAMS D, ASSIS DN, et al. Diagnosis and management of autoimmune hepatitis in adults and children: 2019 practice guidance and guidelines from the American Association for the Study of Liver Diseases[J]. Hepatology, 2020, 72(2): 671-722. DOI: 10.1002/hep.31065. [13] ZHAO LH, JIA JD. Etiological diagnosis and standard treatment of portal hypertension should be taken seriously[J]. J Clin Hepatol, 2019, 35(1): 10-12. DOI: 10.3969/j.issn.1001-5256.2019.01.001.赵连晖, 贾继东. 应重视门静脉高压症的病因诊断及规范治疗[J]. 临床肝胆病杂志, 2019, 35(1): 10-12. DOI: 10.3969/j.issn.1001-5256.2019.01.001. [14] Chinese Portal Hypertension Diagnosis and Monitoring Study Group (CHESS), Minimally Invasive Intervention Collaborative Group, Chinese Society of Gastroenterology, Emergency Intervention Committee, Chinese College of Interventionalists, et al. Consensus on clinical application of hepatic venous pressure gradient in China (2018)[J]. J Clin Hepatol, 2018, 34(12): 2526-2536. DOI: 10.3969/j.issn.1001-5256.2018.12.008.中国门静脉高压诊断与监测研究组(CHESS), 中华医学会消化病学分会微创介入协作组, 中国医师协会介入医师分会急诊介入专业委员会, 等. 中国肝静脉压力梯度临床应用专家共识(2018版)[J]. 临床肝胆病杂志, 2018, 34(12): 2526-2536. DOI: 10.3969/j.issn.1001-5256.2018.12.008. [15] ROCKEY DC, CALDWELL SH, GOODMAN ZD, et al. Liver biopsy[J]. Hepatology, 2009, 49(3): 1017-1044. DOI: 10.1002/hep.22742. [16] BEHRENS G, FERRAL H. Transjugular liver biopsy[J]. Semin Intervent Radiol, 2012, 29(2): 111-117. DOI: 10.1055/s-0032-1312572. [17] BEHRENS G, FERRAL H, GIUSTO D, et al. Transjugular liver biopsy: Comparison of sample adequacy with the use of two automated needle systems[J]. J Vasc Interv Radiol, 2011, 22(3): 341-345. DOI: 10.1016/j.jvir.2010.10.012. 期刊类型引用(3)
1. 张兆辉,庄轶超,杨文宪. 瞬时弹性成像技术对原发性胆汁性肝硬化、自身免疫性肝炎的鉴别及与肝脏纤维化程度、肝功能的相关性研究. 世界华人消化杂志. 2023(11): 464-469 .  百度学术
百度学术2. 曾意君,蔡晶晶,蔡慧琳,林瑞冰,邓小艳,刘朝阳. 海珠区青年体检人群非酒精性脂肪肝病变程度与血脂、血糖的相关性. 现代养生. 2022(12): 1000-1002 .  百度学术
百度学术3. 张文广,齐县伟,张敬强,田振华,陈鹏飞,周学良,李方正,牛勇,任建庄,韩新巍. 经颈静脉肝内穿刺活检对不明原因肝病患者的应用价值. 中华肝胆外科杂志. 2022(09): 651-655 .  百度学术
百度学术其他类型引用(0)
-




 PDF下载 ( 2586 KB)
PDF下载 ( 2586 KB)

 下载:
下载:

 下载:
下载:
 百度学术
百度学术