Research advances in intraductal papillary mucinous neoplasm of the bile tract
-
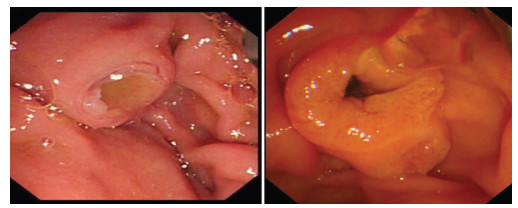
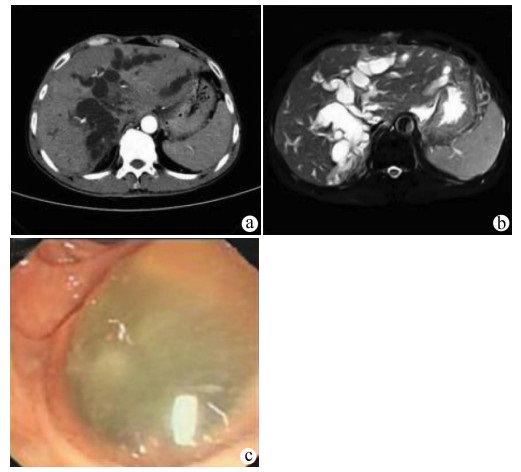
摘要: 胆管导管内乳头状黏液性肿瘤(IPMN-B)是发生在胆管系统的一类特殊肿瘤,其临床表现及影像学均无特异性,术前诊断困难,往往于术中发现胆管内充盈大量黏液时考虑本病而被迫临时改变手术方案。由于其发病率低,临床医师对其缺乏认识。综述了近年来IPMN-B的病因与分型、临床特征、鉴别诊断、治疗及预后等方面研究进展,以期提高临床医师对IPMN-B的诊疗水平。Abstract: Intraductal papillary mucinous neoplasm of the bile duct (IPMN-B) is a special type of tumor occurring in the biliary system, with no specific clinical manifestations and imaging findings, and thus it is difficult to diagnose before surgery. It is often considered when a large amount of mucus is found in the bile duct during surgery and then it is forced to change the surgical plan. Clinicians lack an understanding of this disease due to its low incidence rate. This article reviews the recent research advances in the etiology and classification, clinical features, differential diagnosis, treatment, and prognosis of IPMN-B, so as to improve the clinical diagnosis and treatment of IPMN-B among clinicians.
-
Key words:
- Bile Duct Neoplasms /
- Therapeutics /
- Prognosis
-
表 1 IPMN-B的免疫组化分型
分型 MUC1 MUC2 MUC5AC MUC6 肠型 - + + - 胃型 - - + + 胰胆管型 + - + - 嗜酸性细胞型 + - + + 表 2 IPMN-B的影像学分型
分型 特征 典型IPMN-B 胆管内肿瘤灶和肿瘤上、下游胆管均明显扩张 囊性IPMN-B 胆管呈局限性囊状扩张,表现为囊性肿块,囊内可见瘤灶,可单发或多发 无肿块型IPMN-B 肝内外胆管均明显扩张,未见明显瘤灶和囊性肿块 侵袭型IPMN-B 瘤体不仅向腔内乳头状生长而且突破胆管壁向外浸润胆管周围组织 -
[1] KIM HJ, KIM MH, LEE SK, et al. Mucin-hypersecreting bile duct tumor characterized by a striking homology with an intraductal papillary mucinous tumor (IPMT) of the pancreas[J]. Endoscopy, 2000, 32(5): 389-393. DOI: 10.1055/s-2000-8996. [2] PARK HJ, KIM SY, KIM HJ, et al. Intraductal papillary neoplasm of the bile duct: Clinical, imaging, and pathologic features[J]. AJR Am J Roentgenol, 2018, 211(1): 67-75. DOI: 10.2214/AJR.17.19261. [3] PAIK KY, HEO JS, CHOI SH, et al. Intraductal papillary neoplasm of the bile ducts: The clinical features and surgical outcome of 25 cases[J]. J Surg Oncol, 2008, 97(6): 508-512. DOI: 10.1002/jso.20994. [4] CAI HQ, GENG ZM. Research progress of intradutal papillary neoplasm of the bile duct[J]. Chin J Dig Surg, 2017, 16(8): 879-882. DOI: 10.3760/cma.j.issn.1673-9752.2017.08.024.蔡慧强, 耿智敏. 胆管内乳头状肿瘤的研究进展[J]. 中华消化外科杂志, 2017, 16(8): 879-882. DOI: 10.3760/cma.j.issn.1673-9752.2017.08.024. [5] ZACCARI P, CARDINALE V, SEVERI C, et al. Common features between neoplastic and preneoplastic lesions of the biliary tract and the pancreas[J]. World J Gastroenterol, 2019, 25(31): 4343-4359. DOI: 10.3748/wjg.v25.i31.4343. [6] VALENTE R, CAPURSO G, PIERANTOGNETTI P, et al. Simultaneous intraductal papillary neoplasms of the bile duct and pancreas treated with chemoradiotherapy[J]. World J Gastrointest Oncol, 2012, 4(2): 22-25. DOI: 10.4251/wjgo.v4.i2.22. [7] WU XR, ZHAO S, MIAO L, et al. A case report of mucinous papillary adenocarcinoma of extrahepatic bile duct with colloid carcinoma infiltration and recurrent choledocholithiasis[J]. Chin J Dig Endosc, 2020, 37(10): 757-758. DOI: 10.3760/cma.j.cn321463-20190528-00378.巫雪茹, 赵思, 缪林, 等. 肝外胆管黏液性乳头状腺癌伴胶样癌浸润合并复发性胆总管结石一例[J]. 中华消化内镜杂志, 2020, 37(10): 757-758. DOI: 10.3760/cma.j.cn321463-20190528-00378. [8] ROCHA FG, LEE H, KATABI N, et al. Intraductal papillary neoplasm of the bile duct: A biliary equivalent to intraductal papillary mucinous neoplasm of the pancreas?[J]. Hepatology, 2012, 56(4): 1352-1360. DOI: 10.1002/hep.25786. [9] WANG X, CAI YQ, CHEN YH, et al. Biliary tract intraductal papillary mucinous neoplasm: Report of 19 cases[J]. World J Gastroenterol, 2015, 21(14): 4261-4267. DOI: 10.3748/wjg.v21.i14.4261. [10] WANG SD, WANG XW, LIU GH, et al. Research advances in intradutal papillary neoplasm of the bile duct[J]. J Clin Hepatol, 2020, 36(2): 476-480. DOI: 10.3969/j.issn.1001-5256.2020.02.054.王士东, 王小玮, 刘国红, 等. 胆管内乳头状肿瘤的研究现状[J]. 临床肝胆病杂志, 2020, 36(2): 476-480. DOI: 10.3969/j.issn.1001-5256.2020.02.054. [11] WHITE AD, YOUNG AL, VERBEKE C, et al. Biliary papillomatosis in three Caucasian patients in a Western centre[J]. Eur J Surg Oncol, 2012, 38(2): 181-184. DOI: 10.1016/j.ejso.2011.11.007. [12] YANG X, ZHOU X, HU CY, et al. Intraductal papillary neoplasm of intrahepatic bile duct: One case report[J]. Chin J Gastroenterol and Hepatol, 2020, 29(12): 1383-1385. DOI: 10.3969/j.issn.1006-5709.2020.12.013.杨潇, 周晓, 胡春阳, 等. 肝内胆管导管内乳头状肿瘤1例报道[J]. 胃肠病学和肝病学杂, 2020, 29(12): 1383-1385. DOI: 10.3969/j.issn.1006-5709.2020.12.013. [13] BENNETT S, MARGINEAN EC, PAQUIN-GOBEIL M, et al. Clinical and pathological features of intraductal papillary neoplasm of the biliary tract and gallbladder[J]. HPB (Oxford), 2015, 17(9): 811-818. DOI: 10.1111/hpb.12460. [14] OHTSUKA M, KIMURA F, SHIMIZU H, et al. Similarities and differences between intraductal papillary tumors of the bile duct with and without macroscopically visible mucin secretion[J]. Am J Surg Pathol, 2011, 35(4): 512-521. DOI: 10.1097/PAS.0b013e3182103f36. [15] KIM KM, LEE JK, SHIN JU, et al. Clinicopathologic features of intraductal papillary neoplasm of the bile duct according to histologic subtype[J]. Am J Gastroenterol, 2012, 107(1): 118-125. DOI: 10.1038/ajg.2011.316. [16] LI RR, CHEN YY, ZHOU S. A case report of papillary mucinous tumor in bile duct[J/CD]. Chin J Hepat Surg: Electronic Edition, 2020, 9(6): 609-612. DOI: 10.3877/cma.j.issn.2095-3232.2020.06.023.李冉冉, 陈永艺, 周松. 胆管内乳头状黏液性肿瘤一例[J/CD]. 中华肝脏外科手术学电子杂志, 2020, 9(6): 609-612. DOI: 10.3877/cma.j.issn.2095-3232.2020.06.023. [17] RUIZ A, VEDEL B, FABRE C, et al. Intraductal papillary mucinous neoplasm of the bile ducts (IPMN-B)[J]. Clin Res Hepatol Gastroenterol, 2016, 40(4): 370-372. DOI: 10.1016/j.clinre.2016.03.001. [18] WANG M, DENG BY, WEN TF, et al. An observational and comparative study on intraductal papillary mucinous neoplasm of the biliary tract and the pancreas from a Chinese cohort[J]. Clin Res Hepatol Gastroenterol, 2016, 40(2): 161-168. DOI: 10.1016/j.clinre.2015.12.002. [19] LI LT, WU B, WANG SQ, et al. Intrahepatic biliary papillomatosis with local canceration: A case report[J]. J Clin Hepatol, 2018, 34(8): 1760-1762. DOI: 10.3969/j.issn.1001-5256.2018.08.035.李良涛, 武波, 王守乾, 等. 肝内胆管乳头状瘤伴局部癌变1例报告[J]. 临床肝胆病杂志, 2018, 34(8): 1760-1762. DOI: 10.3969/j.issn.1001-5256.2018.08.035. [20] ZHANG H, ZHONG Z, KONG G, et al. Clinicopathological findings and imaging features of intraductal papillary neoplasms in bile ducts[J]. PeerJ, 2020, 8: e10040. DOI: 10.7717/peerj.10040. [21] OHTSUKA M, SHIMIZU H, KATO A, et al. Intraductal papillary neoplasms of the bile duct[J]. Int J Hepatol, 2014, 2014: 459091. DOI: 10.1155/2014/459091. [22] YING S, YING M, LIANG W, et al. Morphological classification of intraductal papillary neoplasm of the bile duct[J]. Eur Radiol, 2018, 28(4): 1568-1578. DOI: 10.1007/s00330-017-5123-2. [23] LIU LN, XU HX, ZHANG YF, et al. Imaging features of intraductal papillary neoplasm of the bile duct (IPN-B) on baseline ultrasound and contrast-enhanced ultrasound[J]. Chin J Ultrasonogr, 2012, 21(11): 969-972. DOI: 10.3760/cma.j.issn.1004-4477.2012.11.016.刘琳娜, 徐辉雄, 张一峰, 等. 胆管内乳头状肿瘤超声及超声造影表现[J]. 中华超声影像学杂志, 2012, 21(11): 969-972. DOI: 10.3760/cma.j.issn.1004-4477.2012.11.016. [24] LIU YB, LI M, ZHONG XM, et al. Imaging features of intraductal papillary neoplasm of the bile duct[J]. Chin J Radiol, 2014, 48(2): 128-131. DOI: 10.3760/cma.j.issn.1005-1201.2014.02.010.刘于宝, 李萌, 钟小梅, 等. 胆管导管内乳头状肿瘤的影像表现[J]. 中华放射学杂志, 2014, 48(2): 128-131. DOI: 10.3760/cma.j.issn.1005-1201.2014.02.010. [25] YING SH, ZHAO YL, TENG XD, et al. Imaging findings and morphology classification of intreductal papillary mucinous neoplasm of the bile duct[J]. Chin J Radiol, 2015, 49(1): 42-46. DOI: 10.3760/cma.j.issn.1005-1201.2015.01.011.应世红, 赵艺蕾, 滕晓东, 等. 胆管导管内乳头状黏液性肿瘤的影像表现和形态分型[J]. 中华放射学杂志, 2015, 49(1): 42-46. DOI: 10.3760/cma.j.issn.1005-1201.2015.01.011. [26] YOON HJ, KIM YK, JANG KT, et al. Intraductal papillary neoplasm of the bile ducts: Description of MRI and added value of diffusion-weighted MRI[J]. Abdom Imaging, 2013, 38(5): 1082-1090. DOI: 10.1007/s00261-013-9989-4. [27] YING SH, TENG XD, WANG ZM, et al. Gd-EOB-DTPA-enhanced magnetic resonance imaging for bile duct intraductal papillary mucinous neoplasms[J]. World J Gastroenterol, 2015, 21(25): 7824-7833. DOI: 10.3748/wjg.v21.i25.7824. [28] REN X, ZHU CL, QIN XF, et al. Co-occurrence of IPMN and malignant IPNB complicated by a pancreatobiliary fistula: A case report and review of the literature[J]. World J Clin Cases, 2019, 7(1): 102-108. DOI: 10.12998/wjcc.v7.i1.102. [29] PAN P, ZHAO SB, WANG S, et al. Biliary dilatation in a 67-year-old woman: Seeing is believing[J]. Gut, 2020, 69(2): 223-310. DOI: 10.1136/gutjnl-2018-318200. [30] KUBOTA K, NAKANUMA Y, KONDO F, et al. Clinicopathological features and prognosis of mucin-producing bile duct tumor and mucinous cystic tumor of the liver: A multi-institutional study by the Japan Biliary Association[J]. J Hepatobiliary Pancreat Sci, 2014, 21(3): 176-185. DOI: 10.1002/jhbp.23. [31] WU X, LI BL, ZHENG CJ, et al. Diagnosis and surgical treatment of intraductal papillary mucinous of biliary tract[J]. Chin J Hepatobiliary Surg, 2017, 23(1): 28-31. DOI: 10.3760/cma.j.issn.1007-8118.2017.01.009.吴昕, 李秉璐, 郑朝纪, 等. 胆管导管内乳头状黏液瘤的诊断和外科治疗[J]. 中华肝胆外科杂志, 2017, 23(1): 28-31. DOI: 10.3760/cma.j.issn.1007-8118.2017.01.009. [32] RIZZO A, FREGA G, RICCI AD, et al. Anti-EGFR monoclonal antibodies in advanced biliary tract cancer: A systematic review and meta-analysis[J]. In Vivo, 2020, 34(2): 479-488. DOI: 10.21873/invivo.11798. [33] LEVY MJ, WONG KEE SONG LM, KENDRICK ML, et al. EUS-guided coil embolization for refractory ectopic variceal bleeding (with videos)[J]. Gastrointest Endosc, 2008, 67(3): 572-574. DOI: 10.1016/j.gie.2007.06.063. [34] GUO W, ZHANG ZT. Diagnosis and treatment of intraductal papillary neoplasm of the bile duct[J]. Chin J Dig Surg, 2018, 17(3): 233-236. DOI: 10.3760/cma.j.issn.1673-9752.2018.03.005.郭伟, 张忠涛. 胆管内乳头状肿瘤的诊断与治疗[J]. 中华消化外科杂志, 2018, 17(3): 233-236. DOI: 10.3760/cma.j.issn.1673-9752.2018.03.005. -



 PDF下载 ( 2212 KB)
PDF下载 ( 2212 KB)

 下载:
下载: