慢加急性肝衰竭急性静脉曲张出血的危险因素及预后分析
DOI: 10.3969/j.issn.1001-5256.2022.11.018
Risk factors for acute variceal bleeding in acute-on-chronic liver failure and its influence on prognosis
-
摘要:
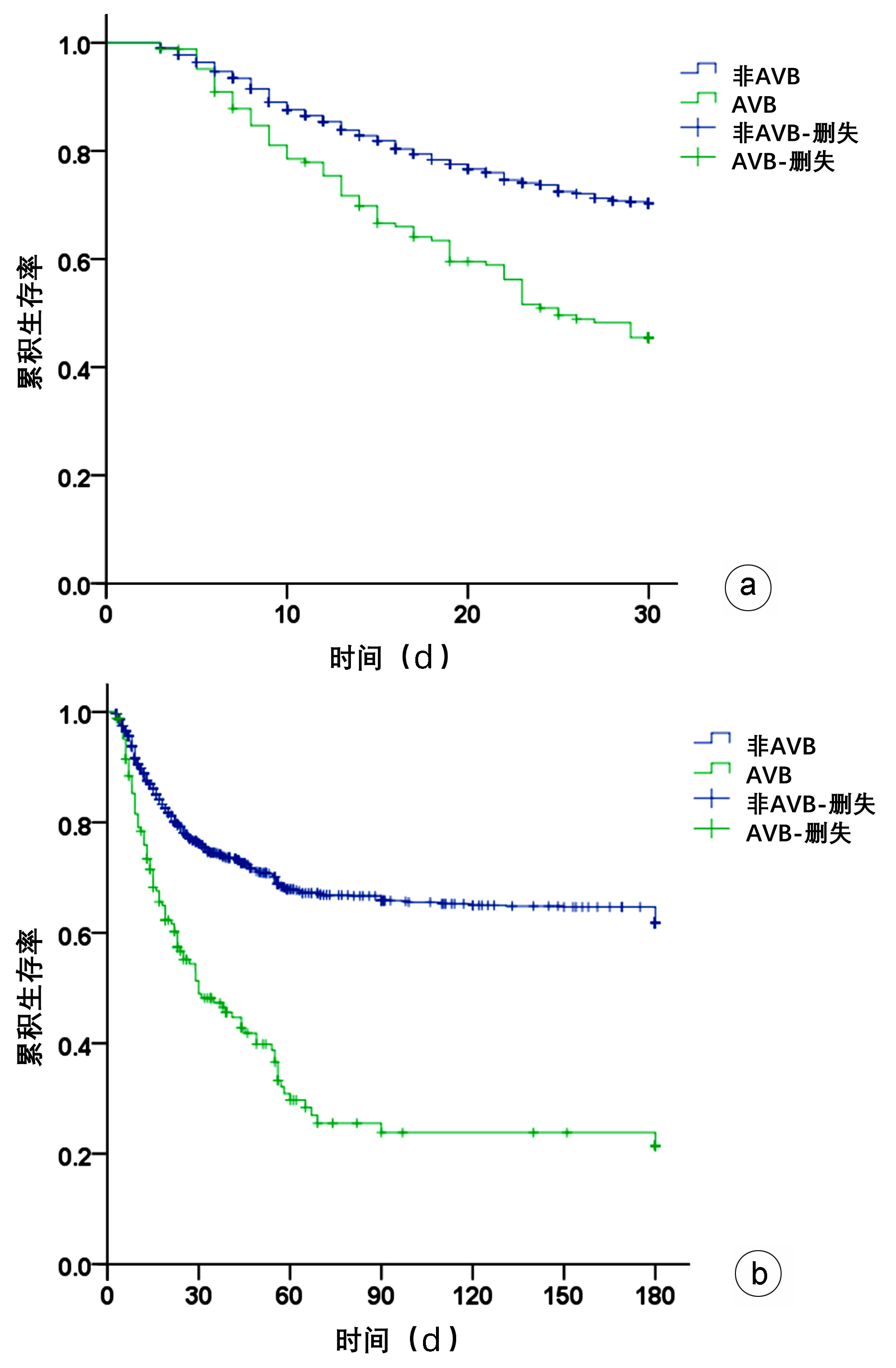
目的 探讨慢加急性肝衰竭(ACLF)急性静脉曲张出血(AVB)的危险因素及对预后的影响。 方法 对解放军总医院第五医学中心2009年—2015年收治ACLF患者1409例随访6个月,根据是否出现AVB分为AVB组(n=167)和非AVB组(n=1242)。计量资料符合正态分布两组间比较使用Student t检验;不符合正态分布资料两组间比较采用Mann-Whitney U检验。Kaplan-Meier法绘制生存曲线,对随访过程中组间病死率及进展进行Log-rank检验。采用二元Logistic回归分析AVB发生的危险因素。 结果 1409例患者发生AVB 167例,占11.85%。AVB及非AVB患者30 d存活率分别为43.42%、67.79%(χ2=33.558,P<0.001);两组患者180 d存活率分别为18.91%、53.97%(χ2=76.881,P<0.001)。Log-rank检验显示AVB与非AVB患者30 d生存率、180 d生存率差异均有统计学意义(χ2值分别为40.950、89.320,P值均<0.05)。Logistic回归分析AVB发生的危险因素,胸腔积液(OR=1.522,95%CI: 1.071 ~2.162,P=0.019)、急性肾损伤(OR=2.201,95%CI: 1.415~3.426,P<0.001)、ACLF分型(OR=2.491,95%CI: 1.489~4.168,P=0.001)、ACLF分期(OR=2.403,95%CI: 1.687~3.421,P<0.001)及尿素(OR=2.567,95%CI:1.570~4.196,P<0.001)与ACLF患者AVB的发生独立相关。 结论 AVB是影响ACLF近期生存的重要因素,胸腔积液、急性肾损伤、ACLF分型BC型、ACLF晚期以及尿素是AVB发生的独立危险因素。 Abstract:Objective To investigate the risk factors for acute variceal bleeding (AVB) in acute-on-chronic liver failure (ACLF) and its influence on prognosis. Methods A total of 1409 ACLF patients who were admitted to The Fifth Medical Center of Chinese PLA General Hospital from 2009 to 2015 were followed up for 6 months, and according to the presence or absence of AVB, they were divided into AVB group and non-AVB group. The Student's t-test was used for comparison of normally distributed continuous data between two groups, and the Mann-Whitney U test was used for comparison of non-normally distributed continuous data between two groups. The Kaplan-Meier curves were plotted and the Log-rank test was performed to analyze mortality rate and progression during follow-up, and a binary Logistic regression analysis was used to investigate the risk factors for AVB. Results Among these 1409 patients, 167 (11.85%) experienced AVB. The 30-day survival rate was 43.42% in the AVB group and 67.79% in the non-AVB group (χ2=33.558, P < 0.001), and the 180-day survival rate was 18.91% in the AVB group and 53.97% in the non-AVB group (χ2=76.881, P < 0.001). The Log-rank test showed significant differences in 30- and 180-day survival rates between the AVB group and the non-AVB group (χ2=40.950 and 89.320, both P < 0.05). The Logistic regression analysis showed that pleural effusion (odds ratio [OR]=1.522, 95% confidence interval [CI]: 1.071-2.162, P=0.019), acute kidney injury (AKI) (OR=2.201, 95%CI: 1.415-3.426, P < 0.001), ABC subtype of ACLF (OR=2.491, 95%CI: 1.489-4.168, P=0.001), ACLF stage (OR=2.403, 95%CI: 1.687-3.421, P < 0.001), and urea(OR=2.567, 95%CI: 1.570-4.196, P < 0.001)were independently associated with AVB in ACLF patients. Conclusion AVB is an important influencing factor for the short-term survival of ACLF patients, and pleural effusion, AKI, BC subtype of ACLF, advanced ACLF, and urea are independent risk factors for the onset of AVB. -
Key words:
- Acute-On-Chronic Liver Failure /
- Varicose Veins /
- Risk Factors /
- Prognosis
-
非酒精性脂肪性肝病(NAFLD)是以体内甘油三酯异常蓄积于肝脏为特征,在远期可进展为肝硬化甚至肝细胞癌,在过去20年间我国NAFLD患病率迅速增长[1],现已取代病毒性肝炎成为我国第一大慢性肝病[2]。现行指南推荐通过改善生活方式来达到预防疾病的目的,但并无可量化的标准以作为参考。理想心血管健康行为和因素包括四个生活方式因素(不吸烟、BMI<25 kg/m2、积极体育活动和符合指南的最佳饮食),以及三个生物因素(未治疗的总胆固醇<200 mg/dL,未治疗的空腹血糖<100 mg/dL,未治疗血压<120/80 mmHg)[3],有多项研究[4-6]已证实促进理想心血管健康行为和因素可有助于降低癌症、糖尿病及慢性肾病等疾病的发病风险。以往研究[7]也通过横断面研究的方法证实健康生活方式与NAFLD呈负向关联。依托开滦研究的数据资料,通过队列研究的方法,探究理想心血管健康行为和因素对NAFLD发病的影响。
1. 资料与方法
1.1 观察对象
本研究数据源于开滦研究(注册号:ChiCTR-TNRC-11001489)。2006年7月—2007年6月(以下简称2006年度),由开滦总医院及所属10家分院对开滦集团职工进行了第1次健康体检,以后每2年进行1次随访,现已完成5次。收集流行病学调查内容、人体测量学指标、生化指标检测以及包括肝脏超声资料在内的腹部超声检查。选择2006年度体检数据作为基线资料。在随后的随访中流行病学调查内容、人体测量学指标及生化指标检测均同第1次健康体检。参加并完成2006年度开滦集团健康体检的在职及离退休职工共计101 510例。入选标准:(1)年满18周岁,参加2006年度健康体检者;(2)基线资料中心血管健康行为和因素7项数据全部完整者;(3)基线肝脏超声资料完整者;(4)至少完成1次随访者。排除标准:(1)长期大量饮酒者(折合乙醇量男性≥140 g/周,女性≥70 g/周);(2)基线资料中患有NAFLD、肝炎、肝硬化者;(3)虽然参加该次随访,但肝脏超声资料缺失者;(4)既往患有恶性肿瘤、心脑血管疾病者。
1.2 资料收集
流行病学调查、人体测量学及血清生化检测等资料的收集方法见本课题组已发表的文章[8]。流行病学收集的数据资料包括体育锻炼、吸烟、饮酒情况等,人体测量学收集资料包括身高、体质量等,血清生化检测收集资料包括血脂、血糖、转氨酶等。
1.3 NAFLD的确定
参照《非酒精性脂肪性肝病防治指南(2018年更新版)》[9]定义。由具有多年临床经验的影像科医生为体检者进行空腹腹部超声检查。采用PHILIPS公司HD-15彩色超声诊断仪,低频探头,频率3.5 MHz。收集资料起自2006年7月1日,截止至2013年12月31日,未发生事件者随访截止时间为死亡时间或末次随访时间,发生事件者随访截止时间为NAFLD确诊时间。
1.4 理想心血管健康行为及因素的定义
根据美国心脏协会2010年提出的心血管健康指标评分标准,包括吸烟、体育锻炼、BMI、饮食、血脂、血压、血糖,每项指标分为3个等级(理想、一般、差)。由于2006年启动的开滦研究调查问卷中未列入“蔬菜摄入量”的健康指标,但考虑到盐摄入水平对我国人群的影响及《心脏病学实践2010——规范化治疗》[10]中提出的健康标准,本研究将美国心脏协会健康行为定义中的“蔬菜摄入量”改为“食盐摄入量”,根据喜好归类为“喜淡”“一般”“喜咸”。
1.5 相关定义
根据2006年度开滦职工收入情况,将家庭人均收入定义为:一般收入(<1000元)、高收入(>1000元);受教育程度:高等教育水平(大学及以上学历)、非高等教育水平(高中及以下学历)。
1.6 分组依据
采用Huffman等人创建的简易复合式评分系统——心血管健康评分(CHS)评估个体心血管健康情况[11]。心血管健康指标的赋值:差为0分,一般为1分,理想为2分,分值范围:0~14分。将研究对象按照CHS评分情况进行四分位分组:第一分位组(CHS≤7分,Q1组)、第二分位组(7分<CHS≤9分,Q2组)、第三分位组(9分<CHS≤10分,Q3组)、第四分位组(CHS>10分,Q4组)。
1.7 伦理学审查
本研究遵照赫尔辛基宣言,并通过开滦总医院伦理委员会审批,批号:200605,所有观察对象均签署知情同意书。
1.8 统计学方法
应用SAS 9.4统计软件进行数据分析。正态分布的计量资料以x±s表示,多组间比较采用单因素方差分析;偏态分布的计量资料采用M(P25~P75)表示,多组间比较采用Kruskal-Wallis H检验。计数资料组间比较采用χ2检验。采用人年发病率描述4组间NAFLD的发病情况。采用Cox比例风险模型分析不同CHS水平对新发NAFLD的HR和95%CI。使用限制性立方样条曲线(restricted cubic spline regression,RCS)计算CHS作为连续型变量和NAFLD发病风险的剂量反应关系。并对CHS的每一组分与NAFLD的发病影响重复进行了Cox回归模型分析。P<0.05为差异有统计学意义。
2. 结果
2.1 一般情况
参加2006年度健康体检者101 510例,按照纳入标准共纳入85 025例观察对象,排除基线资料中过量饮酒者15 450例,患有NAFLD、病毒性肝炎、肝硬化者16 904例,排除随访过程中肝脏超声资料缺失者780例,排除既往恶性肿瘤、心脑血管疾病者1380例,最终纳入统计分析的观察对象共计50 511例,平均(49.15±12.53)岁,其中男37 953例,女12 558例。根据CHS将观察对象进行四分位分组,其中Q1组10 057例,Q2组17 732例,Q3组10 321例,Q4组12 401例,4组间观察人群年龄、男性比例、HDL-C、TG、ALT、Hs-CRP水平及家庭收入、受教育程度、理想BMI、理想血压、理想血糖、理想总胆固醇、理想吸烟、理想体育锻炼、理想饮食比例比较差异均有统计学意义(P值均<0.05)(表 1)。
表 1 观察人群不同分组情况的一般情况比较指标 Q1组(n=10 057) Q2组(n=17 732) Q3组(n=10 321) Q4组(n=12 401) 统计值 P值 年龄(岁) 50.38±11.44 50.72±12.28 49.40±12.73 45.70±12.92 F=451.17 <0.001 男性[例(%)] 9336(92.83) 14 723(83.03) 7492(72.59) 6402(51.62) χ2=598.24 <0.001 HDL-C(mmol/L) 1.53±0.39 1.54±0.40 1.54±0.39 1.52±0.36 F=7.77 <0.001 TG (mmol/L) 1.54(1.09~2.33) 1.23(0.90~1.77) 1.10(0.79~1.51) 0.93(0.68~1.27) χ2=52.83 <0.001 UA (mmol/L) 305.12±87.04 284.01±77.00 369.96±74.26 255.54±71.72 F=825.22 <0.001 ALT(U/L) 19.00(13.00~26.00) 18.00(12.00~23.00) 17.00(12.00~23.00) 15.00(11.00~21.00) χ2=883.24 <0.001 Hs-CRP (mg/L) 0.91(0.40~2.14) 0.70(0.29~1.82) 0.60(0.21~1.64) 0.50(0.20~1.40) χ2=908.36 <0.001 高等教育程度[例(%)] 760(7.56) 1202(6.78) 839(8.13) 1791(14.44) χ2=584.02 <0.001 高家庭收入[例(%)] 791(7.87) 1156(6.52) 623(6.04) 994(8.02) χ2=51.74 <0.001 理想BMI[例(%)] 1430(14.22) 5957(33.59) 5915(57.31) 10 337(83.36) χ2=126.43 <0.001 理想血压[例(%)] 523(5.20) 2505(14.13) 2545(24.66) 7278(58.69) χ2=105.98 <0.001 理想血糖[例(%)] 6440(64.04) 15 421(86.97) 9806(95.01) 12 210(98.46) χ2=66.56 <0.001 理想总胆固醇[例(%)] 3503(34.83) 10 357(58.41) 7658(74.20) 10 841(87.42) χ2=737.19 <0.001 理想吸烟[例(%)] 2710(26.95) 10 610(59.84) 8248(79.91) 11 537(93.03) χ2=119.82 <0.001 理想体育锻炼[例(%)] 1004(9.98) 2337(13.18) 1427(13.83) 2306(18.60) χ2=362.34 <0.001 理想饮食[例(%)] 570(5.67) 1280(7.22) 933(9.04) 1909(15.39) χ2=795.99 <0.001 注:Hs-CRP,超敏-C反应蛋白。 2.2 不同CHS水平对NAFLD的发病影响
64 836例观察对象平均随访5.58年,共发生15 265例NAFLD,男性10 969例,女性4296例。在总人群中,4组观察对象的人年发病率分别为77.88/千人年、61.33/千人年、46.37/千人年、33.69/千人年,随着CHS水平的增加,NAFLD的发病情况依次降低。
Cox比例风险模型结果显示:在校正年龄、性别、HDL-C、TG、ALT、Hs-CRP、家庭收入、受教育程度后,CHS每增加1分,NAFLD的发病风险比为0.73(0.72~0.74)。CHS与NAFLD发病风险的剂量-反应关系,RCS结果表明(取25%、50%和75% 3个截点):CHS连续型变量与NAFLD呈非线性关系(P<0.05)。将CHS的不同分组代入模型,校正相同的混杂因素后,以Q1组为对照组,Q2组、Q3组、Q4组发生NAFLD的风险逐渐降低(P for trend<0.05),Q2组发病风险比为0.78(0.74~0.81),Q 3组发病风险比为0.57(0.54~0.59),Q4组发病风险比为0.38(0.36~0.41)。在男女性及年龄的分层分析中,也得到了类似的结果(P for trent<0.05)(表 2)。
表 2 心血管健康评分影响NAFLD发病的Cox风险比例模型项目 例数 发病例数 发病率(/千人年) HR(95%CI) P值 总体 Q1组 10 057 4104 77.88 Q2组 17 732 5956 61.33 0.78(0.74~0.81) <0.001 Q3组 10 321 2737 46.37 0.57(0.54~0.59) <0.001 Q4组 12 401 2468 33.69 0.38(0.36~0.41) <0.001 性别 <0.0011) 男 Q1组 9336 3655 73.94 Q2组 14 723 4492 54.84 0.77(0.73~0.80) <0.001 Q3组 7492 1725 39.79 0.57(0.53~0.60) <0.001 Q4组 6402 1097 28.92 0.52(0.39~0.45) <0.001 女 Q1组 721 449 137.57 Q2组 3009 1464 96.32 0.79(0.71~0.88) <0.001 Q3组 2829 1012 64.65 0.56(0.50~0.63) <0.001 Q4组 5999 1371 38.81 0.37(0.33~0.42) <0.001 年龄 <0.0011) ≤45岁 Q1组 3106 1164 67.79 Q2组 5584 1773 55.02 0.83(0.77~0.90) <0.001 Q3组 3751 890 39.91 0.58(0.53~0.64) <0.001 Q4组 6192 1016 27.14 0.37(0.34~0.41) <0.001 >45岁 Q1组 6951 2940 82.75 Q2组 12 148 4183 64.46 0.76(0.72~0.79) <0.001 Q3组 6570 1847 50.29 0.56(0.53~0.60) <0.001 Q4组 6209 1452 40.54 0.42(0.39~0.45) <0.001 注:模型校正了年龄、性别、HDL-C、TG、ALT、Hs-CRP、家庭收入、受教育程度。1)P for interaction<0.001。 2.3 CHS各组分对NAFLD的发病影响
Cox比例风险模型结果显示:在校正年龄、性别、HDL-C、TG、ALT、Hs-CRP、家庭收入、受教育程度后,理想BMI、理想血压、理想血糖、理想总胆固醇、理想饮食是NAFLD发病的保护因素,理想吸烟、理想体育锻炼对NAFLD的发病无影响(表 3)。
表 3 CHS各组成影响NAFLD发病的Cox风险比例模型组成 HR(95%CI) P值 理想BMI[例(%)] 0.37(0.36~0.39) <0.001 理想血压[例(%)] 0.72(0.69~0.75) <0.001 理想血糖[例(%)] 0.80(0.77~0.84) <0.001 理想总胆固醇[例(%)] 0.86(0.83~0.89) <0.001 理想吸烟[例(%)] 0.98(0.94~1.02) 0.524 理想体育锻炼[例(%)] 1.02(0.98~1.08) 0.595 理想饮食[例(%)] 0.94(0.90~0.99) 0.006 注:模型校正了年龄、性别、HDL-C、TG、ALT、Hs-CRP、家庭收入、受教育程度。 3. 讨论
随着我国经济水平和生活水平的不断提高,我国NAFLD的患病率同西方发达国家一样,也在呈现不断攀升的局面,主要的影响因素为营养过剩、缺乏体育锻炼等不良生活方式。根据我国流行病学调查数据[12]显示,城乡居民中仅有0.7%的个体拥有全部的6种健康生活方式,这也就意味着居民在健康生活方式方面急需改进。
本研究发现CHS评分越高,NAFLD的发病风险越低。在校正混杂因素后,CHS每增加1分,NAFLD的发病风险下降至0.73。RCS结果显示,CHS与NAFLD发病风险之间的剂量-反应关系呈曲线效应,并非简单直线变化。因此将CHS以四分位分组代入Cox比例风险模型中,与Q1组相比,Q2组、Q3组、Q4组NAFLD的发病风险分别下降至0.78倍、0.57倍、0.38倍。这提示CHS对NAFLD的发病风险起到保护作用。由于NAFLD的发病存在性别与年龄差异,且CHS对NAFLD的影响与性别、年龄存在交互作用,因此按性别和年龄分层后重复进行Cox模型分析。在性别分层分析中,发现女性观察对象未来发生NAFLD的风险较男性更低,这种性别间的差异可能与女性观察对象雌激素的保护作用有关。另外,在年龄分层分析中,青年人群中第四分位组的观察对象未来发生NAFLD的风险低于同水平中老年组,虽然NAFLD的发病年龄越发提前,但早期保持健康的生活方式,对于NAFLD的预防将十分有效。
以往研究结论也支持保持健康的生活方式可以降低NAFLD的发生风险。一项来自我国上海地区包括3424例观察的队列研究[13]结果显示:在5年的随访过程中,与0~2项理想心血管健康行为和因素的观察对象相比,拥有6~7项指标的观察对象发生NAFLD的风险降低66%(OR=0.34,95%CI:0.22~0.51)。Liu等[14]的结果也证实CHS评分越高,NAFLD的发生风险越低。另一项来自韩国的队列研究[15]也得到了类似的结论。但与以往研究不同的是,本研究未简单根据理想心血管健康行为和因素的指标个数进行分组,而是将评分更加细化,考虑到了人群“一般”情况的存在;另外,本研究纳入统计分析的样本量更大,有着更充分的随访时长,因此本结果更具有说服力。
本研究对理想心血管健康行为和因素中的每一组分对NAFLD的发病影响也分别进行了分析,发现保持理想的BMI水平发生NAFLD可降低至0.37,而且保持理想的BMI水平较其他组分对NAFLD的影响更大,所起到的保护作用更强。在本研究中,未能发现理想体育锻炼及理想吸烟与NAFLD间的关联,这可能与这些数据的收集是来自观察对象的自我报告有关。体育锻炼一方面可以减轻肝细胞凋亡和增加胰岛素敏感性来改善NAFLD病情严重程度;另一方面可使机体维持着一个较正常的BMI水平,有助于预防NAFLD的发生[16]。在本研究中,还发现理想饮食也可降低NAFLD的发病,虽然采用盐摄入量来代替蔬菜摄入量作为参考指标,但盐摄入量与NAFLD的发病关系密切,Shen等[17]的研究发现与低食盐摄入量(<6 g/d)的人群相比,中食盐摄入量(6~9 g/d)及高食盐摄入量(≥9 g/d)的观察对象NAFLD的发病风险均有增加。
目前的流行病学研究更加强调健康生活方式的综合效应而非某单一因素的影响,通过主动改善生活方式,积极增加健康行为因素的数量并长期坚持,对于减轻NAFLD造成的疾病负担至关重要。
本研究使用了回顾性队列研究方法,样本量大且失访率低,随访时间长,观察对象依从性较好。但本研究亦存在一定的局限:首先,本研究NAFLD的诊断主要以腹部超声为依据,尽管肝组织活检是目前NAFLD诊断的金标准,但由于活检的有创性,不适于体检人群的流行病学调查。腹部超声检查无创,且方便、快捷便于实施,具有较高灵敏度和特异度。其次,本研究吸烟、饮酒、饮食、体育锻炼等行为特征通过调查对象自报获得,可能存在信息偏倚;最后,基线数据仅使用单次收集的资料,这可能会导致结果不稳定。因此,未来进一步的随访及病因学的探索将有助于精准探讨理想心血管健康行为和因素对NAFLD发病的影响。
-
表 1 1409例ACLF基线特征
Table 1. Baseline and clinical characteristics of 1409 cases of ACLF
指标 AVB组(n=167) 非AVB组(n=1242) 统计值 P值 年龄(岁) 46.48±9.37 46.70±9.97 t=0.079 0.778 性别[例(%)] χ2=0.721 0.396 男 145(12.16) 1047(87.84) 女 22(10.14) 195(89.86) ACLF分型[例(%)] χ2=47.069 <0.001 A型 20(4.17) 460(95.83) B型 115(14.71) 667(85.29) C型 32(21.77) 115(78.23) ACLF分期[例(%)] χ2=47.902 <0.001 早期 3(8.82) 31(91.18) 中期 69(7.61) 838(92.39) 晚期 95(20.30) 373(79.70) 并发症[例(%)] 腹水 157(94.01) 1103(88.81) χ2=3.683 0.055 胸腔积液 77(46.11) 373(30.03) χ2=16.769 <0.001 肺部感染 70(41.92) 196(15.78) χ2=63.960 <0.001 SBP 80(47.90) 373(30.03) χ2=20.743 <0.001 菌血症 24(14.37) 123(9.90) χ2=3.145 0.076 肝性脑病 124(74.25) 446(35.91) χ2=88.252 <0.001 AKI 126(75.45) 497(40.02) χ2=73.500 <0.001 白蛋白(g/L) 28.89±5.73 31.20±4.26 t=6.134 0.013 TBil(μmol/L) 280.55(172.50~421.78) 284.25(194.93~388.43) Z=0.260 0.795 PTA(%) 19.01±10.93 25.72±9.77 t=67.070 <0.001 INR 2.07±0.54 2.07±0.61 t=0.011 0.917 血清钠(mmol/L) 132.47±5.87 133.29±5.89 t=2.861 0.091 胆碱酯酶(U/L) 2 583.30±1 420.97 2 770.91±1 404.29 t=2.056 0.040 纤维蛋白原(g/L) 1.68±0.90 1.74±0.96 t=0.568 0.451 血肌酐(μmol/L) 95.00(78.75~120.25) 89.00(78.00~105.00) Z=2.740 0.006 血尿素(mmol/L) 12.65(7.98~21.04) 6.70(4.60~11.30) Z=10.085 <0.001 血清铁(μmol/L) 22.16±8.63 24.61±7.79 t=13.826 <0.001 血红蛋白(g/L) 112.20(85.75~137.25) 121.70(104.00~139.00) Z=3.512 <0.001 血小板计数(×109/L) 80.32±61.09 94.01±55.35 t=8.741 0.003 MELD评分 25.82±6.69 25.40±5.36 t=0.830 0.363 MELD-Na评分 31.93±11.21 29.93±9.82 t=5.875 0.015 30 d存活率(%) 43.42(66/152) 67.79(722/1065) χ2=33.558 <0.001 180 d存活率(%) 18.91(21/111) 53.97(421/780) χ2=76.881 <0.001 表 2 Logistic回归方程中的变量
Table 2. Variables in the equation for the multilevel Logistic regression
变量 回归系数 标准误 Wald值 自由度 P值 OR 95%CI 胸腔积液 0.420 0.179 5.491 1 0.019 1.522 1.071~2.162 ACLF分型B、C型 0.913 0.263 12.089 1 0.001 2.491 1.489~4.168 ACLF分期晚期 0.877 0.180 23.644 1 <0.001 2.403 1.687~3.421 AKI 0.789 0.226 12.235 1 <0.001 2.201 1.415~3.426 尿素 0.943 0.251 14.122 1 <0.001 2.567 1.570~4.196 血小板计数 0.370 0.199 3.447 1 0.063 1.448 0.980~2.141 MELD-Na评分 -0.311 0.184 2.853 1 0.091 0.733 0.511~1.051 -
[1] SARIN SK, CHOUDHURY A, SHARMA MK, et al. Acute-on-chronic liver failure: consensus recommendations of the Asian Pacific association for the study of the liver (APASL): an update[J]. Hepatol Int, 2019, 13(4): 353-390. DOI: 10.1007/s12072-019-09946-3. [2] JOSHI D, O'GRADY J, PATEL A, et al. Cerebral oedema is rare in acute-on-chronic liver failure patients presenting with high-grade hepatic encephalopathy[J]. Liver Int, 2014, 34(3): 362-366. DOI: 10.1111/liv.12257. [3] SHIN J, YU JH, JIN YJ, et al. Acute-on-chronic liver failure as a major predictive factor for mortality in patients with variceal bleeding[J]. Clin Mol Hepatol, 2020, 26(4): 540-553. DOI: 10.3350/cmh.2020.0034. [4] TREBICKA J, GU W, IBÁÑEZ-SAMANIEGO L, et al. Rebleeding and mortality risk are increased by ACLF but reduced by pre-emptive TIPS[J]. J Hepatol, 2020, 73(5): 1082-1091. DOI: 10.1016/j.jhep.2020.04.024. [5] AL-MAHTAB M, AKBAR SM, GARG H. Influence of variceal bleeding on natural history of ACLF and management options[J]. Hepatol Int, 2016, 10(3): 436-439. DOI: 10.1007/s12072-015-9677-2. [6] Liver Failure and Artificial Liver Group, Chinese Society of Infectious Diseases, Chinese Medical Association; Severe Liver Diseases and Artificial Liver Group, Chinese Society of Hepatology, Chinese Medical Association. Diagnostic and treatment guidelines for liver failure (2018 version)[J]. J Chin Hepatol, 2019, 35(1): 38-44. DOI: 10.3969/j.issn.1001-5256.2019.01.007.中华医学会感染病学分会肝衰竭与人工肝学组, 中华医学会肝病学分会重型肝病与人工肝学组. 肝衰竭诊治指南(2018年版)[J]. 临床肝胆病杂志, 2019, 35(1): 38-44. DOI: 10.3969/j.issn.1001-5256.2019.01.007. [7] MOREAU R, JALAN R, GINES P, et al. Acute-on-chronic liver failure is a distinct syndrome that develops in patients with acute decompensation of cirrhosis[J]. Gastroenterology, 2013, 144(7): 1426-1437. e1-9. DOI: 10.1053/j.gastro.2013.02.042. [8] GARCIA-TSAO G, ABRALDES JG, BERZIGOTTI A, et al. Portal hypertensive bleeding in cirrhosis: Risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases[J]. Hepatology, 2017, 65(1): 310-335. DOI: 10.1002/hep.28906. [9] HUANG Y, ZHANG W, XIANG H, et al. Treatment strategies in emergency endoscopy for acute esophageal variceal bleeding (CHESS1905): A Nationwide Cohort Study[J]. Front Med (Lausanne), 2022, 9: 872881. DOI: 10.3389/fmed.2022.872881. [10] KAMATH PS, KIM WR, Advanced Liver Disease Study Group. The model for end-stage liver disease (MELD)[J]. Hepatology, 2007, 45(3): 797-805. DOI: 10.1002/hep.21563. [11] KIM WR, BIGGINS SW, KREMERS WK, et al. Hyponatremia and mortality among patients on the liver-transplant waiting list[J]. N Engl J Med, 2008, 359(10): 1018-1026. DOI: 10.1056/NEJMoa0801209. [12] GARG H, KUMAR A, GARG V, et al. Hepatic and systemic hemodynamic derangements predict early mortality and recovery in patients with acute-on-chronic liver failure[J]. J Gastroenterol Hepatol, 2013, 28(8): 1361-1367. DOI: 10.1111/jgh.12191. [13] KAR R, KAR SS, SARIN SK. Hepatic coagulopathy-intricacies and challenges; a cross-sectional descriptive study of 110 patients from a superspecialty institute in North India with review of literature[J]. Blood Coagul Fibrinolysis, 2013, 24(2): 175-180. DOI: 10.1097/MBC.0b013e32835b2483. [14] European Association for the Study of the Liver. EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis[J]. J Hepatol, 2018, 69(2): 406-460. DOI: 10.1016/j.jhep.2018.03.024. [15] AMITRANO L, GUARDASCIONE MA, MARTINO R, et al. Hypoxic hepatitis occurring in cirrhosis after variceal bleeding: still a lethal disease[J]. J Clin Gastroenterol, 2012, 46(7): 608-612. DOI: 10.1097/MCG.0b013e318254e9d4. [16] KUMAR A, DAS K, SHARMA P, et al. Hemodynamic studies in acute-on-chronic liver failure[J]. Dig Dis Sci, 2009, 54(4): 869-878. DOI: 10.1007/s10620-008-0421-9. [17] MEHTA G, MOOKERJEE RP, SHARMA V, et al. Systemic inflammation is associated with increased intrahepatic resistance and mortality in alcohol-related acute-on-chronic liver failure[J]. Liver Int, 2015, 35(3): 724-734. DOI: 10.1111/liv.12559. [18] TREBICKA J, GU W, IBÁÑEZ-SAMANIEGO L, et al. Rebleeding and mortality risk are increased by ACLF but reduced by pre-emptive TIPS[J]. J Hepatol, 2020, 73(5): 1082-1091. DOI: 10.1016/j.jhep.2020.04.024. [19] HEO NY. Acute-on-chronic liver failure: A predictor of poor prognosis in patients with variceal bleeding or a risk factor for variceal bleeding?[J]. Clin Mol Hepatol, 2020, 26(4): 487-488. DOI: 10.3350/cmh.2020.0209. [20] KUMAR R, KERBERT A, SHEIKH MF, et al. Determinants of mortality in patients with cirrhosis and uncontrolled variceal bleeding[J]. J Hepatol, 2021, 74(1): 66-79. DOI: 10.1016/j.jhep.2020.06.010. 期刊类型引用(6)
1. 王钰莹,张继佳,吴照科,朱慎慎. 老年冠心病患者营养不良的影响因素及Nomogram预测模型的构建. 海南医学. 2025(01): 34-40 .  百度学术
百度学术2. 刘文丽,丁彦淳,蔡靖姣. 心血管健康行为和健康因素对2型糖尿病人群脑梗死事件的影响研究. 当代护士(下旬刊). 2024(12): 111-115 .  百度学术
百度学术3. 曾冠男,陈容容,卢世云. 成年人Life's Simple 7和非酒精性脂肪性肝病之间的关联. 中国医药指南. 2023(21): 29-32 .  百度学术
百度学术4. 李庚,张国新,凡华,李恒涛,汤卫兵. 短期强化他汀治疗ST段抬高型心肌梗死的效果. 长春中医药大学学报. 2023(10): 1138-1141 .  百度学术
百度学术5. 迟玉玉,刘丹,刘涛,郁建阳,周晓燕,吴寿岭. 理想心血管健康指标评分对恶性肿瘤发病的影响. 中西医结合心脑血管病杂志. 2023(22): 4210-4214 .  百度学术
百度学术6. 徐淑倩,朱敬丽,刘梦莹,沈冲,于蕾,陆慧. 成人心血管健康评分、生命质量与心脑血管病的关系研究. 中国心血管病研究. 2023(11): 966-971 .  百度学术
百度学术其他类型引用(0)
-




 PDF下载 ( 2154 KB)
PDF下载 ( 2154 KB)

 下载:
下载:
 下载:
下载:
 百度学术
百度学术

