| [1] |
Chinese Society of Hepatology, Chinese Medical Association. Chinese guidelines on the management of liver cirrhosis[J]. J Clin Hepatol, 2019, 35( 11): 2408- 2425. DOI: 10.3969/j.issn.1001-5256.2019.11.006. |
| [2] |
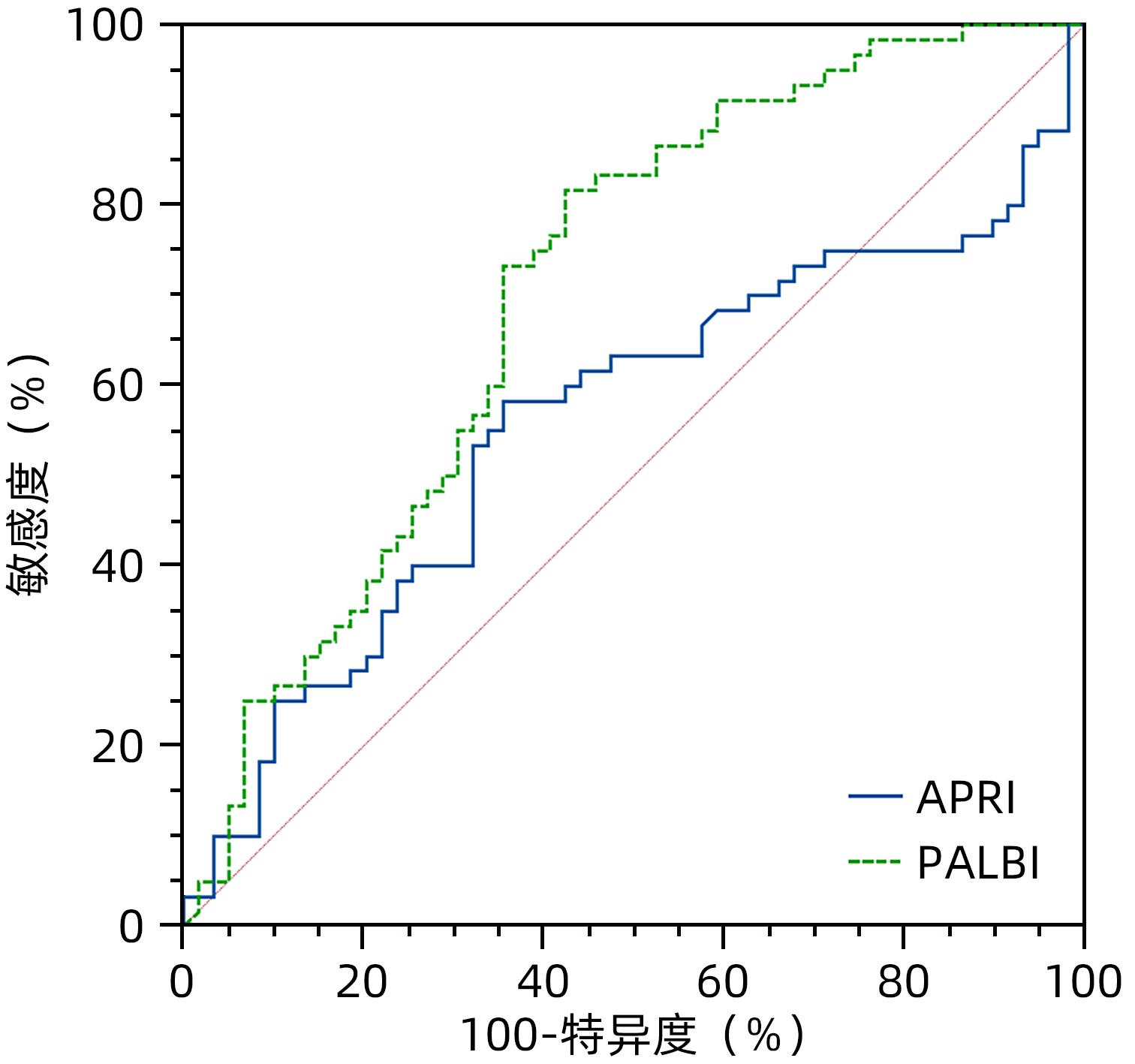
DENG H, QI X, PENG Y, et al. Diagnostic accuracy of APRI, AAR, FIB-4, FI, and King Scores for diagnosis of esophageal varices in liver cirrhosis: A retrospective study[J]. Med Sci Monit, 2015, 21: 3961- 3977. DOI: 10.12659/msm.895005. |
| [3] |
WU X, ZHANG XJ, XUE Y, et al. Changes and clinical significance of blood antithrombin- and D-dimer levels in liver cirrhosis patients with gastrointestinal bleeding[J/CD]. Chin J Liver Dis: Electronic Edition, 2023, 15( 1): 56- 61. DOI: 10.3969/j.issn.1674-7380.2023.01.009. |
| [4] |
LI DZ, LI J, GUO XL. Value of albumin-bilirubin score in predicting the prognosis of patients with liver cirrhosis and esophagogastric variceal bleeding[J]. J Clin Hepatol, 2021, 37( 5): 1085- 1090. DOI: 10.3969/j.issn.1001-5256.2021.05.022. |
| [5] |
TANAKA K, TSUJI K, MATSUI T, et al. Potential of PALBI-T score as a prognostic model for hepatocellular carcinoma in alcoholic liver disease[J]. JGH Open, 2022, 6( 1): 36- 43. DOI: 10.1002/jgh3.12705. |
| [6] |
|
| [7] |
NIU SN, ZHAO JY, CHANG YF, et al. Application of monitored anesthesia care technique in emergency endoscopic treatment of liver cirrhosis patients with gastric varices bleeding[J/CD]. Chin J Liver Dis(Electronic Version), 2022, 14( 1): 67- 72. DOI: 10.3969/j.issn.1674-7380.2022.01.010. |
| [8] |
SINGAL AK, MATHURIN P. Diagnosis and treatment of alcohol-associated liver disease: A review[J]. JAMA, 2021, 326( 2): 165- 176. DOI: 10.1001/jama.2021.7683. |
| [9] |
ZHANG XH, GUAN L, TIAN HY, et al. Risk factors and prevention of viral hepatitis-related hepatocellular carcinoma[J]. Front Oncol, 2021, 11: 686962. DOI: 10.3389/fonc.2021.686962. |
| [10] |
MAI RY, WANG YY, BAI T, et al. Combination of ALBI and APRI to predict post-hepatectomy liver failure after liver resection for HBV-related HCC patients[J]. Cancer Manag Res, 2019, 11: 8799- 8806. DOI: 10.2147/CMAR.S213432. |
| [11] |
WAI CT, GREENSON JK, FONTANA RJ, et al. A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis C[J]. Hepatology, 2003, 38( 2): 518- 526. DOI: 10.1053/jhep.2003.50346. |
| [12] |
XIAO GQ, YANG JY, YAN LN. Comparison of diagnostic accuracy of aspartate aminotransferase to platelet ratio index and fibrosis-4 index for detecting liver fibrosis in adult patients with chronic hepatitis B virus infection: A systemic review and meta-analysis[J]. Hepatology, 2015, 61( 1): 292- 302. DOI: 10.1002/hep.27382. |
| [13] |
SHRIVASTAVA R, SEN S, BANERJI D, et al. Assessment of non-invasive models for liver fibrosis in chronic hepatitis B virus related liver disease patients in resource limited settings[J]. Indian J Pathol Microbiol, 2013, 56( 3): 196- 199. DOI: 10.4103/0377-4929.120359. |
| [14] |
IACOB DG, LUMINOS M, BENEA OE, et al. Liver fibrosis progression in a cohort of young HIV and HIV/HBV co-infected patients: A longitudinal study using non-invasive APRI and Fib-4 scores[J]. Front Med, 2022, 9: 888050. DOI: 10.3389/fmed.2022.888050. |
| [15] |
KANG NL, RUAN QF, ZHANG DS, et al. Advantages of a novel model for predicting hepatic fibrosis in chronic hepatitis B virus carriers compared with APRI and FIB-4 scores[J]. J Clin Transl Hepatol, 2022, 10( 3): 412- 419. DOI: 10.14218/JCTH.2022.00098. |
| [16] |
MORISHITA N, HIRAMATSU N, OZE T, et al. Liver stiffness measurement by acoustic radiation force impulse is useful in predicting the presence of esophageal varices or high-risk esophageal varices among patients with HCV-related cirrhosis[J]. J Gastroenterol, 2014, 49( 7): 1175- 1182. DOI: 10.1007/s00535-013-0877-z. |
| [17] |
WANG JH, CHUAH SK, LU SN, et al. Transient elastography and simple blood markers in the diagnosis of esophageal varices for compensated patients with hepatitis B virus-related cirrhosis[J]. J Gastroenterol Hepatol, 2012, 27( 7): 1213- 1218. DOI: 10.1111/j.1440-1746.2012.07132.x. |
| [18] |
YANG L, KAN QX, GAO J. Relationship between PALBI, MELD, INR and the prognosis of patients with liver cirrhosis combined with upper gastrointestinal hemorrhage and a multivariate study[J]. J Clin Exp Med, 2022, 21( 11): 1137- 1141. DOI: 10.3969/j.issn.1671-4695.2022.11.005. |






 DownLoad:
DownLoad:



