| [1] |
RIAZI K, AZHARI H, CHARETTE JH, et al. The prevalence and incidence of NAFLD worldwide: a systematic review and meta-analysis[J]. Lancet Gastroenterol Hepatol, 2022, 7( 9): 851- 861. DOI: 10.1016/S2468-1253(22)00165-0. |
| [2] |
WU CM, ZHANG CY, XU HL, et al. Epidemiological research and diagnosis of nonalcoholic fatty liver disease in China[J]. China Med Herald, 2023, 20( 11): 158- 161. DOI: 10.20047/j.issn1673-7210.2023.11.36. |
| [3] |
JIN R, WANG XX, LIU F, et al. Research advances in pharmacotherapy for nonalcoholic fatty liver disease[J]. J Clin Hepatol, 2022, 38( 7): 1634- 1640. DOI: 10.3969/j.issn.1001-5256.2022.07.033. |
| [4] |
ZHAO Q, YU J, HAO Y, et al. Akkermansiamuciniphila plays critical roles in host health[J]. Crit Rev Microbiol, 2023, 49( 1): 82- 100. DOI: 10.1080/1040841X.2022.2037506. |
| [5] |
SHEN K, SINGH AD, MODARESI ESFEH J, et al. Therapies for non-alcoholic fatty liver disease: A 2022 update[J]. World J Hepatol, 2022, 14( 9): 1718- 1729. DOI: 10.4254/wjh.v14.i9.1718. |
| [6] |
LI YQ, TANG WJ, ZHOU YJ. Role of intestinal microbiota and metabolites in the development, progression, and treatment of nonalcoholic fatty liver disease[J]. J Clin Hepatol, 2023, 39( 8): 1805- 1810. DOI: 10.3969/j.issn.1001-5256.2023.08.006. |
| [7] |
|
| [8] |
CANI PD, DEPOMMIER C, DERRIEN M, et al. Akkermansia muciniphila: paradigm for next-generation beneficial microorganisms[J]. Nat Rev Gastroenterol Hepatol, 2022, 19( 10): 625- 637. DOI: 10.1038/s41575-022-00631-9. |
| [9] |
SI J, KANG H, YOU HJ, et al. Revisiting the role of Akkermansia muciniphila as a therapeutic bacterium[J]. Gut Microbes, 2022, 14( 1): 2078619. DOI: 10.1080/19490976.2022.2078619. |
| [10] |
BAE M, CASSILLY CD, LIU X, et al. Akkermansia muciniphilaphospholipid induces homeostatic immune responses[J]. Nature, 2022, 608( 7921): 168- 173. DOI: 10.1038/s41586-022-04985-7. |
| [11] |
KESHAVARZ AZIZI RAFTAR S, ASHRAFIAN F, YADEGAR A, et al. The protective effects of live and pasteurized akkermansiamuciniphila and its extracellular vesicles against HFD/CCl4-induced liver injury[J]. Microbiol Spectr, 2021, 9( 2): e0048421. DOI: 10.1128/Spectrum.00484-21. |
| [12] |
KIM S, SHIN YC, KIM TY, et al. Mucin degrader Akkermansiamuciniphila accelerates intestinal stem cell-mediated epithelial development[J]. Gut Microbes, 2021, 13( 1): 1- 20. DOI: 10.1080/19490976.2021.1892441. |
| [13] |
QU S, FAN L, QI Y, et al. Akkermansiamuciniphila Alleviates Dextran Sulfate Sodium(DSS)-induced acute colitis by NLRP3 activation[J]. Microbiol Spectr, 2021, 9( 2): e0073021. DOI: 10.1128/Spectrum.00730-21. |
| [14] |
REUNANEN J, KAINULAINEN V, HUUSKONEN L, et al. Akkermansia muciniphila adheres to enterocytes and strengthens the integrity of the epithelial cell layer[J]. Appl Environ Microbiol, 2015, 81( 11): 3655- 3662. DOI: 10.1128/AEM.04050-14. |
| [15] |
LOPETUSO LR, QUAGLIARIELLO A, SCHIAVONI M, et al. Towards a disease-associated common trait of gut microbiota dysbiosis: The pivotal role of Akkermansia muciniphila[J]. Dig Liver Dis, 2020, 52( 9): 1002- 1010. DOI: 10.1016/j.dld.2020.05.020. |
| [16] |
SUN XW, HE JH, JIANG XZ, et al. Probiotics A. muciniphila improving diarrhea induced by ETEC in mice[J]. Acta Univ Med Nanjing(Natural Science Edition), 2023, 43( 1): 27- 33. DOI: 10.7655/NYDXBNS20230104. 孙学伟, 何君花, 姜新泽, 等. 益生菌 A. muciniphila改善大肠杆菌诱导的小鼠腹泻[J]. 南京医科大学学报(自然科学版), 2023, 43( 1): 27- 33. DOI: 10.7655/NYDXBNS20230104. |
| [17] |
ŠEŠELJA K, BAZINA I, VRECL M, et al. TFF3 deficiency protects against hepatic fat accumulation after prolonged high-fat diet[J]. Life(Basel), 2022, 12( 8): 1288. DOI: 10.3390/life12081288. |
| [18] |
BARCENA C, VALDES-MAS R, MAYORAL P, et al. Healthspan and lifespan extension by fecal microbiota transplantation into progeroid mice[J]. Nat Med, 2019, 25( 8): 1234- 1242. DOI: 10.1038/s41591-019-0504-5. |
| [19] |
van der LUGT B, van BEEK AA, AALVINK S, et al. Akkermansia muciniphila ameliorates the age-related decline in colonic mucus thickness and attenuates immune activation in accelerated aging Ercc1-/Δ7 mice[J]. Immun Ageing, 2019, 16: 6. DOI: 10.1186/s12979-019-0145-z. |
| [20] |
GRANDER C, GRABHERR F, SPADONI I, et al. The role of gut vascular barrier in experimental alcoholic liver disease and A. muciniphila supplementation[J]. Gut Microbes, 2020, 12( 1): 1851986. DOI: 10.1080/19490976.2020.1851986. |
| [21] |
BI M, LIU C, WANG Y, et al. Therapeutic prospect of new probiotics in neurodegenerative diseases[J]. Microorganisms, 2023, 11( 6): 1527. DOI: 10.3390/microorganisms11061527. |
| [22] |
OU Z, DENG L, LU Z, et al. Protective effects of Akkermansiamuciniphila on cognitive deficits and amyloid pathology in a mouse model of Alzheimer’s disease[J]. Nutr Diabetes, 2020, 10( 1): 12. DOI: 10.1016/j.jep.2023.116505. |
| [23] |
LIU J, LIU H, LIU H, et al. Live and pasteurized Akkermansia muciniphila decrease susceptibility to Salmonella Typhimurium infection in mice[J]. J Adv Res, 2023, 52: 89- 102. DOI: 10.1016/j.jare.2023.03.008. |
| [24] |
LI J, YANG G, ZHANG Q, et al. Function of Akkermansia muciniphila in type 2 diabetes and related diseases[J]. Front Microbiol, 2023, 14: 1172400. DOI: 10.3389/fmicb.2023.1172400. |
| [25] |
HOYLES L, FERNÁNDEZ-REAL JM, FEDERICI M, et al. Molecular phenomics and metagenomics of hepatic steatosis in non-diabetic obese women[J]. Nat Med, 2018, 24( 7): 1070- 1080. DOI: 10.1038/s41591-018-0061-3. |
| [26] |
TSAI HJ, TSAI YC, HUNG WW, et al. Gut microbiota and non-alcoholic fatty liver disease severity in type 2 diabetes patients[J]. J Pers Med, 2021, 11( 3). DOI: 10.3390/jpm11030238. |
| [27] |
ÖZKUL C, YALıNAY M, KARAKAN T, et al. Determination of certain bacterial groups in gut microbiota and endotoxin levels in patients with nonalcoholic steatohepatitis[J]. Turk J Gastroenterol, 2017, 28( 5): 361- 369. DOI: 10.5152/tjg.2017.17033. |
| [28] |
LIANG T, LI D, ZUNONG J, et al. Interplay of lymphocytes with the intestinal microbiota in children with nonalcoholic fatty liver disease[J]. Nutrients, 2022, 14( 21): 4641. DOI: 10.3390/nu14214641. |
| [29] |
PAN X, KAMINGA AC, LIU A, et al. Gut microbiota, glucose, lipid, and water-electrolyte metabolism in children with nonalcoholic fatty liver disease[J]. Front Cell Infect Microbiol, 2021, 11: 683743. DOI: 10.3389/fcimb.2021.683743. |
| [30] |
KIM S, LEE Y, KIM Y, et al. Akkermansia muciniphila prevents fatty liver disease, decreases serum triglycerides, and maintains gut homeostasis[J]. Appl Environ Microbiol, 2020, 86( 7): e03004-19. DOI: 10.1128/AEM.03004-19. |
| [31] |
SHI Z, LEI H, CHEN G, et al. Impaired intestinal Akkermansia muciniphila and Aryl hydrocarbon receptor ligands contribute to nonalcoholic fatty liver disease in mice[J]. mSystems, 2021, 6( 1): e00985-20. DOI: 10.1128/mSystems.00985-20. |
| [32] |
YE JZ, LI YT, WU WR, et al. Dynamic alterations in the gut microbiota and metabolome during the development of methionine-choline-deficient diet-induced nonalcoholic steatohepatitis[J]. World J Gastroenterol, 2018, 24( 23): 2468- 2481. DOI: 10.3748/wjg.v24.i23.2468. |
| [33] |
CHOPYK DM, GRAKOUI A. Contribution of the intestinal microbiome and gut barrier to hepatic disorders[J]. Gastroenterology, 2020, 159( 3): 849- 863. DOI: 10.1053/j.gastro.2020.04.077. |
| [34] |
CARPINO G, DEL BEN M, PASTORI D, et al. Increased liver localization of lipopolysaccharides in human and experimental NAFLD[J]. Hepatology, 2020, 72( 2): 470- 485. DOI: 10.1002/hep.31056. |
| [35] |
ZHAO S, LIU W, WANG J, et al. Akkermansia muciniphila improves metabolic profiles by reducing inflammation in chow diet-fed mice[J]. J Mol Endocrinol, 2017, 58( 1): 1- 14. DOI: 10.1530/JME-16-0054. |
| [36] |
WU W, LV L, SHI D, et al. Protective effect of Akkermansia muciniphila against immune-mediated liver injury in a mouse model[J]. Front Microbiol, 2017, 8: 1804. DOI: 10.3389/fmicb.2017.01804. |
| [37] |
CLIFFORD BL, SEDGEMAN LR, WILLIAMS KJ, et al. FXR activation protects against NAFLD via bile-acid-dependent reductions in lipid absorption[J]. Cell Metab, 2021, 33( 8): 1671- 1684. e 4. DOI: 10.1016/j.cmet.2021.06.012. |
| [38] |
YAN N, YAN T, XIA Y, et al. The pathophysiological function of non-gastrointestinal farnesoid X receptor[J]. Pharmacol Ther, 2021, 226: 107867. DOI: 10.1016/j.pharmthera.2021.107867. |
| [39] |
NIAN F, WU L, XIA Q, et al. Akkermansia muciniphila and bifidobacterium bifidum prevent NAFLD by regulating FXR expression and gut microbiota[J]. J Clin Transl Hepatol, 2023, 11( 4): 763- 776. DOI: 10.14218/JCTH.2022.00415. |
| [40] |
LENG W, LIU Y, SHI H, et al. Aspartate alleviates liver injury and regulates mRNA expressions of TLR4 and NOD signaling-related genes in weaned pigs after lipopolysaccharide challenge[J]. J Nutr Biochem, 2014, 25( 6): 592- 599. DOI: 10.1016/j.jnutbio.2014.01.010. |
| [41] |
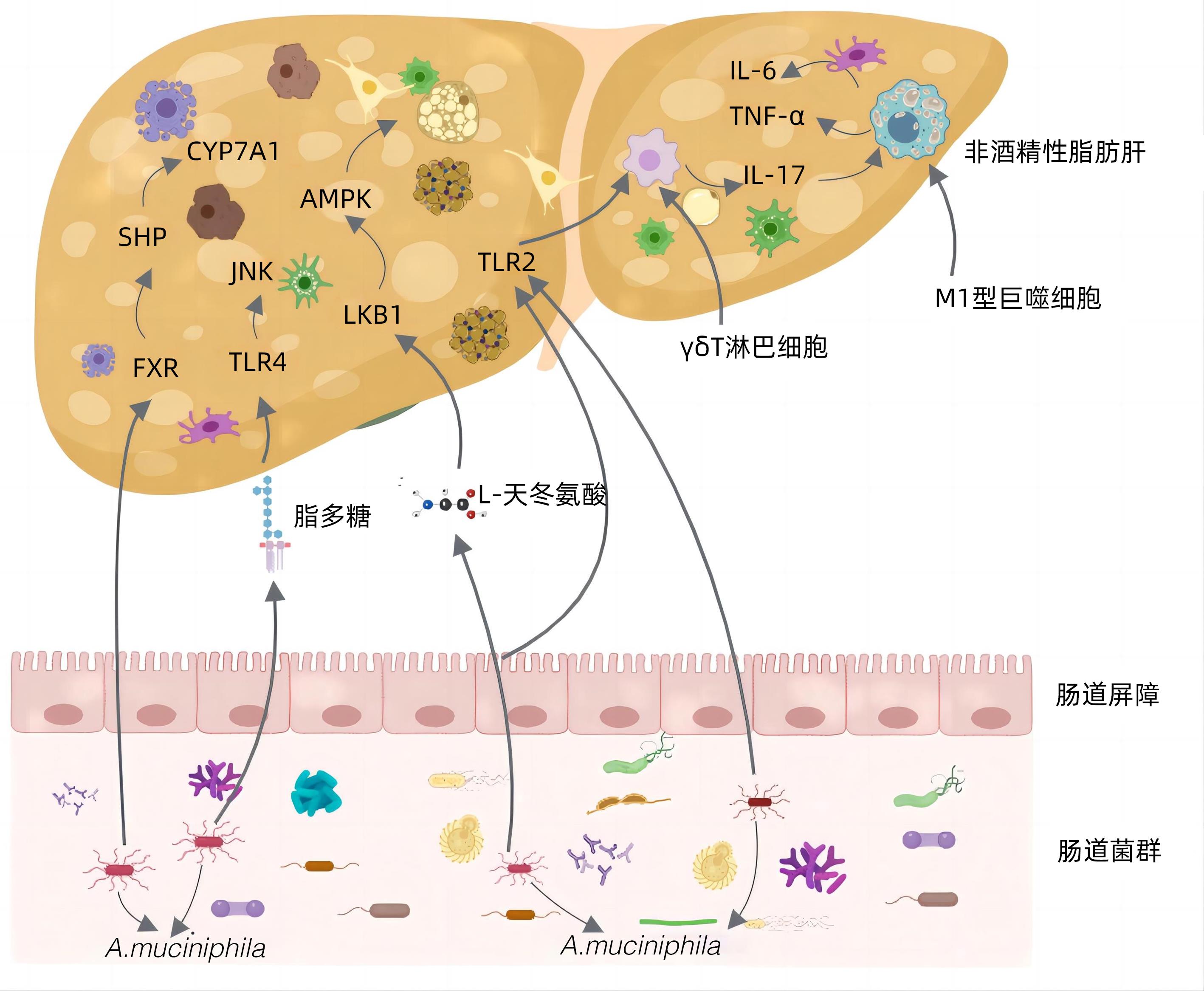
RAO Y, KUANG Z, LI C, et al. Gut Akkermansia muciniphila ameliorates metabolic dysfunction-associated fatty liver disease by regulating the metabolism of L-aspartate via gut-liver axis[J]. Gut Microbes, 2021, 13( 1): 1- 19. DOI: 10.1080/19490976.2021.1927633. |
| [42] |
KAZANKOV K, JØRGENSEN S, THOMSEN KL, et al. The role of macrophages in nonalcoholic fatty liver disease and nonalcoholic steatohepatitis[J]. Nat Rev Gastroenterol Hepatol, 2019, 16( 3): 145- 159. DOI: 10.1038/s41575-018-0082-x. |
| [43] |
HAN Y, LING Q, WU L, et al. Akkermansia muciniphila inhibits nonalcoholic steatohepatitis by orchestrating TLR2-activated γδT17 cell and macrophage polarization[J]. Gut Microbes, 2023, 15( 1): 2221485. DOI: 10.1080/19490976.2023.2221485. |
| [44] |
NEGI CK, BABICA P, BAJARD L, et al. Insights into the molecular targets and emerging pharmacotherapeutic interventions for nonalcoholic fatty liver disease[J]. Metabolism, 2022, 126: 154925. DOI: 10.1016/j.metabol.2021.154925. |
| [45] |
MOREIRA GV, AZEVEDO FF, RIBEIRO LM, et al. Liraglutide modulates gut microbiota and reduces NAFLD in obese mice[J]. J Nutr Biochem, 2018, 62: 143- 154. DOI: 10.1016/j.jnutbio.2018.07.009. |
| [46] |
DU J, ZHANG P, LUO J, et al. Dietary betaine prevents obesity through gut microbiota-drived microRNA-378a family[J]. Gut Microbes, 2021, 13( 1): 1- 19. DOI: 10.1080/19490976.2020.1862612. |
| [47] |
ZHANG Y, YANG L, ZHAO N, et al. Soluble polysaccharide derived from Laminaria japonica attenuates obesity-related nonalcoholic fatty liver disease associated with gut microbiota regulation[J]. Mar Drugs, 2021, 19( 12): 699. DOI: 10.3390/md19120699. |
| [48] |
PÉREZ-MONTER C, ÁLVAREZ-ARCE A, NUÑO-LAMBARRI N, et al. Inulin improves diet-induced hepatic steatosis and increases intestinal akkermansia genus level[J]. Int J Mol Sci, 2022, 23( 2): 991. DOI: 10.3390/ijms23020991. |
| [49] |
ZHANG WJ, LI T. Akkermansia muciniphila suppresses non-alcoholic steatohepatitis-associated liver cancer in mice by recovering intestinal barrier function[J]. Cancer Res Prevent Treat, 2023, 50( 5): 463- 469. DOI: 10.3971/j.issn.1000-8578.2023.22.1259. |
| [50] |
HIGARZA SG, ARBOLEYA S, ARIAS JL, et al. Akkermansia muciniphila and environmental enrichment reverse cognitive impairment associated with high-fat high-cholesterol consumption in rats[J]. Gut Microbes, 2021, 13( 1): 1- 20. DOI: 10.1080/19490976.2021.1880240. |
| [51] |
AGUZZI A, BARRES BA, BENNETT ML. Microglia: scapegoat, saboteur, or something else?[J]. Science, 2013, 339( 6116): 156- 161. DOI: 10.1126/science.1227901. |
| [52] |
YANG Y, ZHONG Z, WANG B, et al. Early-life high-fat diet-induced obesity programs hippocampal development and cognitive functions via regulation of gut commensal Akkermansia muciniphila[J]. Neuropsychopharmacology, 2019, 44( 12): 2054- 2064. DOI: 10.1038/s41386-019-0437-1. |






 DownLoad:
DownLoad: