| [1] |
CHIANG JYL, FERRELL JM. Discovery of farnesoid X receptor and its role in bile acid metabolism[J]. Mol Cell Endocrinol, 2022, 548: 111618. DOI: 10.1016/j.mce.2022.111618. |
| [2] |
FANG D, LI PY. The treatment of cholestasis[J]. J Crit Care Intern Med, 2020, 26( 1): 22- 24. DOI: 10.11768/nkjwzzzz20200106. |
| [3] |
LI X, HAN XX, VOGT RD, et al. Polyethylene terephthalate and di-(2-ethylhexyl) phthalate in surface and core sediments of Bohai Bay, China: Occurrence and ecological risk[J]. Chemosphere, 2022, 286( Pt 3): 131904. DOI: 10.1016/j.chemosphere.2021.131904. |
| [4] |
BAGEL S, DESSAIGNE B, BOURDEAUX D, et al. Influence of lipid type on bis(2-ethylhexyl)phthalate(DEHP) leaching from infusion line sets in parenteral nutrition[J]. JPEN J Parenter Enteral Nutr, 2011, 35( 6): 770- 775. DOI: 10.1177/0148607111414021. |
| [5] |
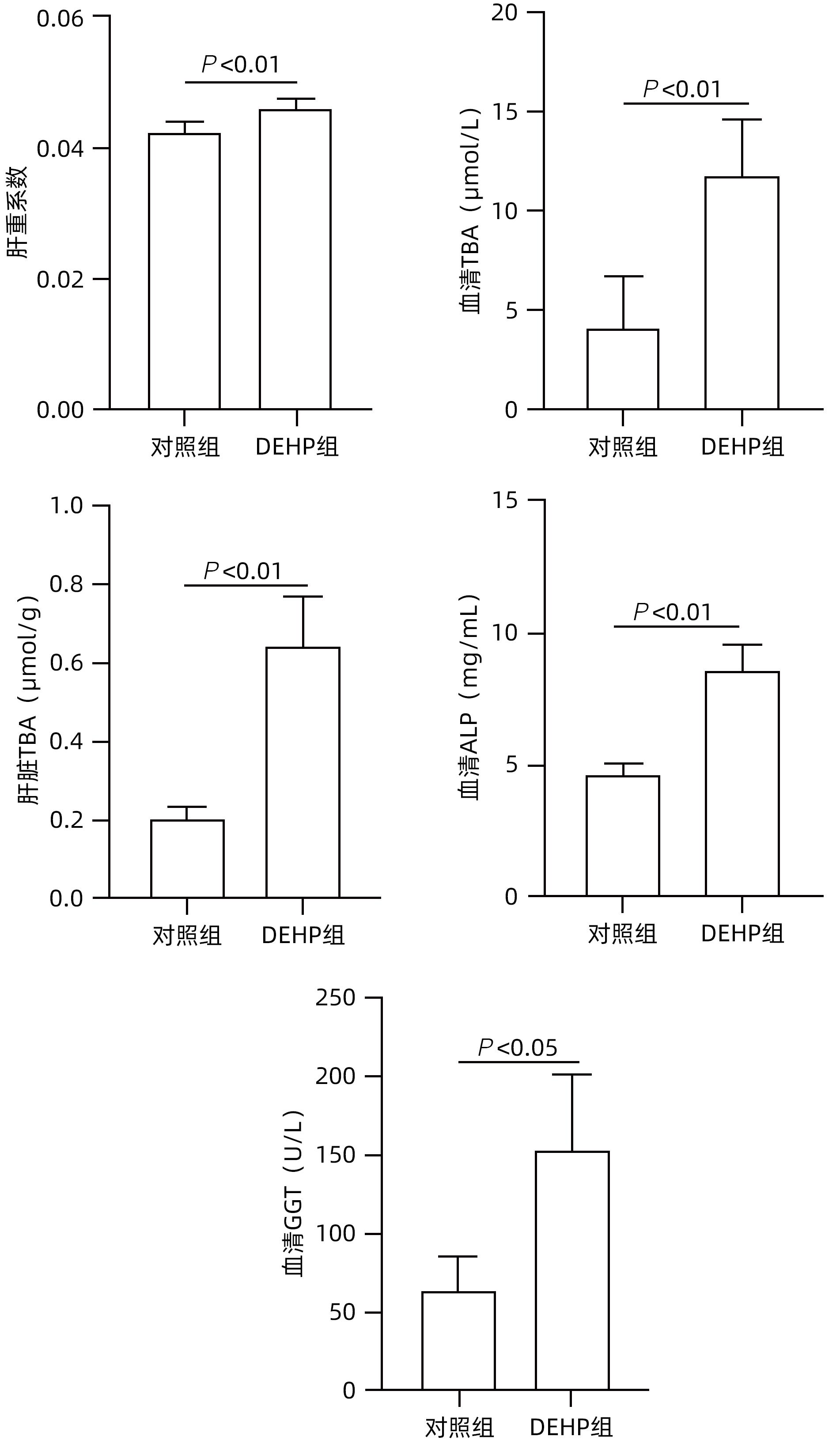
GAITANTZI H, HAKENBERG P, THEOBALD J, et al. Di(2-ethylhexyl) phthalate and its role in developing cholestasis: An in vitro study on different liver cell types[J]. J Pediatr Gastroenterol Nutr, 2018, 66( 2): e28- e35. DOI: 10.1097/MPG.0000000000001813. |
| [6] |
QU MC, ZHAO F, ZHANG C, et al. Protective effect of obeticholic acid on cholestasis induced by subacute exposure to DEHP in mice[J]. Acta Univ Med Anhui, 2022, 57( 10): 1608- 1613. DOI: 10.19405/j.cnki.issn1000-1492.2022.10.018. |
| [7] |
PREECE AS, SHU H, KNUTZ M, et al. Indoor phthalate exposure and contributions to total intake among pregnant women in the SELMA study[J]. Indoor Air, 2021, 31( 5): 1495- 1508. DOI: 10.1111/ina.12813. |
| [8] |
ZHANG YX, HUANG B, HE H, et al. Urinary phthalate metabolites among workers in plastic greenhouses in Western China[J]. Environ Pollut, 2021, 289: 117939. DOI: 10.1016/j.envpol.2021.117939. |
| [9] |
ZHANG JY, WANG JQ. Research advances in the impact of phthalates on cholestatic liver disease[J]. J Clin Hepatol, 2023, 39( 1): 226- 230. DOI: 10.3969/j.issn.1001-5256.2023.01.035. |
| [10] |
Chinese Society of Hepatology, Chinese Medical Association, Chinese Society of Gastroenterology, Chinese Medical Association, Chinese Society of Infectious Diseases, Chinese Medical Association. Consensus on the diagnosis and treatment of cholestasis liver diseases(2015)[J]. J Clin Hepatol, 2015, 31( 12): 1989- 1999.
中华医学会肝病学分会, 中华医学会消化病分会, 中华医学会感染病学分会. 胆汁淤积性肝病诊断和治疗共识(2015)[J]. 临床肝胆病杂志, 2015, 31( 12): 1989- 1999.
|
| [11] |
GOURLAY T, SAMARTZIS I, STEFANOU D, et al. Inflammatory response of rat and human neutrophils exposed to di-(2-ethyl-hexyl)-phthalate-plasticized polyvinyl chloride[J]. Artif Organs, 2003, 27( 3): 256- 260. DOI: 10.1046/j.1525-1594.2003.07107.x. |
| [12] |
SONG PZ, ZHANG YC, KLAASSEN CD. Dose-response of five bile acids on serum and liver bile Acid concentrations and hepatotoxicty in mice[J]. Toxicol Sci, 2011, 123( 2): 359- 367. DOI: 10.1093/toxsci/kfr177. |






 DownLoad:
DownLoad: