| [1] |
MAKUC J. Management of pancreatogenic diabetes: Challenges and solutions[J]. Diabetes Metab Syndr Obes, 2016, 9: 311- 315. DOI: 10.2147/DMSO.S99701. |
| [2] |
PETROV MS, BASINA M. Diagnosis of endocrine disease: Diagnosing and classifying diabetes in diseases of the exocrine pancreas[J]. Eur J Endocrinol, 2021, 184( 4): R151- R163. DOI: 10.1530/EJE-20-0974. |
| [3] |
|
| [4] |
CHO J, SCRAGG R, PETROV MS. Risk of mortality and hospitalization after post-pancreatitis diabetes mellitus vs type 2 diabetes mellitus: A population-based matched cohort study[J]. Am J Gastroenterol, 2019, 114( 5): 804- 812. DOI: 10.14309/ajg.0000000000000225. |
| [5] |
SANTOS R, COLEMAN HG, CAIRNDUFF V, et al. Clinical prediction models for pancreatic cancer in general and at-risk populations: A systematic review[J]. Am J Gastroenterol, 2023, 118( 1): 26- 40. DOI: 10.14309/ajg.0000000000002022. |
| [6] |
American Diabetes Association. 2. classification and diagnosis of diabetes: Standards of medical care in diabetes-2021[J]. Diabetes Care, 2021, 44( Suppl 1): S15- S33. DOI: 10.2337/dc21-S002. |
| [7] |
LI GQ, SUN JF, ZHANG J, et al. Identification of inflammation-related biomarkers in diabetes of the exocrine pancreas with the use of weighted gene co-expression network analysis[J]. Front Endocrinol, 2022, 13: 839865. DOI: 10.3389/fendo.2022.839865. |
| [8] |
|
| [9] |
ZHANG H, CAI D, BAI X. Macrophages regulate the progression of osteoarthritis[J]. Osteoarthritis Cartilage, 2020, 28( 5): 555- 561. DOI: 10.1016/j.joca.2020.01.007. |
| [10] |
SWAIN SM, ROMAC JMJ, SHAHID RA, et al. TRPV4 channel opening mediates pressure-induced pancreatitis initiated by Piezo1 activation[J]. J Clin Invest, 2020, 130( 5): 2527- 2541. DOI: 10.1172/JCI134111. |
| [11] |
PALLAGI P, MADÁCSY T, VARGA Á, et al. Intracellular Ca 2+ signalling in the pathogenesis of acute pancreatitis: Recent advances and translational perspectives[J]. Int J Mol Sci, 2020, 21( 11): 4005. DOI: 10.3390/ijms21114005. |
| [12] |
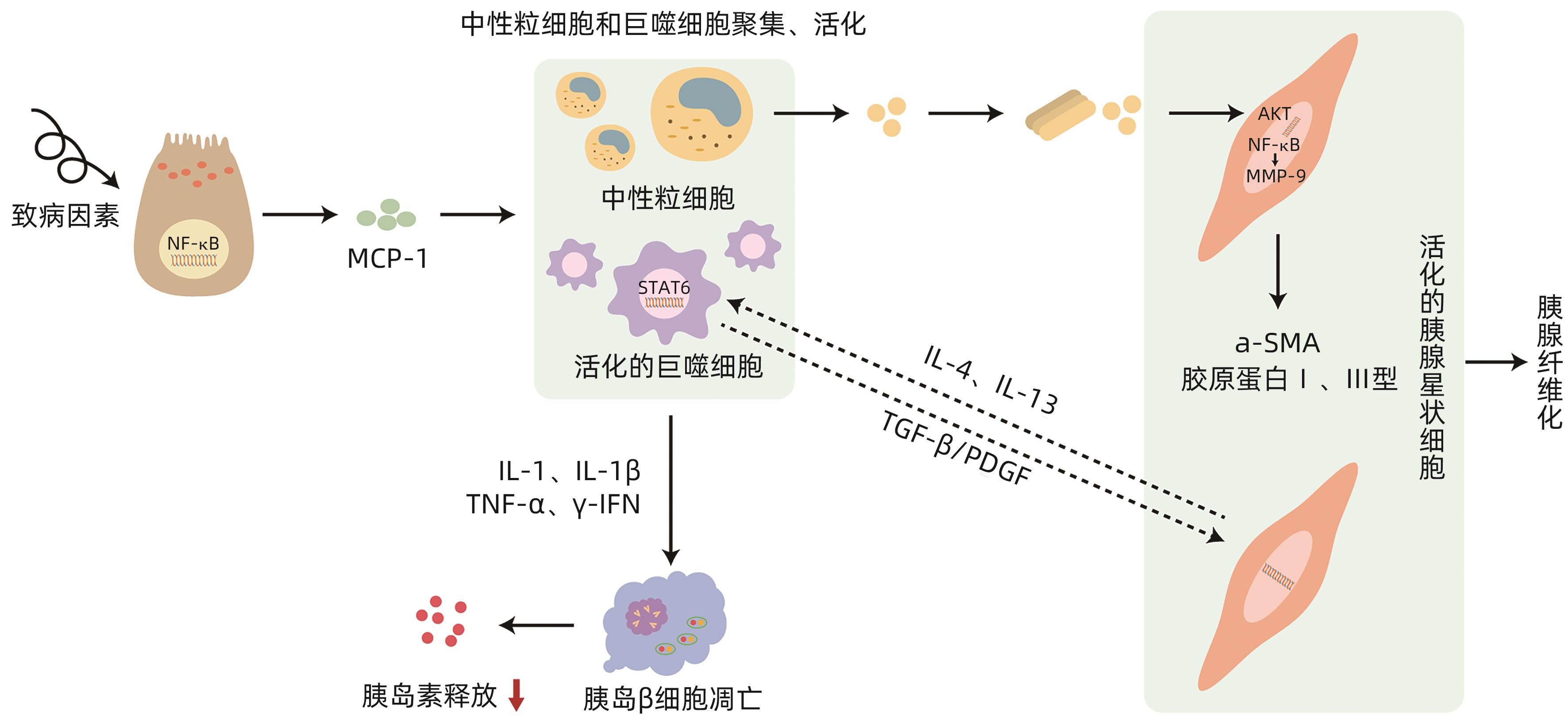
ZHANG Y, ZHANG WQ, LIU XY, et al. Immune cells and immune cell-targeted therapy in chronic pancreatitis[J]. Front Oncol, 2023, 13: 1151103. DOI: 10.3389/fonc.2023.1151103. |
| [13] |
LIU SY, SZATMARY P, LIN JW, et al. Circulating monocytes in acute pancreatitis[J]. Front Immunol, 2022, 13: 1062849. DOI: 10.3389/fimmu.2022.1062849. |
| [14] |
SALUJA A, DUDEJA V, DAWRA R, et al. Early intra-acinar events in pathogenesis of pancreatitis[J]. Gastroenterology, 2019, 156( 7): 1979- 1993. DOI: 10.1053/j.gastro.2019.01.268. |
| [15] |
KRATOCHVILL F, NEALE G, HAVERKAMP JM, et al. TNF counterbalances the emergence of M2 tumor macrophages[J]. Cell Rep, 2015, 12( 11): 1902- 1914. DOI: 10.1016/j.celrep.2015.08.033. |
| [16] |
PAVAN KUMAR P, RADHIKA G, RAO GV, et al. Interferon γ and glycemic status in diabetes associated with chronic pancreatitis[J]. Pancreatology, 2012, 12( 1): 65- 70. DOI: 10.1016/j.pan.2011.12.005. |
| [17] |
CASU AN, GRIPPO PJ, WASSERFALL C, et al. Evaluating the immunopathogenesis of diabetes after acute pancreatitis in the diabetes RElated to acute pancreatitis and its mechanisms study: From the type 1 diabetes in acute pancreatitis consortium[J]. Pancreas, 2022, 51( 6): 580- 585. DOI: 10.1097/MPA.0000000000002076. |
| [18] |
WEN L, JAVED TA, DOBBS AK, et al. The protective effects of calcineurin on pancreatitis in mice depend on the cellular source[J]. Gastroenterology, 2020, 159( 3): 1036- 1050. e 8. DOI: 10.1053/j.gastro.2020.05.051. |
| [19] |
JAGANJAC M, CIPAK A, SCHAUR RJ, et al. Pathophysiology of neutrophil-mediated extracellular redox reactions[J]. Front Biosci(Landmark Ed), 2016, 21( 4): 839- 855. DOI: 10.2741/4423. |
| [20] |
XIA D, HALDER B, GODOY C, et al. NADPH oxidase 1 mediates caerulein-induced pancreatic fibrosis in chronic pancreatitis[J]. Free Radic Biol Med, 2020, 147: 139- 149. DOI: 10.1016/j.freeradbiomed.2019.11.034. |
| [21] |
CANNON A, THOMPSON CM, BHATIA R, et al. Molecular mechanisms of pancreatic myofibroblast activation in chronic pancreatitis and pancreatic ductal adenocarcinoma[J]. J Gastroenterol, 2021, 56( 8): 689- 703. DOI: 10.1007/s00535-021-01800-4. |
| [22] |
SCHMITZ-WINNENTHAL H, PIETSCH DH, SCHIMMACK S, et al. Chronic pancreatitis is associated with disease-specific regulatory T-cell responses[J]. Gastroenterology, 2010, 138( 3): 1178- 1188. DOI: 10.1053/j.gastro.2009.11.011. |
| [23] |
ZHOU Q, TAO XF, XIA SL, et al. T lymphocytes: A promising immunotherapeutic target for pancreatitis and pancreatic cancer?[J]. Front Oncol, 2020, 10: 382. DOI: 10.3389/fonc.2020.00382. |
| [24] |
GLAUBITZ J, WILDEN A, GOLCHERT J, et al. In mouse chronic pancreatitis CD25 +FOXP3 + regulatory T cells control pancreatic fibrosis by suppression of the type 2 immune response[J]. Nat Commun, 2022, 13( 1): 4502. DOI: 10.1038/s41467-022-32195-2. |
| [25] |
CHANG M, CHEN WJ, XIA RT, et al. Pancreatic stellate cells and the targeted therapeutic strategies in chronic pancreatitis[J]. Molecules, 2023, 28( 14): 5586. DOI: 10.3390/molecules28145586. |
| [26] |
RABIEE A, GALIATSATOS P, SALAS-CARRILLO R, et al. Pancreatic polypeptide administration enhances insulin sensitivity and reduces the insulin requirement of patients on insulin pump therapy[J]. J Diabetes Sci Technol, 2011, 5( 6): 1521- 1528. DOI: 10.1177/193229681100500629. |
| [27] |
APTE M, PIROLA R, WILSON J. The fibrosis of chronic pancreatitis: New insights into the role of pancreatic stellate cells[J]. Antioxid Redox Signal, 2011, 15( 10): 2711- 2722. DOI: 10.1089/ars.2011.4079. |
| [28] |
RAMAKRISHNAN P, LOH WM, GOPINATH SCB, et al. Selective phytochemicals targeting pancreatic stellate cells as new anti-fibrotic agents for chronic pancreatitis and pancreatic cancer[J]. Acta Pharm Sin B, 2020, 10( 3): 399- 413. DOI: 10.1016/j.apsb.2019.11.008. |
| [29] |
BYNIGERI RR, JAKKAMPUDI A, JANGALA R, et al. Pancreatic stellate cell: Pandora’s box for pancreatic disease biology[J]. World J Gastroenterol, 2017, 23( 3): 382- 405. DOI: 10.3748/wjg.v23.i3.382. |
| [30] |
ARUMUGAM T, BRANDT W, RAMACHANDRAN V, et al. Trefoil factor 1 stimulates both pancreatic cancer and stellate cells and increases metastasis[J]. Pancreas, 2011, 40( 6): 815- 822. DOI: 10.1097/MPA.0b013e31821f6927. |
| [31] |
LEE SH, PARK SY, CHOI CS. Insulin resistance: From mechanisms to therapeutic strategies[J]. Diabetes Metab J, 2022, 46( 1): 15- 37. DOI: 10.4093/dmj.2021.0280. |
| [32] |
OLESEN SS, SVANE HML, NICOLAISEN SK, et al. Clinical and biochemical characteristics of postpancreatitis diabetes mellitus: A cross-sectional study from the Danish nationwide DD2 cohort[J]. J Diabetes, 2021, 13( 12): 960- 974. DOI: 10.1111/1753-0407.13210. |
| [33] |
ASLAM M, VIJAYASARATHY K, TALUKDAR R, et al. Reduced pancreatic polypeptide response is associated with early alteration of glycemic control in chronic pancreatitis[J]. Diabetes Res Clin Pract, 2020, 160: 107993. DOI: 10.1016/j.diabres.2019.107993. |
| [34] |
HENNIG R, KEKIS PB, FRIESS H, et al. Pancreatic polypeptide in pancreatitis[J]. Peptides, 2002, 23( 2): 331- 338. DOI: 10.1016/s0196-9781(01)00605-2. |
| [35] |
GOODARZI MO, PETROV MS. Diabetes of the exocrine pancreas: Implications for pharmacological management[J]. Drugs, 2023, 83( 12): 1077- 1090. DOI: 10.1007/s40265-023-01913-5. |
| [36] |
GOLDSTEIN JA, KIRWIN JD, SEYMOUR NE, et al. Reversal of in vitro hepatic insulin resistance in chronic pancreatitis by pancreatic polypeptide in the rat[J]. Surgery, 1989, 106( 6): 1128-1132; discussion 1132-1133.
|
| [37] |
CAI DS, YUAN MS, FRANTZ DF, et al. Local and systemic insulin resistance resulting from hepatic activation of IKK-beta and NF-kappaB[J]. Nat Med, 2005, 11( 2): 183- 190. DOI: 10.1038/nm1166. |
| [38] |
HEO YJ, CHOI SE, JEON JY, et al. Visfatin induces inflammation and insulin resistance via the NF-κB and STAT3 signaling pathways in hepatocytes[J]. J Diabetes Res, 2019, 2019: 4021623. DOI: 10.1155/2019/4021623. |
| [39] |
SAH RP, NAGPAL SJ, MUKHOPADHYAY D, et al. New insights into pancreatic cancer-induced paraneoplastic diabetes[J]. Nat Rev Gastroenterol Hepatol, 2013, 10( 7): 423- 433. DOI: 10.1038/nrgastro.2013.49. |
| [40] |
YARIBEYGI H, FARROKHI FR, BUTLER AE, et al. Insulin resistance: Review of the underlying molecular mechanisms[J]. J Cell Physiol, 2019, 234( 6): 8152- 8161. DOI: 10.1002/jcp.27603. |
| [41] |
ZHOU XL, YOU SY. Rosiglitazone inhibits hepatic insulin resistance induced by chronic pancreatitis and IKK-β/NF-κB expression in liver[J]. Pancreas, 2014, 43( 8): 1291- 1298. DOI: 10.1097/MPA.0000000000000173. |
| [42] |
WENTWORTH JM, ZHANG JG, BANDALA-SANCHEZ E, et al. Interferon-gamma released from omental adipose tissue of insulin-resistant humans alters adipocyte phenotype and impairs response to insulin and adiponectin release[J]. Int J Obes, 2017, 41( 12): 1782- 1789. DOI: 10.1038/ijo.2017.180. |
| [43] |
REHMAN K, AKASH MSH, LIAQAT A, et al. Role of interleukin-6 in development of insulin resistance and type 2 diabetes mellitus[J]. Crit Rev Eukaryot Gene Expr, 2017, 27( 3): 229- 236. DOI: 10.1615/CritRevEukaryotGeneExpr.2017019712. |
| [44] |
AKBARI M, HASSAN-ZADEH V. IL-6 signalling pathways and the development of type 2 diabetes[J]. Inflammopharmacology, 2018, 26( 3): 685- 698. DOI: 10.1007/s10787-018-0458-0. |
| [45] |
DOU L, ZHAO T, WANG LL, et al. MiR-200s contribute to interleukin-6(IL-6)-induced insulin resistance in hepatocytes[J]. J Biol Chem, 2013, 288( 31): 22596- 22606. DOI: 10.1074/jbc.M112.423145. |
| [46] |
DOU L, WANG SY, SUI XF, et al. MiR-301a mediates the effect of IL-6 on the AKT/GSK pathway and hepatic glycogenesis by regulating PTEN expression[J]. Cell Physiol Biochem, 2015, 35( 4): 1413- 1424. DOI: 10.1159/000373962. |
| [47] |
CHEANG JY, MOYLE PM. Glucagon-like peptide-1(GLP-1)-based therapeutics: Current status and future opportunities beyond type 2 diabetes[J]. ChemMedChem, 2018, 13( 7): 662- 671. DOI: 10.1002/cmdc.201700781. |
| [48] |
TUDURÍ E, LÓPEZ M, DIÉGUEZ C, et al. Glucagon-like peptide 1 analogs and their effects on pancreatic islets[J]. Trends Endocrinol Metab, 2016, 27( 5): 304- 318. DOI: 10.1016/j.tem.2016.03.004. |
| [49] |
DRUCKER DJ. Mechanisms of action and therapeutic application of glucagon-like peptide-1[J]. Cell Metab, 2018, 27( 4): 740- 756. DOI: 10.1016/j.cmet.2018.03.001. |
| [50] |
ZHOU Z, SUN B, YU DS, et al. Gut microbiota: An important player in type 2 diabetes mellitus[J]. Front Cell Infect Microbiol, 2022, 12: 834485. DOI: 10.3389/fcimb.2022.834485. |
| [51] |
TILG H, ZMORA N, ADOLPH TE, et al. The intestinal microbiota fuelling metabolic inflammation[J]. Nat Rev Immunol, 2020, 20( 1): 40- 54. DOI: 10.1038/s41577-019-0198-4. |
| [52] |
TAO J, CHEEMA H, KESH K, et al. Chronic pancreatitis in a caerulein-induced mouse model is associated with an altered gut microbiome[J]. Pancreatology, 2022, 22( 1): 30- 42. DOI: 10.1016/j.pan.2021.12.003. |
| [53] |
ARON-WISNEWSKY J, WARMBRUNN MV, NIEUWDORP M, et al. Metabolism and metabolic disorders and the microbiome: The intestinal microbiota associated with obesity, lipid metabolism, and metabolic health-pathophysiology and therapeutic strategies[J]. Gastroenterology, 2021, 160( 2): 573- 599. DOI: 10.1053/j.gastro.2020.10.057. |
| [54] |
TALUKDAR R, SARKAR P, JAKKAMPUDI A, et al. The gut microbiome in pancreatogenic diabetes differs from that of Type 1 and Type 2 diabetes[J]. Sci Rep, 2021, 11( 1): 10978. DOI: 10.1038/s41598-021-90024-w. |
| [55] |
JANDHYALA SM, MADHULIKA A, DEEPIKA G, et al. Altered intestinal microbiota in patients with chronic pancreatitis: Implications in diabetes and metabolic abnormalities[J]. Sci Rep, 2017, 7: 43640. DOI: 10.1038/srep43640. |
| [56] |
ZOU WB, TANG XY, ZHOU DZ, et al. SPINK1, PRSS1, CTRC, and CFTR genotypes influence disease onset and clinical outcomes in chronic pancreatitis[J]. Clin Transl Gastroenterol, 2018, 9( 11): 204. DOI: 10.1038/s41424-018-0069-5. |
| [57] |
CHEN JM, FÉREC C. Genetics and pathogenesis of chronic pancreatitis: The 2012 update[J]. Clin Res Hepatol Gastroenterol, 2012, 36( 4): 334- 340. DOI: 10.1016/j.clinre.2012.05.003. |
| [58] |
MASSON E, CHEN JM, AUDRÉZET MP, et al. A conservative assessment of the major genetic causes of idiopathic chronic pancreatitis: Data from a comprehensive analysis of PRSS1, SPINK1, CTRC and CFTR genes in 253 young French patients[J]. PLoS One, 2013, 8( 8): e73522. DOI: 10.1371/journal.pone.0073522. |
| [59] |
LIU QC, ZHUANG ZH, ZENG K, et al. Prevalence of pancreatic diabetes in patients carrying mutations or polymorphisms of the PRSS1 gene in the Han population[J]. Diabetes Technol Ther, 2009, 11( 12): 799- 804. DOI: 10.1089/dia.2009.0051. |






 DownLoad:
DownLoad: