| [1] |
AUGUSTINUS S, MACKAY TM, ANDERSSON B, et al. Ideal outcome after pancreatoduodenectomy: A transatlantic evaluation of a harmonized composite outcome measure[J]. Ann Surg, 2023, 278( 5): 740- 747. DOI: 10.1097/SLA.0000000000006037. |
| [2] |
WANG Z, LYU X, YU JA, et al. Pathogenesis of delayed gastric emptying after pancreaticoduodenectomy and related risk factors[J]. J Clin Hepatol, 2023, 39( 2): 474- 480. DOI: 10.3969/j.issn.1001-5256.2023.02.036. |
| [3] |
GAO HQ, LI BY, MA YS, et al. Risk factors analysis and treatment of postpancreaticoduodenectomy hemorrhage[J]. Chin J Dig Surg, 2022, 21( 4): 492- 499. DOI: 10.3760/cma.j.cn115610-20220228-00111. |
| [4] |
MARCHEGIANI G. The 2016 update of the International Study Group(ISGPS) definition and grading of postoperative pancreatic fistula: 11 Years After[J]. HPB, 2019, 21: S748. DOI: 10.1016/j.hpb.2019.10.1473. |
| [5] |
AMBROSETTI MC, AMBROSETTI A, PERRI G, et al. Quantitative edge analysis of pancreatic margins in patients with head pancreatic tumors: Correlations between pancreatic margins and the onset of postoperative pancreatic fistula[J]. Eur Radiol, 2024, 34( 3): 1515- 1523. DOI: 10.1007/s00330-023-10200-6. |
| [6] |
LIU L, XU ZH, WANG WQ, et al. Prevention and management of pancreatic fistula after pancreatoduodenectomy with precise and comprehensive opinion[J]. Chin J Dig Surg, 2023, 22( 5): 657- 662. DOI: 10.3760/cma.j.cn115610-20230401-00143. |
| [7] |
POTTER KC, SUTTON TL, O’GRADY J, et al. Risk factors for postoperative pancreatic fistula in the Era of pasireotide[J]. Am J Surg, 2022, 224( 2): 733- 736. DOI: 10.1016/j.amjsurg.2022.02.050. |
| [8] |
RAMACCIATO G, MERCANTINI P, PETRUCCIANI N, et al. Risk factors of pancreatic fistula after pancreaticoduodenectomy: A collective review[J]. Am Surg, 2011, 77( 3): 257- 269.
|
| [9] |
KAMARAJAH SK, BUNDRED JR, LIN A, et al. Systematic review and meta-analysis of factors associated with post-operative pancreatic fistula following pancreatoduodenectomy[J]. ANZ J Surg, 2021, 91( 5): 810- 821. DOI: 10.1111/ans.16408. |
| [10] |
ZHANG B, YUAN QH, LI S, et al. Risk factors of clinically relevant postoperative pancreatic fistula after pancreaticoduodenectomy: A systematic review and meta-analysis[J]. Medicine, 2022, 101( 26): e29757. DOI: 10.1097/MD.0000000000029757. |
| [11] |
LI Y, SHI YB, TU JH, et al. Risk factors and prophylaxis for pancreatic fistula after pancreaticoduodenectomy[J/OL]. Chin J Hepat Surg(Electronic Edition), 2023, 12( 3): 352- 355. DOI: 10.3877/cma.j.issn.2095-3232.2023.03.021. |
| [12] |
RAZA SS, NUTU A, POWELL-BRETT S, et al. Early postoperative risk stratification in patients with pancreatic fistula after pancreaticoduodenectomy[J]. Surgery, 2023, 173( 2): 492- 500. DOI: 10.1016/j.surg.2022.09.008. |
| [13] |
GUO CX, SHEN YN, ZHANG Q, et al. Prediction of postoperative pancreatic fistula using a nomogram based on the updated definition[J]. Ann Surg Treat Res, 2020, 98( 2): 72- 81. DOI: 10.4174/astr.2020.98.2.72. |
| [14] |
SHEN J, GUO F, SUN Y, et al. Predictive nomogram for postoperative pancreatic fistula following pancreaticoduodenectomy: A retrospective study[J]. BMC Cancer, 2021, 21( 1): 550. DOI: 10.1186/s12885-021-08201-z. |
| [15] |
CHOI M, LEE JH, ROH YH, et al. Multidimensional nomogram to predict postoperative pancreatic fistula after minimally invasive pancreaticoduodenectomy[J]. Ann Surg Oncol, 2023, 30( 8): 5083- 5090. DOI: 10.1245/s10434-023-13360-3. |
| [16] |
YOU Y, HAN IW, CHOI DW, et al. Nomogram for predicting postoperative pancreatic fistula[J]. HPB(Oxford), 2019, 21( 11): 1436- 1445. DOI: 10.1016/j.hpb.2019.03.351. |
| [17] |
ZHOU Z, WANG R, WANG H, et al. Myocardial extracellular volume fraction quantification in an animal model of the doxorubicin-induced myocardial fibrosis: A synthetic hematocrit method using 3T cardiac magnetic resonance[J]. Quant Imaging Med Surg, 2021, 11( 2): 510- 520. DOI: 10.21037/qims-20-501. |
| [18] |
CAVALCANTE JL, KOIKE H. The rise of myocardial extracellular volume fraction in computed tomography for identification of cardiac amyloidosis[J]. JACC Cardiovasc Imaging, 2022, 15( 12): 2095- 2097. DOI: 10.1016/j.jcmg.2022.09.010. |
| [19] |
MESROPYAN N, KUPCZYK P, ISAAK A, et al. Synthetic extracellular volume fraction without hematocrit sampling for hepatic applications[J]. Abdom Radiol, 2021, 46( 10): 4637- 4646. DOI: 10.1007/s00261-021-03140-6. |
| [20] |
TAKAHASHI M, TAKAOKA H, YASHIMA S, et al. Extracellular volume fraction by computed tomography predicts prognosis after transcatheter aortic valve replacement[J]. Circ J, 2024, 88( 4): 492- 500. DOI: 10.1253/circj.CJ-23-0288. |
| [21] |
OZAKI K, OHTANI T, ISHIDA S, et al. Extracellular volume fraction obtained by dual-energy CT depicting the etiological differences of liver fibrosis[J]. Abdom Radiol, 2023, 48( 6): 1975- 1986. DOI: 10.1007/s00261-023-03873-6. |
| [22] |
ZHU L, SUN ZY, DAI MH, et al. Tomoelastography and pancreatic extracellular volume fraction derived from MRI for predicting clinically relevant postoperative pancreatic fistula[J]. J Magn Reson Imaging, 2024, 59( 3): 1074- 1082. DOI: 10.1002/jmri.28788. |
| [23] |
SOFUE K, UESHIMA E, MASUDA A, et al. Estimation of pancreatic fibrosis and prediction of postoperative pancreatic fistula using extracellular volume fraction in Multiphasic contrast-enhanced CT[J]. Eur Radiol, 2022, 32( 3): 1770- 1780. DOI: 10.1007/s00330-021-08255-4. |
| [24] |
Study Group of Pancreatic Surgery in Chinese Society of Surgery of Chinese Medical Association, Pancreatic Disease Committee of Chinese Research Hospital Association, Editorial Board of Chinese Journal of Surgery. A consensus statement on the diagnosis, treatment, and prevention of common complications after pancreatic surgery(2017)[J]. Chin J Surg, 2017, 55( 5): 328- 334. DOI: 10.3760/cma.j.issn.0529-5815.2017.05.003. |
| [25] |
HANAKI T, UEJIMA C, AMISAKI M, et al. The attenuation value of preoperative computed tomography as a novel predictor for pancreatic fistula after pancreaticoduodenectomy[J]. Surg Today, 2018, 48( 6): 598- 608. DOI: 10.1007/s00595-018-1626-y. |
| [26] |
KIM SY, KIM H, CHO JY, et al. Quantitative assessment of pancreatic fat by using unenhanced CT: Pathologic correlation and clinical implications[J]. Radiology, 2014, 271( 1): 104- 112. DOI: 10.1148/radiol.13122883. |
| [27] |
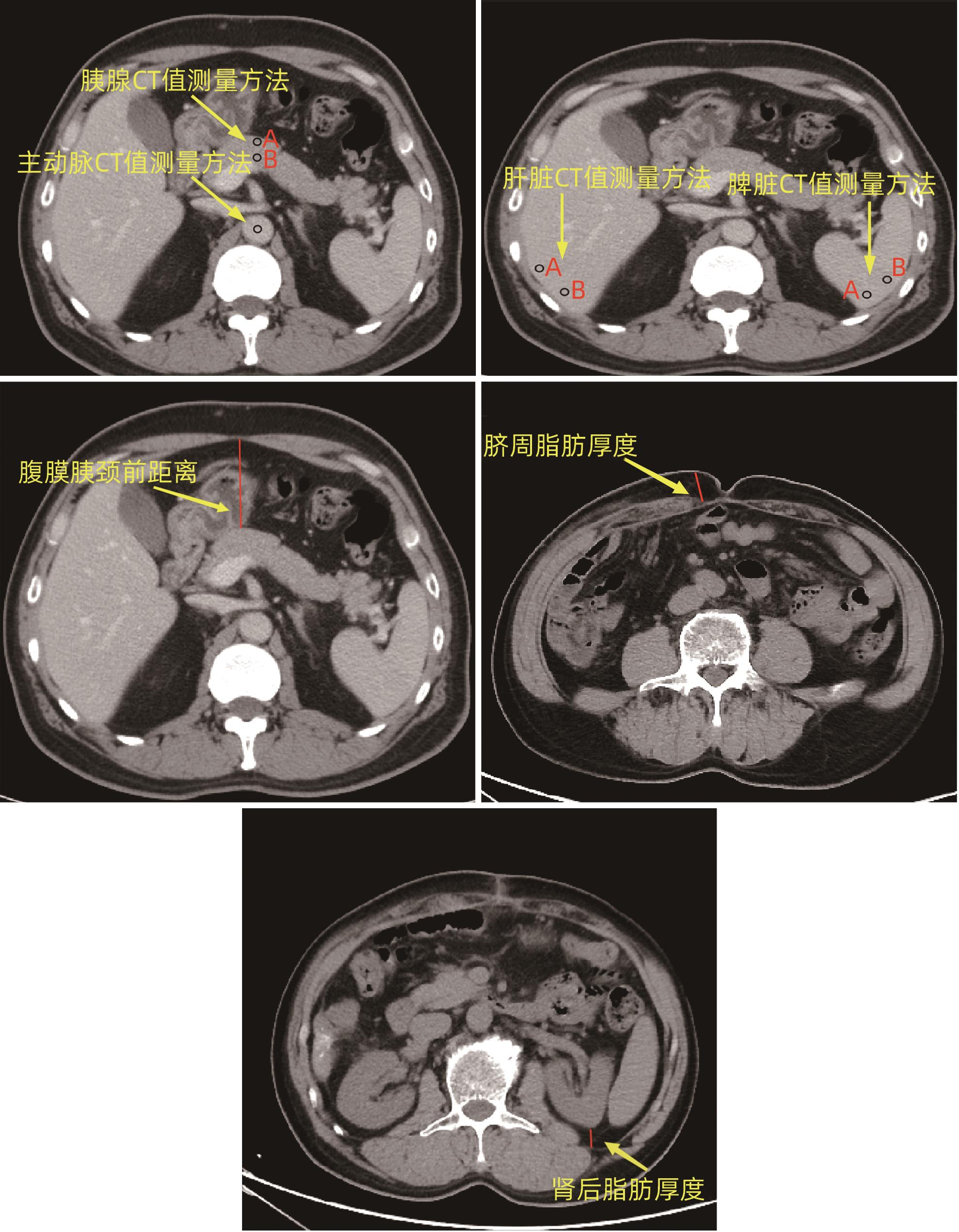
ZHAO ZR, ZHOU LC, HAN L, et al. The visceral pancreatic neck anterior distance may be an effective parameter to predict post-pancreaticoduodenectomy clinically relevant postoperative pancreatic fistula[J]. Heliyon, 2023, 9( 2): e13660. DOI: 10.1016/j.heliyon.2023.e13660. |
| [28] |
TANAKA K, YAMADA S, SONOHARA F, et al. Pancreatic fat and body composition measurements by computed tomography are associated with pancreatic fistula after pancreatectomy[J]. Ann Surg Oncol, 2021, 28( 1): 530- 538. DOI: 10.1245/s10434-020-08581-9. |
| [29] |
CALLERY MP, PRATT WB, KENT TS, et al. A prospectively validated clinical risk score accurately predicts pancreatic fistula after pancreatoduodenectomy[J]. J Am Coll Surg, 2013, 216( 1): 1- 14. DOI: 10.1016/j.jamcollsurg.2012.09.002. |
| [30] |
GU ZT, DU YX, WANG P, et al. Development and validation of a novel nomogram to predict postoperative pancreatic fistula after pancreatoduodenectomy using lasso-logistic regression: An international multi-institutional observational study[J]. Int J Surg, 2023, 109( 12): 4027- 4040. DOI: 10.1097/JS9.0000000000000695. |
| [31] |
WANG CY, OU HY, CHEN MF, et al. Enigmatic ectopic fat: Prevalence of nonalcoholic fatty pancreas disease and its associated factors in a Chinese population[J]. J Am Heart Assoc, 2014, 3( 1): e000297. DOI: 10.1161/JAHA.113.000297. |
| [32] |
PECORELLI N, PALUMBO D, GUARNERI G, et al. Preoperative CT image analysis to improve risk stratification for clinically relevant pancreatic fistula after distal pancreatectomy[J]. Br J Surg, 2023, 110( 8): 891- 895. DOI: 10.1093/bjs/znac348. |
| [33] |
LEE SE, JANG JY, LIM CS, et al. Measurement of pancreatic fat by magnetic resonance imaging: Predicting the occurrence of pancreatic fistula after pancreatoduodenectomy[J]. Ann Surg, 2010, 251( 5): 932- 936. DOI: 10.1097/SLA.0b013e3181d65483. |
| [34] |
SALTIEL AR, OLEFSKY JM. Inflammatory mechanisms linking obesity and metabolic disease[J]. J Clin Invest, 2017, 127( 1): 1- 4. DOI: 10.1172/JCI92035. |
| [35] |
WANG ZY, LIU RH, LI FS, et al. Analysis of relative factors of pancreatic leakage after laparoscopic pancreaticoduodenectomy[J]. Chin J Minim Invasive Surg, 2019, 19( 2): 106- 110. DOI: 10.3969/j.issn.1009-6604.2019.02.003. |
| [36] |
SERT OZ, BERKESOGLU M, CANBAZ H, et al. The factors of pancreatic fistula development in patients who underwent classical pancreaticoduodenectomy[J]. Ann Ital Chir, 2021, 92: 35- 40.
|
| [37] |
ZHOU LC, TAN Z, TANG YP, et al. Value of pancreatic anatomic structure under standard pancreatic neck transection in predicting pancreatic fistula after pancreaticoduodenectomy[J]. J Clin Hepatol, 2022, 38( 12): 2807- 2813. DOI: 10.3969/j.issn.1001-5256.2022.12.022. |
| [38] |
SCHUH F, MIHALJEVIC AL, PROBST P, et al. A simple classification of pancreatic duct size and texture predicts postoperative pancreatic fistula: A classification of the international study group of pancreatic surgery[J]. Ann Surg, 2023, 277( 3): e597- e608. DOI: 10.1097/SLA.0000000000004855. |
| [39] |
HAN D, LIN A, KURONUMA K, et al. Cardiac computed tomography for quantification of myocardial extracellular volume fraction: A systematic review and meta-analysis[J]. JACC Cardiovasc Imaging, 2023, 16( 10): 1306- 1317. DOI: 10.1016/j.jcmg.2023.03.021. |
| [40] |
OZAKI K, OHTANI T, ISHIDA T, et al. Liver fibrosis estimated using extracellular volume fraction obtained from dual-energy CT as a risk factor for hepatocellular carcinoma after sustained virologic response: A preliminary case-control study[J]. Eur J Radiol, 2023, 168: 111112. DOI: 10.1016/j.ejrad.2023.111112. |
| [41] |
GUO WX, LV BL, YANG T, et al. Role of dynamic contrast-enhanced magnetic resonance imaging parameters and extracellular volume fraction as predictors of lung cancer subtypes and lymph node status in non-small-cell lung cancer patients[J]. J Cancer, 2023, 14( 16): 3108- 3116. DOI: 10.7150/jca.88367. |






 DownLoad:
DownLoad: