| [1] |
RONG L, ZOU JY, RAN W, et al. Advancements in the treatment of non-alcoholic fatty liver disease(NAFLD)[J]. Front Endocrinol(Lausanne), 2023, 13: 1087260. DOI: 10.3389/fendo.2022.1087260. |
| [2] |
ALMOMANI A, KUMAR P, ONWUZO S, et al. Epidemiology and prevalence of lean nonalcoholic fatty liver disease and associated cirrhosis, hepatocellular carcinoma, and cardiovascular outcomes in the United States: A population-based study and review of literature[J]. J Gastroenterol Hepatol, 2023, 38( 2): 269- 273. DOI: 10.1111/jgh.16049. |
| [3] |
TANG HY, LV FR, ZHANG P, et al. The impact of obstructive sleep apnea on nonalcoholic fatty liver disease[J]. Front Endocrinol(Lausanne), 2023, 14: 1254459. DOI: 10.3389/fendo.2023.1254459. |
| [4] |
IBRAHIM MK, SIMON TG, RINELLA ME. Extrahepatic outcomes of nonalcoholic fatty liver disease: Nonhepatocellular cancers[J]. Clin Liver Dis, 2023, 27( 2): 251- 273. DOI: 10.1016/j.cld.2023.01.004. |
| [5] |
PAIK JM, HENRY L, YOUNOSSI Y, et al. The burden of nonalcoholic fatty liver disease(NAFLD) is rapidly growing in every region of the world from 1990 to 2019[J]. Hepatol Commun, 2023, 7( 10): e0251. DOI: 10.1097/HC9.0000000000000251. |
| [6] |
YOUNOSSI ZM, GOLABI P, PAIK JM, et al. The global epidemiology of nonalcoholic fatty liver disease(NAFLD) and nonalcoholic steatohepatitis(NASH): A systematic review[J]. Hepatology, 2023, 77( 4): 1335- 1347. DOI: 10.1097/HEP.0000000000000004. |
| [7] |
LU R, LIU Y, HONG TP. Epidemiological characteristics and management of nonalcoholic fatty liver disease/nonalcoholic steatohepatitis in China: A narrative review[J]. Diabetes Obes Metab, 2023, 25( Suppl 1): 13- 26. DOI: 10.1111/dom.15014. |
| [8] |
NI WJ, GENG N, BAI X, et al. An excerpt of EASL-EASD-EASO clinical practice guidelines on the management of metabolic dysfunctionassociated steatotic liver disease in 2024[J]. J Clin Hepatol, 2024, 40( 8): 1567- 1574. DOI: 10.12449/JCH240810. 倪文婧, 耿楠, 白雪, 等.《2024年欧洲肝病学会/欧洲糖尿病学会/欧洲肥胖症学会临床实践指南: 代谢相关脂肪性肝病的管理》摘译[J]. 临床肝胆病杂志, 2024, 40( 8): 1567- 1574. DOI: 10.12449/JCH240810. |
| [9] |
BABKOVA K, KORABECNY J, SOUKUP O, et al. Prolyl oligopeptidase and its role in the organism: Attention to the most promising and clinically relevant inhibitors[J]. Future Med Chem, 2017, 9( 10): 1015- 1038. DOI: 10.4155/fmc-2017-0030. |
| [10] |
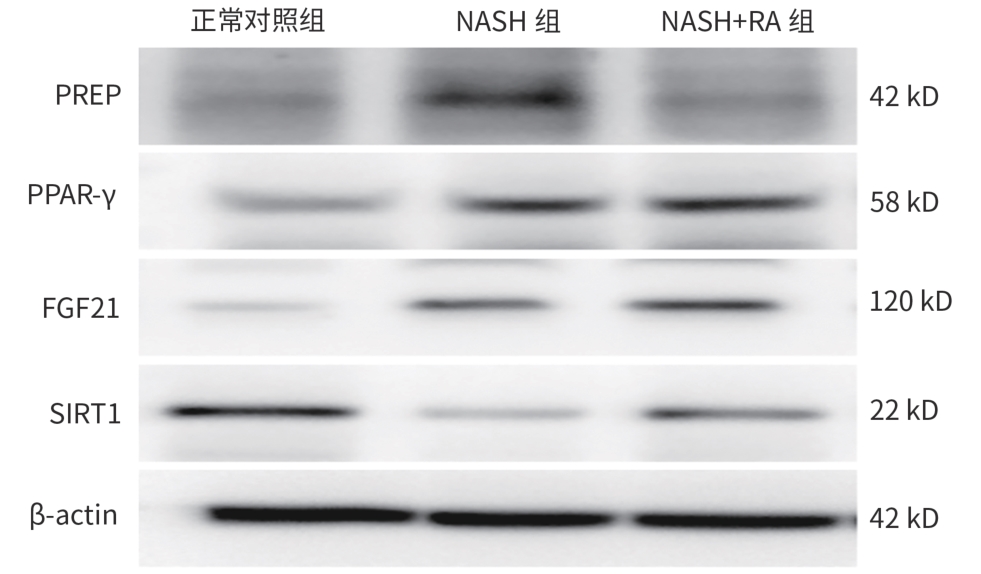
LI MT, JIANG DX, ZHANG JB, et al. Effects of sodium valproate on the progression of non-alcoholic fatty liver disease by inhibiting prolyl endopeptidase activity[J]. J Wenzhou Med Univ, 2022, 52( 8): 657- 662. DOI: 10.3969/j.issn.2095-9400.2022.08.009. |
| [11] |
JIANG DX, ZHANG JB, LI MT, et al. Prolyl endopeptidase gene disruption attenuates high fat diet-induced nonalcoholic fatty liver disease in mice by improving hepatic steatosis and inflammation[J]. Ann Transl Med, 2020, 8( 5): 218. DOI: 10.21037/atm.2020.01.14. |
| [12] |
ZHOU D, LI BH, WANG J, et al. Prolyl oligopeptidase inhibition attenuates steatosis in the L02 human liver cell line[J]. PLoS One, 2016, 11( 10): e0165224. DOI: 10.1371/journal.pone.0165224. |
| [13] |
SAMUEL VT, SHULMAN GI. Nonalcoholic fatty liver disease as a nexus of metabolic and hepatic diseases[J]. Cell Metab, 2018, 27( 1): 22- 41. DOI: 10.1016/j.cmet.2017.08.002. |
| [14] |
WANG ZY, SUN TT, YU JJ, et al. FGF21: A sharp weapon in the process of exercise to improve NAFLD[J]. Front Biosci(Landmark Ed), 2023, 28( 12): 351. DOI: 10.31083/j.fbl2812351. |
| [15] |
BARROSO LN, SALARINI J, LEITE NC, et al. Effect of fish oil supplementation on the concentration of miRNA-122, FGF-21 and liver fibrosis in patients with NAFLD: Study protocol for a randomized, double-blind and placebo-controlled clinical trial[J]. Clin Nutr ESPEN, 2023, 57: 117- 125. DOI: 10.1016/j.clnesp.2023.06.027. |
| [16] |
NAN Y, XIANGLI W, ZHANG W, et al. FGF21 inhibits lipid accumulation and inflammation induced by palmitate in human hepatocytes via SIRT1 pathway[J]. Chin J Cell Mol Immunol, 2019, 35( 7): 606- 612. DOI: 10.13423/j.cnki.cjcmi.008839. 南瑛, 相里伟, 张薇, 等. 成纤维细胞生长因子21(FGF21)通过SIRT1通路抑制棕榈酸酯诱导的人肝细胞脂肪堆积和炎症反应[J]. 细胞与分子免疫学杂志, 2019, 35( 7): 606- 612. DOI: 10.13423/j.cnki.cjcmi.008839. |
| [17] |
WU YS. Exosomes derived from lipotoxic hepatocytes in inducing LSEC capillarization and promoting the progression of non-alcoholic fatty liver disease[D]. Zhenjiang: Jiangsu University, 2022.
武艳霜. 脂毒性损伤肝细胞分泌外泌体诱导LSEC毛细血管化促进NAFLD进展[D]. 镇江: 江苏大学, 2022.
|
| [18] |
LI YQ, TANG WJ, ZHOU YJ. Role of intestinal microbiota and metabolites in the development, progression, and treatment of nonalcoholic fatty liver disease[J]. J Clin Hepatol, 2023, 39( 8): 1805- 1810. DOI: 10.3969/j.issn.1001-5256.2023.08.006. |
| [19] |
YIN JY, WANG Q. Progress on adipokines in non-alcoholic fatty liver disease[J/CD]. Chin J Liver Dis(Electronic Version), 2023, 15( 1): 1- 5. DOI: 10.3969/j.issn.1674-7380.2023.01.001. |
| [20] |
HÖFLING C, KULESSKAYA N, JAAKO K, et al. Deficiency of prolyl oligopeptidase in mice disturbs synaptic plasticity and reduces anxiety-like behaviour, body weight, and brain volume[J]. Eur Neuropsychopharmacol, 2016, 26( 6): 1048- 1061. DOI: 10.1016/j.euroneuro.2016.02.015. |
| [21] |
RAPTIS DD, MANTZOROS CS, POLYZOS SA. Fibroblast growth factor-21 as a potential therapeutic target of nonalcoholic fatty liver disease[J]. Ther Clin Risk Manag, 2023, 19: 77- 96. DOI: 10.2147/TCRM.S352008. |
| [22] |
YANG XN, JIN ZQ, LIN DF, et al. FGF21 alleviates acute liver injury by inducing the SIRT1-autophagy signalling pathway[J]. J Cell Mol Med, 2022, 26( 3): 868- 879. DOI: 10.1111/jcmm.17144. |
| [23] |
HAN JX, LI SW, WANG WZ, et al. SIRT1 activator E1231 alleviates nonalcoholic fatty liver disease by regulating lipid metabolism[J]. Curr Issues Mol Biol, 2023, 45( 6): 5052- 5070. DOI: 10.3390/cimb45060321. |
| [24] |
CHEN H, TAN HB, WAN J, et al. PPAR-γ signaling in nonalcoholic fatty liver disease: Pathogenesis and therapeutic targets[J]. Pharmacol Ther, 2023, 245: 108391. DOI: 10.1016/j.pharmthera.2023.108391. |








 DownLoad:
DownLoad: