| [1] |
SUNG H, FERLAY J, SIEGEL RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J]. CA Cancer J Clin, 2021, 71( 3): 209- 249. DOI: 10.3322/caac.21660. |
| [2] |
GANESAN P, KULIK LM. Hepatocellular carcinoma: New developments[J]. Clin Liver Dis, 2023, 27( 1): 85- 102. DOI: 10.1016/j.cld.2022.08.004. |
| [3] |
COURI T, PILLAI A. Goals and targets for personalized therapy for HCC[J]. Hepatol Int, 2019, 13( 2): 125- 137. DOI: 10.1007/s12072-018-9919-1. |
| [4] |
SHIMABUKURO-VORNHAGEN A, BÖLL B, SCHELLONGOWSKI P, et al. Critical care management of chimeric antigen receptor T-cell therapy recipients[J]. CA Cancer J Clin, 2022, 72( 1): 78- 93. DOI: 10.3322/caac.21702. |
| [5] |
DRANSART B, DEHGHANI H, MOORE A. Product-safety considerations in allogeneic chimeric antigen-receptor T-cell process flows[J]. Curr Opin Biotechnol, 2022, 78: 102797. DOI: 10.1016/j.copbio.2022.102797. |
| [6] |
CARNEIRO BA, EL-DEIRY WS. Targeting apoptosis in cancer therapy[J]. Nat Rev Clin Oncol, 2020, 17( 7): 395- 417. DOI: 10.1038/s41571-020-0341-y. |
| [7] |
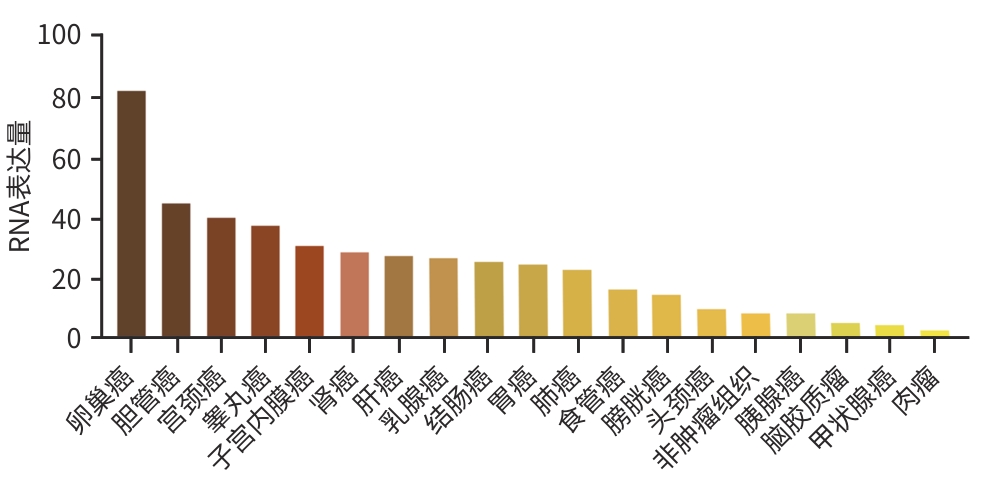
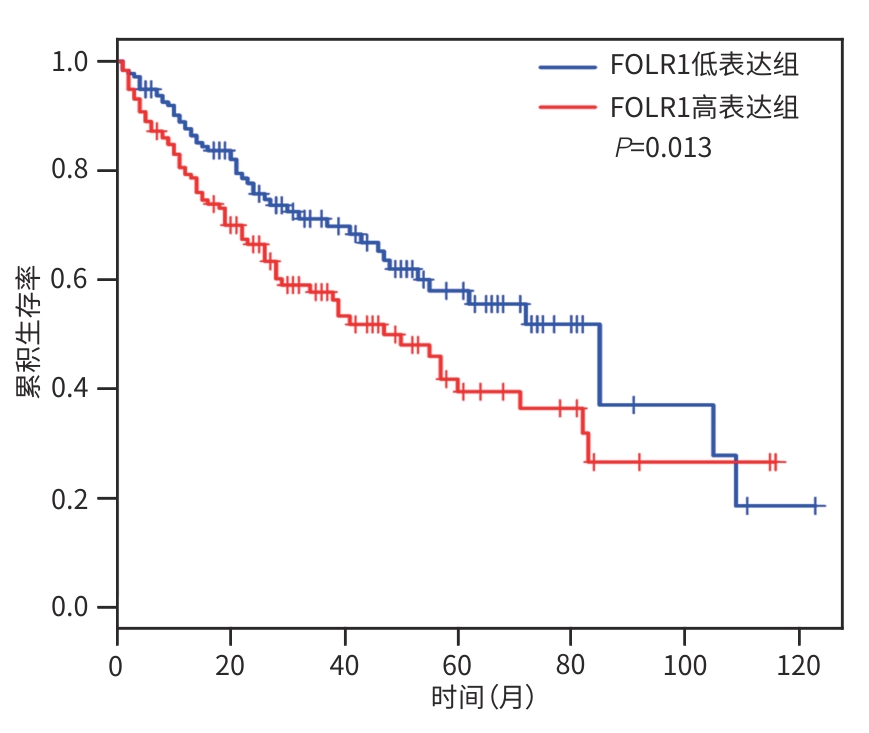
SCARANTI M, COJOCARU E, BANERJEE S, et al. Exploiting the folate receptor α in oncology[J]. Nat Rev Clin Oncol, 2020, 17( 6): 349- 359. DOI: 10.1038/s41571-020-0339-5. |
| [8] |
GILBERT L, OAKNIN A, MATULONIS UA, et al. Safety and efficacy of mirvetuximab soravtansine, a folate receptor alpha(FRα)-targeting antibody-drug conjugate(ADC), in combination with bevacizumab in patients with platinum-resistant ovarian cancer[J]. Gynecol Oncol, 2023, 170: 241- 247. DOI: 10.1016/j.ygyno.2023.01.020. |
| [9] |
YOUNG O, NGO N, LIN L, et al. Folate receptor as a biomarker and therapeutic target in solid tumors[J]. Curr Probl Cancer, 2023, 47( 1): 100917. DOI: 10.1016/j.currproblcancer.2022.100917. |
| [10] |
ZHAO YS, DENG J, RAO SF, et al. Tumor infiltrating lymphocyte(TIL) therapy for solid tumor treatment: Progressions and challenges[J]. Cancers(Basel), 2022, 14( 17): 4160. DOI: 10.3390/cancers14174160. |
| [11] |
HE JJ, XIONG XX, YANG H, et al. Defined tumor antigen-specific T cells potentiate personalized TCR-T cell therapy and prediction of immunotherapy response[J]. Cell Res, 2022, 32( 6): 530- 542. DOI: 10.1038/s41422-022-00627-9. |
| [12] |
ZHENG NB, FANG J, XUE G, et al. Induction of tumor cell autosis by myxoma virus-infected CAR-T and TCR-T cells to overcome primary and acquired resistance[J]. Cancer Cell, 2022, 40( 9): 973- 985.e7. DOI: 10.1016/j.ccell.2022.08.001. |
| [13] |
|
| [14] |
YOUNG RM, ENGEL NW, USLU U, et al. Next-generation CAR T-cell therapies[J]. Cancer Discov, 2022, 12( 7): 1625- 1633. DOI: 10.1158/2159-8290.CD-21-1683. |
| [15] |
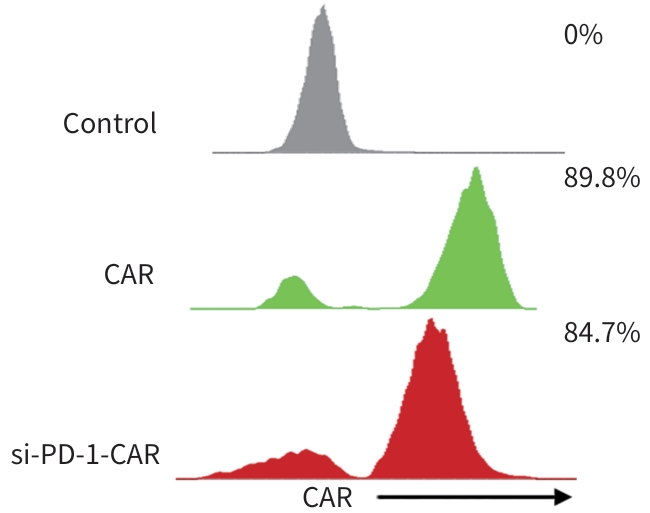
|
| [16] |
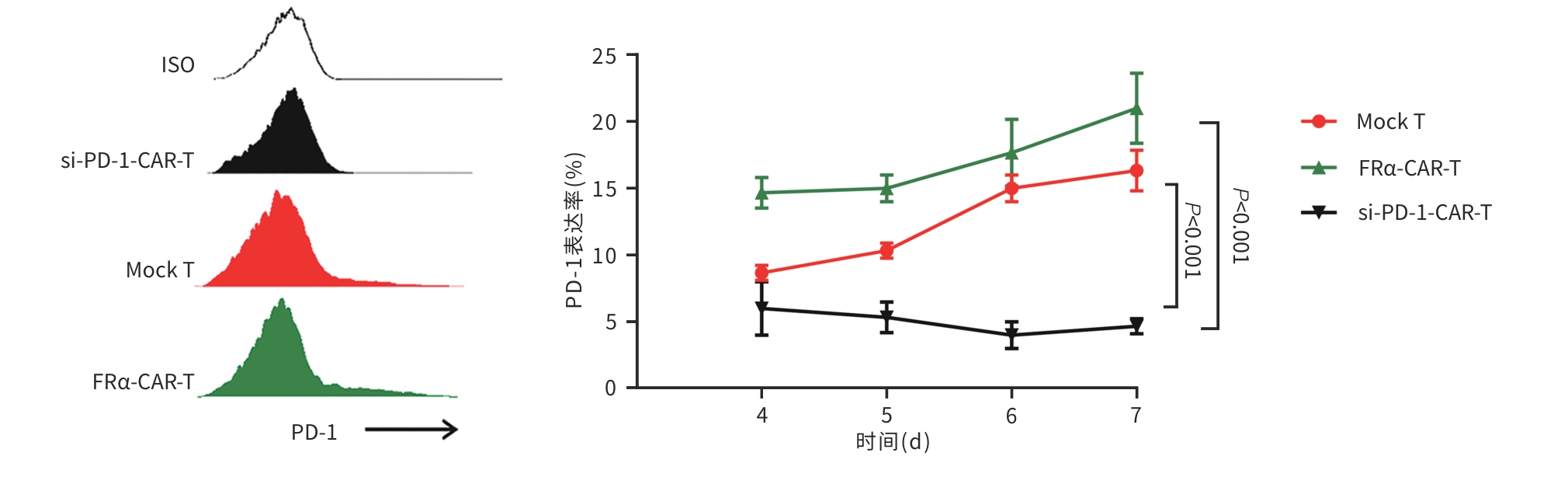
JIANG XJ, WANG J, DENG XY, et al. Role of the tumor microenvironment in PD-L1/PD-1-mediated tumor immune escape[J]. Mol Cancer, 2019, 18( 1): 10. DOI: 10.1186/s12943-018-0928-4. |
| [17] |
|
| [18] |
LEKO V, ROSENBERG SA. Identifying and targeting human tumor antigens for T cell-based immunotherapy of solid tumors[J]. Cancer Cell, 2020, 38( 4): 454- 472. DOI: 10.1016/j.ccell.2020.07.013. |
| [19] |
UPADHYAY R, BOIARSKY JA, PANTSULAIA G, et al. A critical role for fas-mediated off-target tumor killing in T-cell immunotherapy[J]. Cancer Discov, 2021, 11( 3): 599- 613. DOI: 10.1158/2159-8290.CD-20-0756. |
| [20] |
WANG HZ, YE XS, JU Y, et al. Minicircle DNA-mediated CAR T cells targeting CD44 suppressed hepatocellular carcinoma both in vitro and in vivo[J]. Onco Targets Ther, 2020, 13: 3703- 3716. DOI: 10.2147/OTT.S247836. |
| [21] |
SUN L, GAO F, GAO ZH, et al. Shed antigen-induced blocking effect on CAR-T cells targeting Glypican-3 in hepatocellular carcinoma[J]. J Immunother Cancer, 2021, 9( 4): e001875. DOI: 10.1136/jitc-2020-001875. |
| [22] |
PANG NZ, SHI JX, QIN L, et al. IL-7 and CCL19-secreting CAR-T cell therapy for tumors with positive glypican-3 or mesothelin[J]. J Hematol Oncol, 2021, 14( 1): 118. DOI: 10.1186/s13045-021-01128-9. |
| [23] |
SAITO S, KOYA Y, KAJIYAMA H, et al. Folate-appended cyclodextrin carrier targets ovarian cancer cells expressing the proton-coupled folate transporter[J]. Cancer Sci, 2020, 111( 5): 1794- 1804. DOI: 10.1111/cas.14379. |
| [24] |
CHEUNG A, OPZOOMER J, ILIEVA KM, et al. Anti-folate receptor alpha-directed antibody therapies restrict the growth of triple-negative breast cancer[J]. Clin Cancer Res, 2018, 24( 20): 5098- 5111. DOI: 10.1158/1078-0432.CCR-18-0652. |
| [25] |
LUANGWATTANANUN P, JUNKING M, SUJJITJOON J, et al. Fourth-generation chimeric antigen receptor T cells targeting folate receptor alpha antigen expressed on breast cancer cells for adoptive T cell therapy[J]. Breast Cancer Res Treat, 2021, 186( 1): 25- 36. DOI: 10.1007/s10549-020-06032-3. |
| [26] |
NAWAZ FZ, KIPREOS ET. Emerging roles for folate receptor FOLR1 in signaling and cancer[J]. Trends Endocrinol Metab, 2022, 33( 3): 159- 174. DOI: 10.1016/j.tem.2021.12.003. |
| [27] |
SHARMA A, SEOW JJW, DUTERTRE CA, et al. Onco-fetal reprogramming of endothelial cells drives immunosuppressive macrophages in hepatocellular carcinoma[J]. Cell, 2020, 183( 2): 377- 394.e21. DOI: 10.1016/j.cell.2020.08.040. |
| [28] |
ROSELLI E, BOUCHER JC, LI GB, et al. 4-1BB and optimized CD28 co-stimulation enhances function of human mono-specific and bi-specific third-generation CAR T cells[J]. J Immunother Cancer, 2021, 9( 10): e003354. DOI: 10.1136/jitc-2021-003354. |
| [29] |
MAGNANI CF, GAIPA G, LUSSANA F, et al. Sleeping Beauty-engineered CAR T cells achieve antileukemic activity without severe toxicities[J]. J Clin Invest, 2020, 130( 11): 6021- 6033. DOI: 10.1172/JCI138473. |
| [30] |
HUANG RH, LI XP, HE YD, et al. Recent advances in CAR-T cell engineering[J]. J Hematol Oncol, 2020, 13( 1): 86. DOI: 10.1186/s13045-020-00910-5. |
| [31] |
BILLINGSLEY MM, SINGH N, RAVIKUMAR P, et al. Ionizable lipid nanoparticle-mediated mRNA delivery for human CAR T cell engineering[J]. Nano Lett, 2020, 20( 3): 1578- 1589. DOI: 10.1021/acs.nanolett.9b04246. |
| [32] |
SOUNDARA RAJAN T, GUGLIANDOLO A, BRAMANTI P, et al. In vitro-transcribed mRNA chimeric antigen receptor T cell(IVT mRNA CAR T) therapy in hematologic and solid tumor management: A preclinical update[J]. Int J Mol Sci, 2020, 21( 18): 6514. DOI: 10.3390/ijms21186514. |
| [33] |
MORETTI A, PONZO M, NICOLETTE CA, et al. The past, present, and future of non-viral CAR T cells[J]. Front Immunol, 2022, 13: 867013. DOI: 10.3389/fimmu.2022.867013. |







 DownLoad:
DownLoad: