| [1] |
TREBICKA J, HERNAEZ R, SHAWCROSS DL, et al. Recent advances in the prevention and treatment of decompensated cirrhosis and acute-on-chronic liver failure(ACLF) and the role of biomarkers[J]. Gut, 2024, 73( 6): 1015- 1024. DOI: 10.1136/gutjnl-2023-330584. |
| [2] |
PIANO S, MAHMUD N, CARACENI P, et al. Mechanisms and treatment approaches for ACLF[J]. Liver Int, 2025, 45( 3): e15733. DOI: 10.1111/liv.15733. |
| [3] |
|
| [4] |
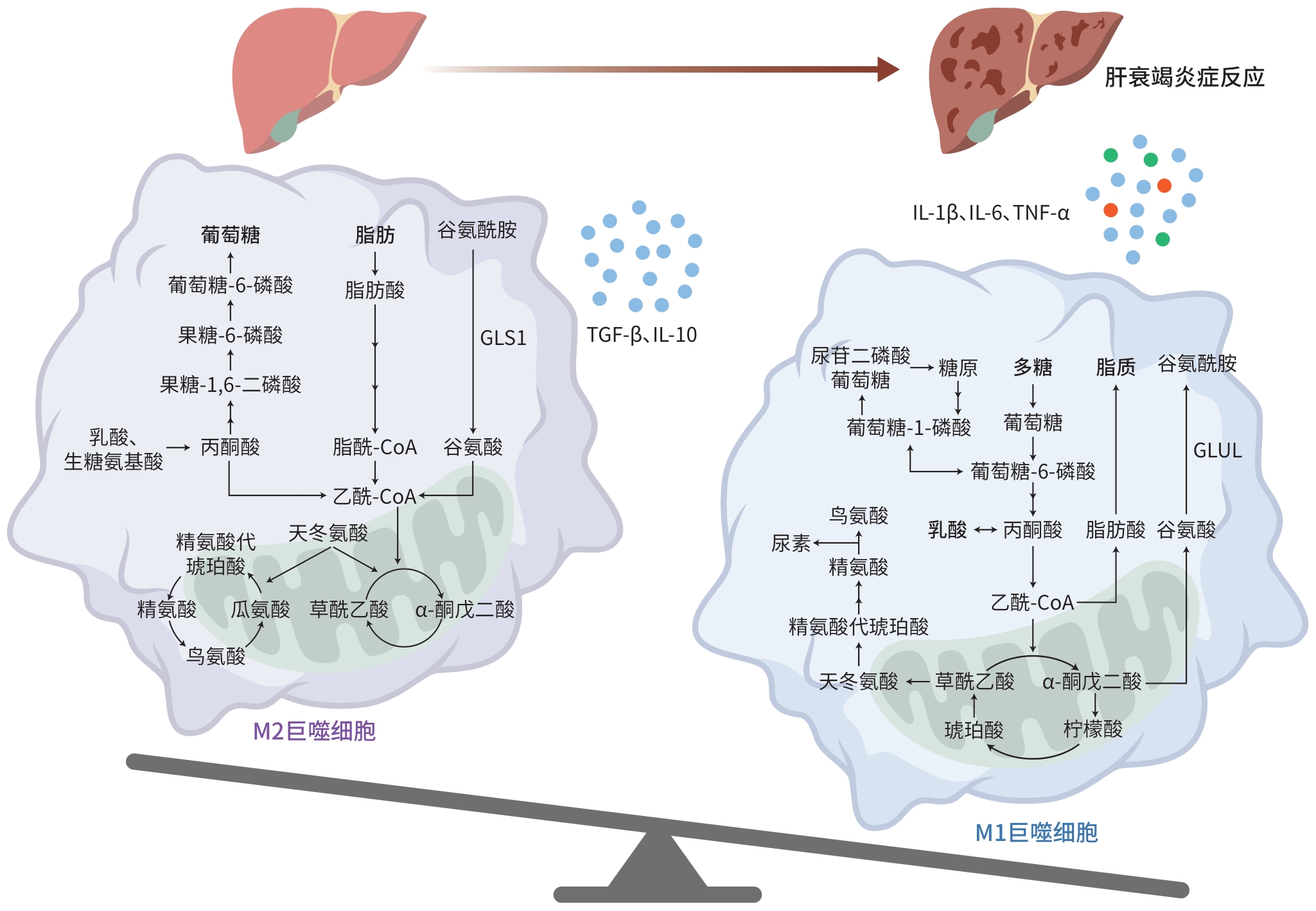
ZHANG Y, WU DS, TIAN XL, et al. From hepatitis B virus infection to acute-on-chronic liver failure: The dynamic role of hepatic macrophages[J]. Scand J Immunol, 2024, 99( 3): e13349. DOI: 10.1111/sji.13349. |
| [5] |
GAO CC, BAI J, HAN H, et al. The versatility of macrophage heterogeneity in liver fibrosis[J]. Front Immunol, 2022, 13: 968879. DOI: 10.3389/fimmu.2022.968879. |
| [6] |
XIAO Y, LU J, XU SY, et al. Metabolic differences among patients with cirrhosis using Q exactive hybrid quadrupole orbitrap mass spectrometry technology[J]. J Proteome Res, 2024, 23( 12): 5352- 5359. DOI: 10.1021/acs.jproteome.4c00437. |
| [7] |
ZHANG IW, CURTO A, LÓPEZ-VICARIO C, et al. Mitochondrial dysfunction governs immunometabolism in leukocytes of patients with acute-on-chronic liver failure[J]. J Hepatol, 2022, 76( 1): 93- 106. DOI: 10.1016/j.jhep.2021.08.009. |
| [8] |
KORF H, du PLESSIS J, van PELT J, et al. Inhibition of glutamine synthetase in monocytes from patients with acute-on-chronic liver failure resuscitates their antibacterial and inflammatory capacity[J]. Gut, 2019, 68( 10): 1872- 1883. DOI: 10.1136/gutjnl-2018-316888. |
| [9] |
ZHANG Y, TIAN XL, LI JQ, et al. Mitochondrial dysfunction affects hepatic immune and metabolic remodeling in patients with hepatitis B virus-related acute-on-chronic liver failure[J]. World J Gastroenterol, 2024, 30( 8): 881- 900. DOI: 10.3748/wjg.v30.i8.881. |
| [10] |
RAO JH, WANG H, NI M, et al. FSTL1 promotes liver fibrosis by reprogramming macrophage function through modulating the intracellular function of PKM2[J]. Gut, 2022, 71( 12): 2539- 2550. DOI: 10.1136/gutjnl-2021-325150. |
| [11] |
MA JW, WEI KK, LIU JW, et al. Glycogen metabolism regulates macrophage-mediated acute inflammatory responses[J]. Nat Commun, 2020, 11: 1769. DOI: 10.1038/s41467-020-15636-8. |
| [12] |
CUI YX, CHEN JH, ZHANG Z, et al. The role of AMPK in macrophage metabolism, function and polarisation[J]. J Transl Med, 2023, 21( 1): 892. DOI: 10.1186/s12967-023-04772-6. |
| [13] |
HAN ZY, SHEN YH, YAN YQ, et al. Metabolic reprogramming shapes post-translational modification in macrophages[J]. Mol Aspects Med, 2025, 102: 101338. DOI: 10.1016/j.mam.2025.101338. |
| [14] |
ZHANG Y, TAN WT, WANG XB, et al. Metabolic biomarkers significantly enhance the prediction of HBV-related ACLF occurrence and outcomes[J]. J Hepatol, 2023, 79( 5): 1159- 1171. DOI: 10.1016/j.jhep.2023.07.011. |
| [15] |
LIU PS, WANG HP, LI XY, et al. α-ketoglutarate orchestrates macrophage activation through metabolic and epigenetic reprogramming[J]. Nat Immunol, 2017, 18( 9): 985- 994. DOI: 10.1038/ni.3796. |
| [16] |
YU ZJ, LI JJ, REN ZG, et al. Switching from fatty acid oxidation to glycolysis improves the outcome of acute-on-chronic liver failure[J]. Adv Sci, 2020, 7( 7): 1902996. DOI: 10.1002/advs.201902996. |
| [17] |
BOSMANS LA, van TIEL CM, AARTS SABM, et al. Myeloid CD40 deficiency reduces atherosclerosis by impairing macrophages’ transition into a pro-inflammatory state[J]. Cardiovasc Res, 2023, 119( 5): 1146- 1160. DOI: 10.1093/cvr/cvac084. |
| [18] |
LIU PS, CHEN YT, LI XY, et al. CD40 signal rewires fatty acid and glutamine metabolism for stimulating macrophage anti-tumorigenic functions[J]. Nat Immunol, 2023, 24( 3): 452- 462. DOI: 10.1038/s41590-023-01430-3. |
| [19] |
ZHANG QY, SONG QL, LIU S, et al. Integrated transcriptomic and metabolomic analysis reveals the metabolic programming of GM-CSF-and M-CSF-differentiated mouse macrophages[J]. Front Immunol, 2023, 14: 1230772. DOI: 10.3389/fimmu.2023.1230772. |
| [20] |
MAO YX, SHI D, LI G, et al. Citrulline depletion by ASS1 is required for proinflammatory macrophage activation and immune responses[J]. Mol Cell, 2022, 82( 3): 527- 541. e 7. DOI: 10.1016/j.molcel.2021.12.006. |
| [21] |
YAN JW, HORNG T. Lipid metabolism in regulation of macrophage functions[J]. Trends Cell Biol, 2020, 30( 12): 979- 989. DOI: 10.1016/j.tcb.2020.09.006. |
| [22] |
YANG Y, NI M, ZONG RB, et al. Targeting Notch1-YAP circuit reprograms macrophage polarization and alleviates acute liver injury in mice[J]. Cell Mol Gastroenterol Hepatol, 2023, 15( 5): 1085- 1104. DOI: 10.1016/j.jcmgh.2023.01.002. |
| [23] |
SÁNCHEZ-RODRÍGUEZ MB, TÉLLEZ É, CASULLERAS M, et al. Reduced plasma extracellular vesicle CD5L content in patients with acute-on-chronic liver failure: Interplay with specialized pro-resolving lipid mediators[J]. Front Immunol, 2022, 13: 842996. DOI: 10.3389/fimmu.2022.842996. |
| [24] |
PENG B, LI H, LIU K, et al. Intrahepatic macrophage reprogramming associated with lipid metabolism in hepatitis B virus-related acute-on-chronic liver failure[J]. J Transl Med, 2023, 21( 1): 419. DOI: 10.1186/s12967-023-04294-1. |
| [25] |
MAHESHWARI D, KUMAR D, JAGDISH RK, et al. Bioenergetic failure drives functional exhaustion of monocytes in acute-on-chronic liver failure[J]. Front Immunol, 2022, 13: 856587. DOI: 10.3389/fimmu.2022.856587. |
| [26] |
MAIWALL R, BAJPAI M, CHOUDHURY AK, et al. Therapeutic plasma-exchange improves systemic inflammation and survival in acute-on-chronic liver failure: A propensity-score matched study from AARC[J]. Liver Int, 2021, 41( 5): 1083- 1096. DOI: 10.1111/liv.14806. |
| [27] |
LI ZH, WANG JY, LI XL, et al. Mesenchymal stem cell-regulated miRNA-mRNA landscape in acute-on-chronic liver failure[J]. Genomics, 2023, 115( 6): 110737. DOI: 10.1016/j.ygeno.2023.110737. |
| [28] |
GAO YH, MI NN, WU WX, et al. Transfer of inflammatory mitochondria via extracellular vesicles from M1 macrophages induces ferroptosis of pancreatic beta cells in acute pancreatitis[J]. J Extracell Vesicles, 2024, 13( 2): e12410. DOI: 10.1002/jev2.12410. |
| [29] |
XUE JH, CHEN F, WANG J, et al. Emodin protects against concanavalin A-induced hepatitis in mice through inhibiting activation of the p38 MAPK-NF-κB signaling pathway[J]. Cell Physiol Biochem, 2015, 35( 4): 1557- 1570. DOI: 10.1159/000373971. |






 DownLoad:
DownLoad: