| [1] |
LI MY, ZHANG W. Research progress of chronic liver disease complicated with depression and anxiety in traditional Chinese and western medicine[J]. Chin J Integr Tradit West Med Liver Dis, 2025, 35( 1): 109- 114. DOI: 10.3969/j.issn.1005-0264.2025.001.026. |
| [2] |
YANG ZH, WANG JH, WANG L, et al. Research progress of the regulation of orphan nuclear receptors on chronic liver diseases[J]. Acta Physiol Sin, 2023, 75( 4): 555- 568. DOI: 10.13294/j.aps.2023.0047. |
| [3] |
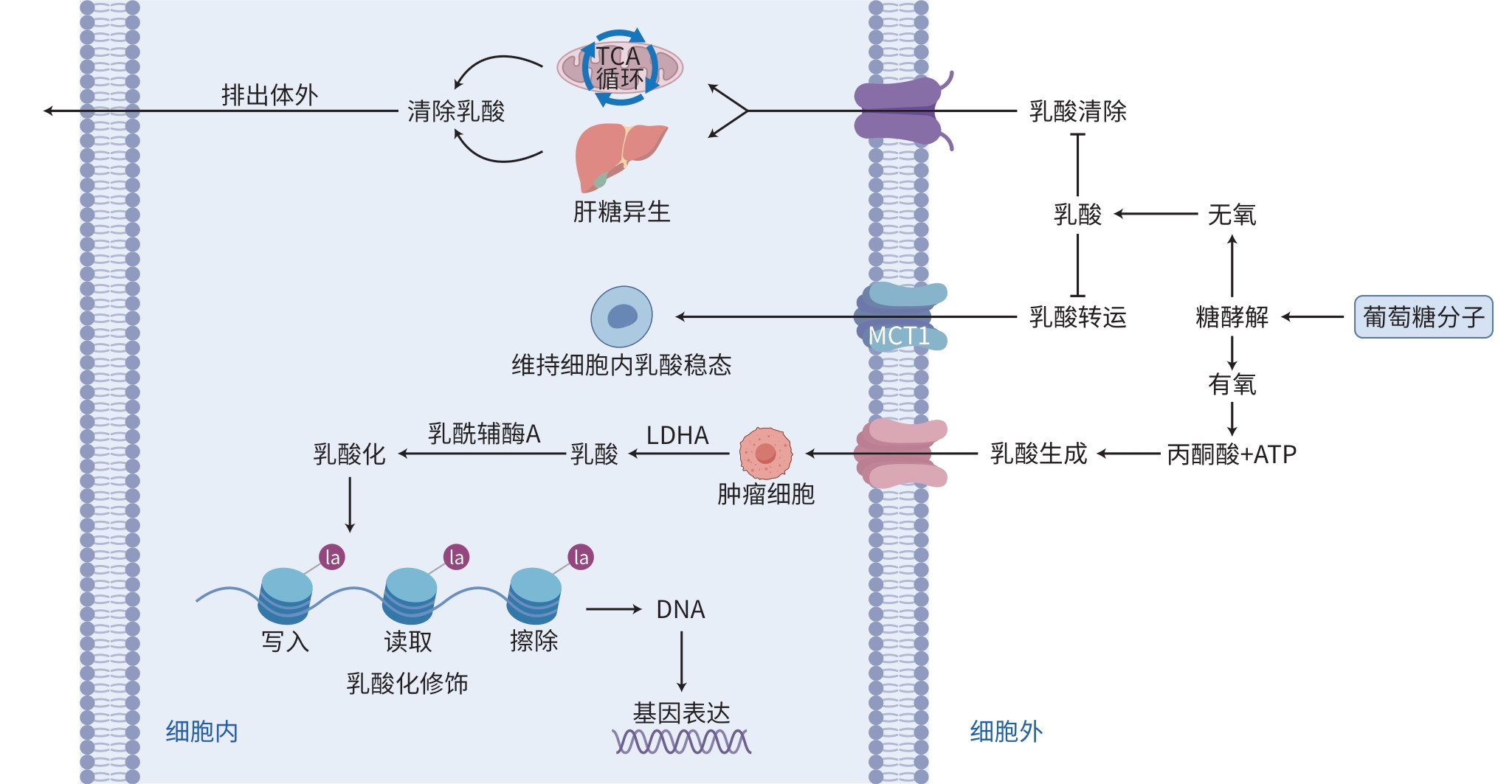
ZHANG D, TANG ZY, HUANG H, et al. Metabolic regulation of gene expression by histone lactylation[J]. Nature, 2019, 574( 7779): 575- 580. DOI: 10.1038/s41586-019-1678-1. |
| [4] |
SHI J, LI HJ, ZHAO MY, et al. Progress in the study of anti-hepatic fibrosis of phenylpropanoid constituents of traditional Chinese medicines[J]. Strait Pharm J, 2024, 36( 10): 1- 5. DOI: 10.3969/j.issn.1006-3765.2024.10.001. |
| [5] |
ZHANG TT, WANG C, SONG AN, et al. Water extract of earthworms mitigates mouse liver fibrosis by potentiating hepatic LKB1/Nrf2 axis to inhibit HSC activation and hepatocyte death[J]. J Ethnopharmacol, 2024, 321: 117495. DOI: 10.1016/j.jep.2023.117495. |
| [6] |
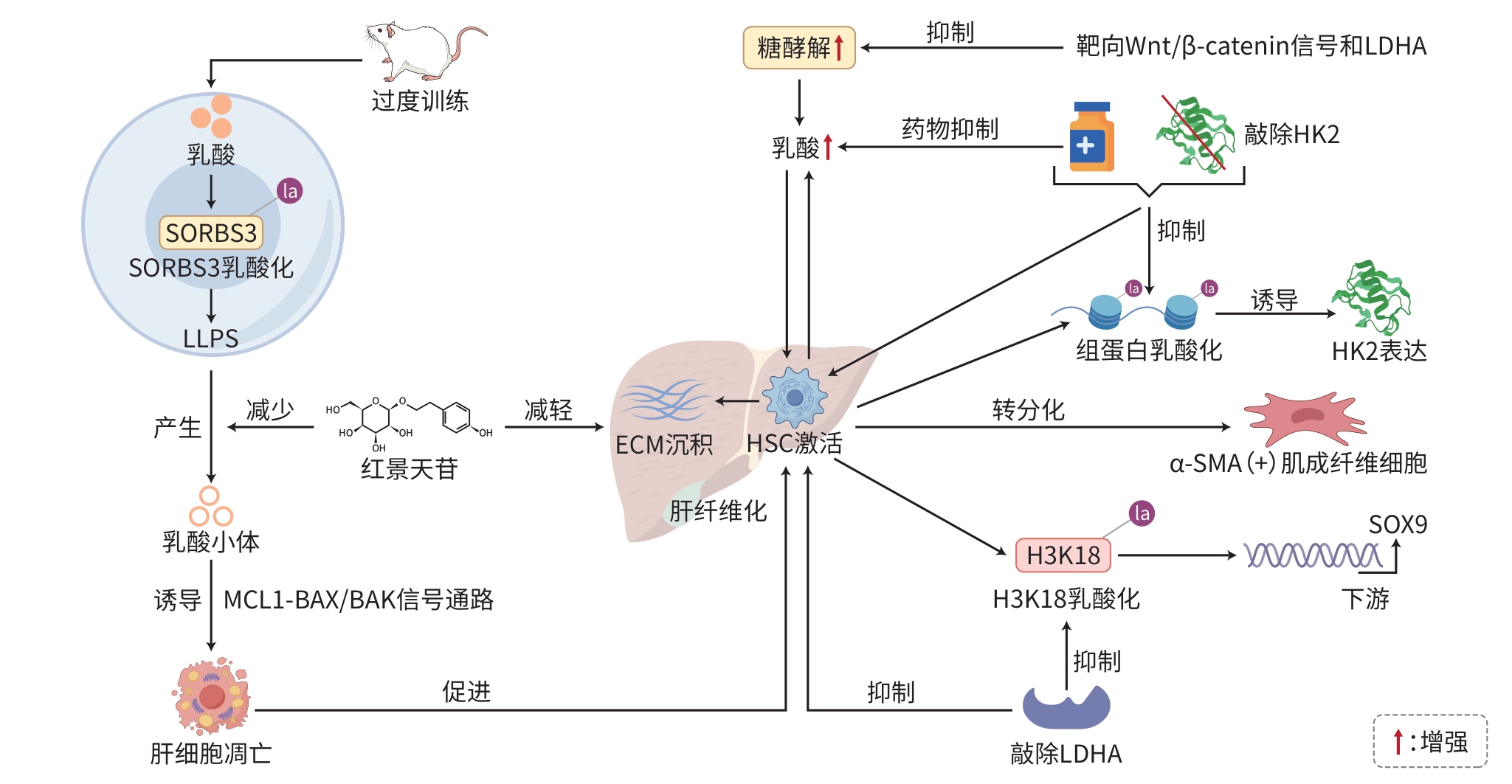
WANG FX, CHEN L, KONG DS, et al. Canonical Wnt signaling promotes HSC glycolysis and liver fibrosis through an LDH-A/HIF-1α transcriptional complex[J]. Hepatology, 2024, 79( 3): 606- 623. DOI: 10.1097/HEP.0000000000000569. |
| [7] |
MA YJ, YU HF. The roles of protein lactylation in liver diseases[J]. Chem Life, 2024, 44( 12): 2334- 2341. DOI: 10.13488/j.smhx.20240457. |
| [8] |
RHO H, TERRY AR, CHRONIS C, et al. Hexokinase 2-mediated gene expression via histone lactylation is required for hepatic stellate cell activation and liver fibrosis[J]. Cell Metab, 2023, 35( 8): 1406- 1423. e 8. DOI: 10.1016/j.cmet.2023.06.013. |
| [9] |
WU SJ, LI JH, ZHAN YF. H3K18 lactylation accelerates liver fibrosis progression through facilitating SOX9 transcription[J]. Exp Cell Res, 2024, 440( 2): 114135. DOI: 10.1016/j.yexcr.2024.114135. |
| [10] |
LIU Y, ZHOU R, GUO YF, et al. Muscle-derived small extracellular vesicles induce liver fibrosis during overtraining[J]. Cell Metab, 2025, 37( 4): 824- 841. e 8. DOI: 10.1016/j.cmet.2024.12.005. |
| [11] |
HUANG WQ, WEN HY, LI JX, et al. Viral hepatitis: A review of global prevalence and research progress toward elimination[J]. Chin J Public Health, 2024, 40( 11): 1413- 1416. DOI: 10.11847/zgggws11-44938.
|
| [12] |
WANG Y. Public health management strategies: A pathway to eliminating viral hepatitis threats[J]. J Clin Hepatol, 2025, 41( 2): 201- 204. DOI: 10.12449/JCH250201. |
| [13] |
YANG ZJ, YAN C, MA JQ, et al. Lactylome analysis suggests lactylation-dependent mechanisms of metabolic adaptation in hepatocellular carcinoma[J]. Nat Metab, 2023, 5( 1): 61- 79. DOI: 10.1038/s42255-022-00710-w. |
| [14] |
HENRY L, PAIK J, YOUNOSSI ZM. Review article: The epidemiologic burden of non-alcoholic fatty liver disease across the world[J]. Aliment Pharmacol Ther, 2022, 56( 6): 942- 956. DOI: 10.1111/apt.17158. |
| [15] |
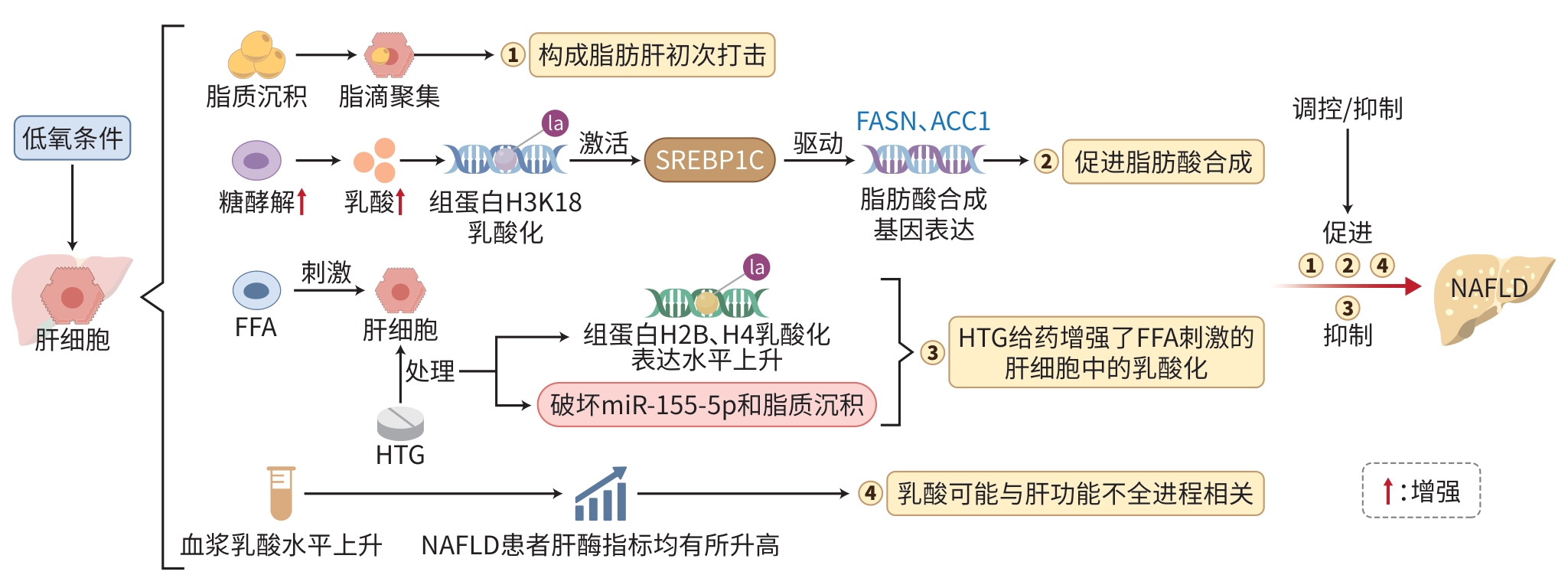
CHENG WH. Effect of hypoxia on lipid metabolism of L02 cells and its possible mechanism[D]. Chongqing: Chongqing Medical University, 2012.
程文会. 低氧对L02细胞脂肪代谢的影响及其可能机制[D]. 重庆: 重庆医科大学, 2012.
|
| [16] |
GAO RX, LI Y, XU ZM, et al. Mitochondrial pyruvate carrier 1 regulates fatty acid synthase lactylation and mediates treatment of nonalcoholic fatty liver disease[J]. Hepatology, 2023, 78( 6): 1800- 1815. DOI: 10.1097/HEP.0000000000000279. |
| [17] |
YIN XJ, LI M, WANG YZ, et al. Herbal medicine formula Huazhuo Tiaozhi granule ameliorates dyslipidaemia via regulating histone lactylation and miR-155-5p biogenesis[J]. Clin Epigenetics, 2023, 15( 1): 175. DOI: 10.1186/s13148-023-01573-y. |
| [18] |
ZHANG SY. Correlation study on the relationship between plasma lactate levels and the severity of fatty liver and related clinical indicators in NAFLD patients[D]. Hangzhou: Hangzhou Normal University, 2023.
章思懿. NAFLD患者血浆乳酸水平与脂肪肝严重程度及相关临床指标的相关性研究[D]. 杭州: 杭州师范大学, 2023.
|
| [19] |
SHENG XD. Study on the mechanism of action of tea water extract in treating alcohol-related liver injury[D]. Hefei: Anhui Medical University, 2024.
盛啸东. 茶叶水提取物治疗酒精性相关性肝损伤的作用机制研究[D]. 合肥: 安徽医科大学, 2024.
|
| [20] |
JIANG QL. Shanghai Institute of Nutrition and Health, CAS, Elucidates Mechanism of Ethyl Lactate in Ameliorating Liver Injury and Alcohol-Associated Liver Disease[N]. Science Times, 2024-12-16(3). DOI: 10.28514/n.cnki.nkxsb.2024.002987. |
| [21] |
JIANG Y, WEI S, SHEN SM, et al. Ethyl lactate ameliorates hepatic steatosis and acute-on-chronic liver injury in alcohol-associated liver disease by inducing fibroblast growth factor 21[J]. Adv Sci(Weinh), 2025, 12( 5): e2409516. DOI: 10.1002/advs.202409516. |
| [22] |
JIANG YC, ZHANG T, KUSUMANCHI P, et al. Alcohol metabolizing enzymes, microsomal ethanol oxidizing system, cytochrome P450 2E1, catalase, and aldehyde dehydrogenase in alcohol-associated liver disease[J]. Biomedicines, 2020, 8( 3): 50. DOI: 10.3390/biomedicines8030050. |
| [23] |
LLOVET JM, KELLEY RK, VILLANUEVA A, et al. Hepatocellular carcinoma[J]. Nat Rev Dis Primers, 2021, 7( 1): 6. DOI: 10.1038/s41572-020-00240-3. |
| [24] |
ZHU CF, WANG XD. Value of local treatment combined with systemic therapy in conversion therapy for hepatocellular carcinoma[J]. J Clin Hepatol, 2024, 40( 9): 1732- 1737. DOI: 10.12449/JCH240903.
朱超凡, 王晓东. 局部治疗联合系统治疗在肝细胞癌转化治疗中的价值[J]. 临床肝胆病杂志, 2024, 40( 9): 1732- 1737. DOI: 10.12449/JCH24-0903. |
| [25] |
YE ZJ. The impact of LSD1 lactic acid modification on the development of liver cancer and the mechanism of TIGD1 on liver cancer growth[D]. Guangzhou: South China University of Technology, 2023.
叶子坚. LSD1乳酸化修饰对肝癌发生发展的影响和TIGD1对肝癌生长的机制研究[D]. 广州: 华南理工大学, 2023.
|
| [26] |
JIN J, BAI L, WANG DY, et al. SIRT3-dependent delactylation of cyclin E2 prevents hepatocellular carcinoma growth[J]. EMBO Rep, 2023, 24( 5): e56052. DOI: 10.15252/embr.202256052. |
| [27] |
HONG H, HAN HX, WANG L, et al. ABCF1-K430-Lactylation promotes HCC malignant progression via transcriptional activation of HIF1 signaling pathway[J]. Cell Death Differ, 2025, 32( 4): 613- 631. DOI: 10.1038/s41418-024-01436-w. |
| [28] |
PAN LH, FENG F, WU JQ, et al. Demethylzeylasteral targets lactate by inhibiting histone lactylation to suppress the tumorigenicity of liver cancer stem cells[J]. Pharmacol Res, 2022, 181: 106270. DOI: 10.1016/j.phrs.2022.106270. |
| [29] |
XU HY, LI LQ, WANG SS, et al. Royal jelly acid suppresses hepatocellular carcinoma tumorigenicity by inhibiting H3 histone lactylation at H3K9la and H3K14la sites[J]. Phytomedicine, 2023, 118: 154940. DOI: 10.1016/j.phymed.2023.154940. |
| [30] |
PERALTA RM, XIE BX, LONTOS K, et al. Dysfunction of exhausted T cells is enforced by MCT11-mediated lactate metabolism[J]. Nat Immunol, 2024, 25( 12): 2297- 2307. DOI: 10.1038/s41590-024-01999-3. |
| [31] |
HAN SL, BAO XY, ZOU YF, et al. D-lactate modulates M2 tumor-associated macrophages and remodels immunosuppressive tumor microenvironment for hepatocellular carcinoma[J]. Sci Adv, 2023, 9( 29): eadg2697. DOI: 10.1126/sciadv.adg2697. |
| [32] |
FENG F, WU JQ, CHI QJ, et al. Lactylome analysis unveils lactylation-dependent mechanisms of stemness remodeling in the liver cancer stem cells[J]. Adv Sci, 2024, 11( 38): 2405975. DOI: 10.1002/advs.202405975. |
| [33] |
WANG HY, XU M, ZHANG T, et al. PYCR1 promotes liver cancer cell growth and metastasis by regulating IRS1 expression through lactylation modification[J]. Clin Transl Med, 2024, 14( 10): e70045. DOI: 10.1002/ctm2.70045. |
| [34] |
DONG RY, FEI Y, HE YR, et al. Lactylation-driven HECTD2 limits the response of hepatocellular carcinoma to lenvatinib[J]. Adv Sci(Weinh), 2025, 12( 15): e2412559. DOI: 10.1002/advs.202412559. |
| [35] |
CHEN J, HUANG ZY, CHEN Y, et al. Lactate and lactylation in cancer[J]. Sig Transduct Target Ther, 2025, 10( 1): 38. DOI: 10.1038/s41392-024-02082-x. |
| [36] |
HALFORD S, VEAL GJ, WEDGE SR, et al. A phase I dose-escalation study of AZD3965, an oral monocarboxylate transporter 1 inhibitor, in patients with advanced cancer[J]. Clin Cancer Res, 2023, 29( 8): 1429- 1439. DOI: 10.1158/1078-0432.CCR-22-2263. |
| [37] |
JIANG PR, NING WS, SHI YS, et al. FSL-Kla: A few-shot learning-based multi-feature hybrid system for lactylation site prediction[J]. Comput Struct Biotechnol J, 2021, 19: 4497- 4509. DOI: 10.1016/j.csbj.2021.08.013. |






 DownLoad:
DownLoad: