| [1] |
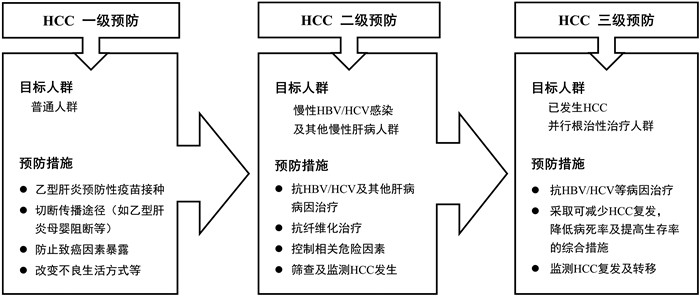
Prevention of Infection Related Cancer (PIRCA) Group, Specialized Committee of Cancer Prevention and Control, Chinese Preventive Medicine Association; Non-communicable & Chronic Disease Control and Prevention Society, Chinese Preventive Medicine Association; Health Communication Society, Chinese Preventive Medicine Association. Strategies of primary prevention of liver cancer in China: Expert Consensus (2018)[J]. J Clin Hepatol, 2018, 34(10): 2090-2097. (in Chinese) DOI: 10.3969/j.issn.1001-5256.2018.10.008 |
| [2] |
Bureau of Medical Administration, National Health Commission of the People's Republic of China. Guidelines for diagnosis and treatment of primary liver cancer in China (2019 edition)[J]. J Clin Hepatol, 2020, 36(2): 277-292. (in Chinese) DOI: 10.3969/j.issn.1001-5256.2020.05.009 |
| [3] |
Chinese society of clinical oncology. Guidelines of Chinese society of clinical onc ology(CSCO) Hepatocellular carcinoma[M]. Beijing: People's Health Publishing House, 2018: 1-98. (in Chinese)
中国临床肿瘤学会. CSCO原发性肝癌诊疗指南(2018. V1)[M]. 北京: 人民卫生出版社, 2018: 1-98.
|
| [4] |
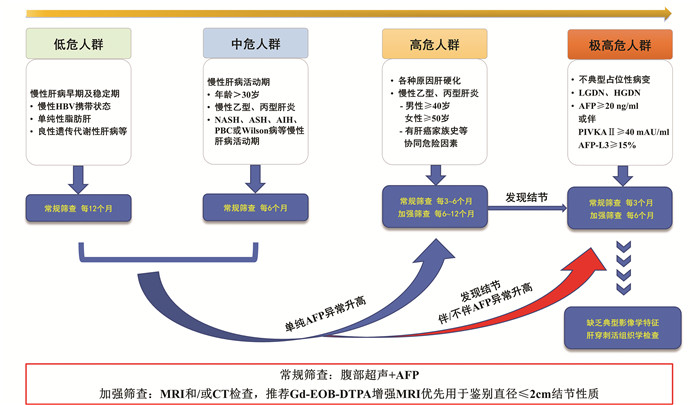
Professional Committee for Prevention and Control of Hepatobiliary and Pancreatic Diseases of Chinese Preventive Medicine Association; Professional Committee for Hepatology, Chinese Research Hospital Association; Chinese Society of Hepatology, Chinese Medical Association, et al. Guideline for stratified screening and surveillance of primary liver cancer (2020 edition)[J]. J Clin Hepatol, 2021, 37(2): 286-295. (in Chinese) DOI: 10.3969/j.issn.1001-5256.2021.02.009 |
| [5] |
|
| [6] |
PARK JW, CHEN M, COLOMBO M, et al. Global patterns of hepatocellular carcinoma management from diagnosis to death: The BRIDGE Study[J]. Liver Int, 2015, 35(9): 2155-2166. DOI: 10.1111/liv.12818 |
| [7] |
MU XM, WANG W, JIANG YY, et al. Patterns of comorbidity in hepatocellular carcinoma: A network perspective[J]. Int J Environ Res Public Health, 2020, 17(9): 3108. DOI: 10.3390/ijerph17093108 |
| [8] |
MARRERO JA, KULIK LM, SIRLIN CB, et al. Diagnosis, staging, and management of hepatocellular carcinoma: 2018 practice guidance by the American Association for the Study of Liver Diseases[J]. Hepatology, 2018, 68(2): 723-750. DOI: 10.1002/hep.29913 |
| [9] |
ALLEMANI C, MATSUDA T, di CARLO V, et al. Global surveillance of trends in cancer survival 2000-14 (CONCORD-3): Analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries[J]. Lancet, 2018, 391(10125): 1023-1075. DOI: 10.1016/S0140-6736(17)33326-3 |
| [10] |
WANG M, WANG Y, FENG X, et al. Contribution of hepatitis B virus and hepatitis C virus to liver cancer in China north areas: Experience of the Chinese National Cancer Center[J]. Int J Infect Dis, 2017, 65: 15-21. DOI: 10.1016/j.ijid.2017.09.003 |
| [11] |
Global Burden of Disease Liver Cancer Collaboration, AKINYEMIJU T, ABERA S, et al. The burden of primary liver cancer and underlying etiologies from 1990 to 2015 at the global, regional, and national level: Results from the Global Burden of Disease Study 2015[J]. JAMA Oncol, 2017, 3(12): 1683-1691. DOI: 10.1001/jamaoncol.2017.3055 |
| [12] |
|
| [13] |
|
| [14] |
LOK AS, MCMAHON BJ, BROWN RS Jr, et al. Antiviral therapy for chronic hepatitis B viral infection in adults: A systematic review and meta-analysis[J]. Hepatology, 2016, 63(1): 284-306. DOI: 10.1002/hep.28280 |
| [15] |
GANNE-CARRIÉ N, NAHON P. Hepatocellular carcinoma in the setting of alcohol-related liver disease[J]. J Hepatol, 2019, 70(2): 284-293. DOI: 10.1016/j.jhep.2018.10.008 |
| [16] |
GANNE-CARRIÉ N, CHAFFAUT C, BOURCIER V, et al. Estimate of hepatocellular carcinoma incidence in patients with alcoholic cirrhosis[J]. J Hepatol, 2018, 69(6): 1274-1283. DOI: 10.1016/j.jhep.2018.07.022 |
| [17] |
WHITE DL, KANWAL F, EL-SERAG HB. Association between nonalcoholic fatty liver disease and risk for hepatocellular cancer, based on systematic review[J]. Clin Gastroenterol Hepatol, 2012, 10(12): 1342-1359. e2. DOI: 10.1016/j.cgh.2012.10.001 |
| [18] |
PARK SZ, NAGORNEY DM, CZAJA AJ. Hepatocellular carcinoma in autoimmune hepatitis[J]. Dig Dis Sci, 2000, 45(10): 1944-1948. DOI: 10.1023/A:1005638500236 |
| [19] |
van MEER S, de MAN RA, van den BERG AP, et al. No increased risk of hepatocellular carcinoma in cirrhosis due to Wilson disease during long-term follow-up[J]. J Gastroenterol Hepatol, 2015, 30(3): 535-539. DOI: 10.1111/jgh.12716 |
| [20] |
SHARMA SA, KOWGIER M, HANSEN BE, et al. Toronto HCC risk index: A validated scoring system to predict 10-year risk of HCC in patients with cirrhosis[J]. J Hepatol, 2017.[Online ahead of print]
|
| [21] |
SHI J, ZHU L, LIU S, et al. A meta-analysis of case-control studies on the combined effect of hepatitis B and C virus infections in causing hepatocellular carcinoma in China[J]. Br J Cancer, 2005, 92(3): 607-612. DOI: 10.1038/sj.bjc.6602333 |
| [22] |
CHEN CJ, YANG HI, ILOEJE UH, et al. Hepatitis B virus DNA levels and outcomes in chronic hepatitis B[J]. Hepatology, 2009, 49(5 Suppl): S72-S84. DOI: 10.1002/hep.22884/abstract |
| [23] |
TSENG TC, LIU CJ, HSU CY, et al. High level of hepatitis B core-related antigen associated with increased risk of hepatocellular carcinoma in patients with chronic HBV infection of intermediate viral load[J]. Gastroenterology, 2019, 157(6): 1518-1529. e3. DOI: 10.1053/j.gastro.2019.08.028 |
| [24] |
CHEN CJ, YANG HI, SU J, et al. Risk of hepatocellular carcinoma across a biological gradient of serum hepatitis B virus DNA level[J]. JAMA, 2006, 295(1): 65-73. DOI: 10.1001/jama.295.1.65 |
| [25] |
YU MW, CHANG HC, LIAW YF, et al. Familial risk of hepatocellular carcinoma among chronic hepatitis B carriers and their relatives[J]. J Natl Cancer Inst, 2000, 92(14): 1159-1164. DOI: 10.1093/jnci/92.14.1159 |
| [26] |
YANG HI, LU SN, LIAW YF, et al. Hepatitis B e antigen and the risk of hepatocellular carcinoma[J]. N Engl J Med, 2002, 347(3): 168-174. DOI: 10.1056/NEJMoa013215 |
| [27] |
|
| [28] |
FATTOVICH G, BORTOLOTTI F, DONATO F. Natural history of chronic hepatitis B: Special emphasis on disease progression and prognostic factors[J]. J Hepatol, 2008, 48(2): 335-352. DOI: 10.1016/j.jhep.2007.11.011 |
| [29] |
XIAO J, WANG F, WONG NK, et al. Global liver disease burdens and research trends: Analysis from a Chinese perspective[J]. J Hepatol, 2019, 71(1): 212-221. DOI: 10.1016/j.jhep.2019.03.004 |
| [30] |
SHERMAN M. Hepatocellular carcinoma: Epidemiology, risk factors, and screening[J]. Semin Liver Dis, 2005, 25(2): 143-154. DOI: 10.1055/s-2005-871194 |
| [31] |
YOSHIDA H, SHIRATORI Y, MORIYAMA M, et al. Interferon therapy reduces the risk for hepatocellular carcinoma: National surveillance program of cirrhotic and noncirrhotic patients with chronic hepatitis C in Japan. IHIT Study Group. Inhibition of hepatocarcinogenesis by interferon therapy[J]. Ann Intern Med, 1999, 131(3): 174-181. DOI: 10.7326/0003-4819-131-3-199908030-00003 |
| [32] |
RAIMONDI S, BRUNO S, MONDELLI MU, et al. Hepatitis C virus genotype 1b as a risk factor for hepatocellular carcinoma development: A meta-analysis[J]. J Hepatol, 2009, 50(6): 1142-1154. DOI: 10.1016/j.jhep.2009.01.019 |
| [33] |
|
| [34] |
SEITZ HK, BATALLER R, CORTEZ-PINTO H, et al. Alcoholic liver disease[J]. Nat Rev Dis Primers, 2018, 4(1): 16. DOI: 10.1038/s41572-018-0014-7 |
| [35] |
HECKLEY GA, JARL J, ASAMOAH BO, et al. How the risk of liver cancer changes after alcohol cessation: A review and meta-analysis of the current literature[J]. BMC Cancer, 2011, 11: 446. DOI: 10.1186/1471-2407-11-446 |
| [36] |
CORRAO G, BAGNARDI V, ZAMBON A, et al. A meta-analysis of alcohol consumption and the risk of 15 diseases[J]. Prev Med, 2004, 38(5): 613-619. DOI: 10.1016/j.ypmed.2003.11.027 |
| [37] |
HASSAN MM, HWANG LY, HATTEN CJ, et al. Risk factors for hepatocellular carcinoma: Synergism of alcohol with viral hepatitis and diabetes mellitus[J]. Hepatology, 2002, 36(5): 1206-1213. DOI: 10.1053/jhep.2002.36780 |
| [38] |
ESLAM M, SARIN SK, WONG VW, et al. The Asian Pacific Association for the Study of the Liver clinical practice guidelines for the diagnosis and management of metabolic associated fatty liver disease[J]. Hepatol Int, 2020, 14(6): 889-919. DOI: 10.1007/s12072-020-10094-2 |
| [39] |
YOUNOSSI ZM, KOENIG AB, ABDELATIF D, et al. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes[J]. Hepatology, 2016, 64(1): 73-84. DOI: 10.1002/hep.28431 |
| [40] |
DYSON J, JAQUES B, CHATTOPADYHAY D, et al. Hepatocellular cancer: The impact of obesity, type 2 diabetes and a multidisciplinary team[J]. J Hepatol, 2014, 60(1): 110-117. DOI: 10.1016/j.jhep.2013.08.011 |
| [41] |
CHEN CL, YANG HI, YANG WS, et al. Metabolic factors and risk of hepatocellular carcinoma by chronic hepatitis B/C infection: A follow-up study in Taiwan[J]. Gastroenterology, 2008, 135(1): 111-121. DOI: 10.1053/j.gastro.2008.03.073 |
| [42] |
LIU Y, CHANG CC, MARSH GM, et al. Population attributable risk of aflatoxin-related liver cancer: Systematic review and meta-analysis[J]. Eur J Cancer, 2012, 48(14): 2125-2136. DOI: 10.1016/j.ejca.2012.02.009 |
| [43] |
KOBAYASHI M, IKEDA K, HOSAKA T, et al. Dysplastic nodules frequently develop into hepatocellular carcinoma in patients with chronic viral hepatitis and cirrhosis[J]. Cancer, 2006, 106(3): 636-647. DOI: 10.1002/cncr.21607 |
| [44] |
TOYODA H, KUMADA T, OSAKI Y, et al. Staging hepatocellular carcinoma by a novel scoring system (BALAD score) based on serum markers[J]. Clin Gastroenterol Hepatol, 2006, 4(12): 1528-1536. DOI: 10.1016/j.cgh.2006.09.021 |
| [45] |
YANG HI, YUEN MF, CHAN HL, et al. Risk estimation for hepatocellular carcinoma in chronic hepatitis B (REACH-B): Development and validation of a predictive score[J]. Lancet Oncol, 2011, 12(6): 568-574. DOI: 10.1016/S1470-2045(11)70077-8 |
| [46] |
FAN C, LI M, GAN Y, et al. A simple AGED score for risk classification of primary liver cancer: Development and validation with long-term prospective HBsAg-positive cohorts in Qidong, China[J]. Gut, 2019, 68(5): 948-949. DOI: 10.1136/gutjnl-2018-316525 |
| [47] |
PAPATHEODORIDIS G, DALEKOS G, SYPSA V, et al. PAGE-B predicts the risk of developing hepatocellular carcinoma in Caucasians with chronic hepatitis B on 5-year antiviral therapy[J]. J Hepatol, 2016, 64(4): 800-806. DOI: 10.1016/j.jhep.2015.11.035 |
| [48] |
PAPATHEODORIDIS GV, SYPSA V, DALEKOS GN, et al. Hepatocellular carcinoma prediction beyond year 5 of oral therapy in a large cohort of Caucasian patients with chronic hepatitis B[J]. J Hepatol, 2020, 72(6): 1088-1096. DOI: 10.1016/j.jhep.2020.01.007 |
| [49] |
CHOI J, KIM GA, HAN S, et al. Longitudinal assessment of three serum biomarkers to detect very early-stage hepatocellular carcinoma[J]. Hepatology, 2019, 69(5): 1983-1994. DOI: 10.1002/hep.30233 |
| [50] |
LUO P, YIN P, HUA R, et al. A Large-scale, multicenter serum metabolite biomarker identification study for the early detection of hepatocellular carcinoma[J]. Hepatology, 2018, 67(2): 662-675. DOI: 10.1002/hep.29561 |
| [51] |
CHANG TS, WU YC, TUNG SY, et al. Alpha-fetoprotein measurement benefits hepatocellular carcinoma surveillance in patients with cirrhosis[J]. Am J Gastroenterol, 2015, 110(6): 836-844; quiz 845. DOI: 10.1038/ajg.2015.100 |
| [52] |
BRUIX J, SHERMAN M, American Association for the Study of Liver Diseases. Management of hepatocellular carcinoma: An update[J]. Hepatology, 2011, 53(3): 1020-1022. DOI: 10.1002/hep.24199 |
| [53] |
YI X, YU S, BAO Y. Alpha-fetoprotein-L3 in hepatocellular carcinoma: A meta-analysis[J]. Clin Chim Acta, 2013, 425: 212-220. DOI: 10.1016/j.cca.2013.08.005 |
| [54] |
Society for hepatobiliary, Medical society of western retuned scholars association; Society for molecular diagnosis, Chinese research hospital Association, SMD/CRHA; Expert committee for liver cancer, Chinese society of clinical oncology; et al. Consensus for clinical application of molecular diagnosis on hepatobiliary carcinoma[J]. J Clin Hepatol, 2020, 36(7): 1482-1488. (in Chinese) DOI: 10.3969/j.issn.1001-5256.2020.07.008 |
| [55] |
BERHANE S, TOYODA H, TADA T, et al. Role of the GALAD and BALAD-2 serologic models in diagnosis of hepatocellular carcinoma and prediction of survival in patients[J]. Clin Gastroenterol Hepatol, 2016, 14(6): 875-886. e6. DOI: 10.1016/j.cgh.2015.12.042 |
| [56] |
EDOO M, CHUTTURGHOON VK, WUSU-ANSAH GK, et al. Serum biomarkers AFP, CEA and CA19-9 combined detection for early diagnosis of hepatocellular carcinoma[J]. Iran J Public Health, 2019, 48(2): 314-322. http://www.ncbi.nlm.nih.gov/pubmed/31205886 |
| [57] |
TZARTZEVA K, OBI J, RICH NE, et al. Surveillance imaging and alpha fetoprotein for early detection of hepatocellular carcinoma in patients with cirrhosis: A meta-analysis[J]. Gastroenterology, 2018, 154(6): 1706-1718. e1. DOI: 10.1053/j.gastro.2018.01.064 |
| [58] |
SINGAL AG, CONJEEVARAM HS, VOLK ML, et al. Effectiveness of hepatocellular carcinoma surveillance in patients with cirrhosis[J]. Cancer Epidemiol Biomarkers Prev, 2012, 21(5): 793-799. DOI: 10.1158/1055-9965.EPI-11-1005 |
| [59] |
SINGAL A, VOLK ML, WALJEE A, et al. Meta-analysis: Surveillance with ultrasound for early-stage hepatocellular carcinoma in patients with cirrhosis[J]. Aliment Pharmacol Ther, 2009, 30(1): 37-47. DOI: 10.1111/j.1365-2036.2009.04014.x |
| [60] |
KUDO M, UESHIMA K, OSAKI Y, et al. B-Mode ultrasonography versus contrast-enhanced ultrasonography for surveillance of hepatocellular carcinoma: A prospective multicenter randomized controlled trial[J]. Liver Cancer, 2019, 8(4): 271-280. DOI: 10.1159/000501082 |
| [61] |
CELLI N, GAIANI S, PISCAGLIA F, et al. Characterization of liver lesions by real-time contrast-enhanced ultrasonography[J]. Eur J Gastroenterol Hepatol, 2007, 19(1): 3-14. DOI: 10.1097/01.meg.0000250585.53608.3c |
| [62] |
ZHANG J, YU Y, LI Y, et al. Diagnostic value of contrast-enhanced ultrasound in hepatocellular carcinoma: A meta-analysis with evidence from 1998 to 2016[J]. Oncotarget, 2017, 8(43): 75418-75426. DOI: 10.18632/oncotarget.20049 |
| [63] |
HANNA RF, MILOUSHEV VZ, TANG A, et al. Comparative 13-year meta-analysis of the sensitivity and positive predictive value of ultrasound, CT, and MRI for detecting hepatocellular carcinoma[J]. Abdom Radiol (NY), 2016, 41(1): 71-90. DOI: 10.1007/s00261-015-0592-8 |
| [64] |
JIANG HY, CHEN J, XIA CC, et al. Noninvasive imaging of hepatocellular carcinoma: From diagnosis to prognosis[J]. World J Gastroenterol, 2018, 24(22): 2348-2362. DOI: 10.3748/wjg.v24.i22.2348 |
| [65] |
LIM JH, KIM CK, LEE WJ, et al. Detection of hepatocellular carcinomas and dysplastic nodules in cirrhotic livers: Accuracy of helical CT in transplant patients[J]. AJR Am J Roentgenol, 2000, 175(3): 693-698. DOI: 10.2214/ajr.175.3.1750693 |
| [66] |
SANGSTER GP, PREVIGLIANO CH, NADER M, et al. MDCT imaging findings of liver cirrhosis: Spectrum of hepatic and extrahepatic abdominal complications[J]. HPB Surg, 2013, 2013: 129396. http://europepmc.org/articles/PMC3748773 |
| [67] |
ROBERTS LR, SIRLIN CB, ZAIEM F, et al. Imaging for the diagnosis of hepatocellular carcinoma: A systematic review and meta-analysis[J]. Hepatology, 2018, 67(1): 401-421. DOI: 10.1002/hep.29487 |
| [68] |
GUO J, SEO Y, REN S, et al. Diagnostic performance of contrast-enhanced multidetector computed tomography and gadoxetic acid disodium-enhanced magnetic resonance imaging in detecting hepatocellular carcinoma: Direct comparison and a meta-analysis[J]. Abdom Radiol (NY), 2016, 41(10): 1960-1972. DOI: 10.1007/s00261-016-0807-7 |
| [69] |
SANTILLAN C, FOWLER K, KONO Y, et al. LI-RADS major features: CT, MRI with extracellular agents, and MRI with hepatobiliary agents[J]. Abdom Radiol (NY), 2018, 43(1): 75-81. DOI: 10.1007/s00261-017-1291-4 |
| [70] |
PANG EH, HARRIS AC, CHANG SD. Approach to the solitary liver lesion: Imaging and when to biopsy[J]. Can Assoc Radiol J, 2016, 67(2): 130-148. DOI: 10.1016/j.carj.2015.07.005 |
| [71] |
PARK YS, LEE CH, KIM JW, et al. Differentiation of hepatocellular carcinoma from its various mimickers in liver magnetic resonance imaging: What are the tips when using hepatocyte-specific agents?[J]. World J Gastroenterol, 2016, 22(1): 284-299. DOI: 10.3748/wjg.v22.i1.284 |
| [72] |
International Communication Group, Imaging Technology Society of Chinese Medical Association. Expert consensus on hepatobiliary specific contrast agent gadolinium-ethoxybenzyl-diethylenetriamine pentaacetic acid enhanced MRI scanning scheme[J]. J Clin Hepatol, 2020, 36(3): 519-521. (in Chinese) DOI: 10.3969/j.issn.1001-5256.2020.03.008 |
| [73] |
|
| [74] |
LIU X, JIANG H, CHEN J, et al. Gadoxetic acid disodium-enhanced magnetic resonance imaging outperformed multidetector computed tomography in diagnosing small hepatocellular carcinoma: A meta-analysis[J]. Liver Transpl, 2017, 23(12): 1505-1518. DOI: 10.1002/lt.24867 |
| [75] |
RENZULLI M, BISELLI M, BROCCHI S, et al. New hallmark of hepatocellular carcinoma, early hepatocellular carcinoma and high-grade dysplastic nodules on Gd-EOB-DTPA MRI in patients with cirrhosis: A new diagnostic algorithm[J]. Gut, 2018, 67(9): 1674-1682. DOI: 10.1136/gutjnl-2017-315384 |
| [76] |
INCHINGOLO R, FALETTI R, GRAZIOLI L, et al. MR with Gd-EOB-DTPA in assessment of liver nodules in cirrhotic patients[J]. World J Hepatol, 2018, 10(7): 462-473. DOI: 10.4254/wjh.v10.i7.462 |
| [77] |
CASTILLA-LIÈVRE MA, FRANCO D, GERVAIS P, et al. Diagnostic value of combining 11C-choline and 18F-FDG PET/CT in hepatocellular carcinoma[J]. Eur J Nucl Med Mol Imaging, 2016, 43(5): 852-859. DOI: 10.1007/s00259-015-3241-0 |
| [78] |
PUNG L, AHMAD M, MUELLER K, et al. The role of cone-beam CT in transcatheter arterial chemoembolization for hepatocellular carcinoma: A systematic review and Meta-analysis[J]. J Vasc Interv Radiol, 2017, 28(3): 334-341. DOI: 10.1016/j.jvir.2016.11.037 |
| [79] |
SHERMAN M, BRUIX J. Biopsy for liver cancer: How to balance research needs with evidence-based clinical practice[J]. Hepatology, 2015, 61(2): 433-436. DOI: 10.1002/hep.27563 |
| [80] |
JUNG KS, KIM SU, AHN SH, et al. Risk assessment of hepatitis B virus-related hepatocellular carcinoma development using liver stiffness measurement (FibroScan)[J]. Hepatology, 2011, 53(3): 885-894. DOI: 10.1002/hep.24121 |
| [81] |
WANG HM, HUNG CH, LU SN, et al. Liver stiffness measurement as an alternative to fibrotic stage in risk assessment of hepatocellular carcinoma incidence for chronic hepatitis C patients[J]. Liver Int, 2013, 33(5): 756-761. DOI: 10.1111/liv.12118 |
| [82] |
ALEXANDER M, LOOMIS AK, VAN DER LEI J, et al. Risks and clinical predictors of cirrhosis and hepatocellular carcinoma diagnoses in adults with diagnosed NAFLD: Real-world study of 18 million patients in four European cohorts[J]. BMC Med, 2019, 17(1): 95. DOI: 10.1186/s12916-019-1321-x |
| [83] |
YANG B, ZHANG B, XU Y, et al. Prospective study of early detection for primary liver cancer[J]. J Cancer Res Clin Oncol, 1997, 123(6): 357-360. DOI: 10.1007/BF01438313 |
| [84] |
|
| [85] |
KUDO M. Management of hepatocellular carcinoma in Japan as a world-leading model[J]. Liver Cancer, 2018, 7(2): 134-147. DOI: 10.1159/000484619 |
| [86] |
ELSAYES KM, KIELAR AZ, ELMOHR MM, et al. White paper of the Society of Abdominal Radiology hepatocellular carcinoma diagnosis disease-focused panel on LI-RADS v2018 for CT and MRI[J]. Abdom Radiol (NY), 2018, 43(10): 2625-2642. DOI: 10.1007/s00261-018-1744-4 |
| [87] |
SUNG JJ, TSOI KK, WONG VW, et al. Meta-analysis: Treatment of hepatitis B infection reduces risk of hepatocellular carcinoma[J]. Aliment Pharmacol Ther, 2008, 28(9): 1067-1077. DOI: 10.1111/j.1365-2036.2008.03816.x |
| [88] |
WU CY, LIN JT, HO HJ, et al. Association of nucleos(t)ide analogue therapy with reduced risk of hepatocellular carcinoma in patients with chronic hepatitis B: A nationwide cohort study[J]. Gastroenterology, 2014, 147(1): 143-151. e5. DOI: 10.1053/j.gastro.2014.03.048 |
| [89] |
KUANG XJ, JIA RR, HUO RR, et al. Systematic review of risk factors of hepatocellular carcinoma after hepatitis B surface antigen seroclearance[J]. J Viral Hepat, 2018, 25(9): 1026-1037. DOI: 10.1111/jvh.12905 |
| [90] |
Chinese Society of Infectious Diseases, Chinese Medical Association; Chinese Society of Hepatology, Chinese Medical Association. Guidelines for the prevention and treatment of chronic hepatitis B (version 2019)[J]. J Clin Hepatol, 2019, 35(12): 2648-2669. (in Chinese) DOI: 10.3969/j.issn.1001-5256.2019.12.007 |
| [91] |
CARRAT F, FONTAINE H, DORIVAL C, et al. Clinical outcomes in patients with chronic hepatitis C after direct-acting antiviral treatment: A prospective cohort study[J]. Lancet, 2019, 393(10179): 1453-1464. DOI: 10.1016/S0140-6736(18)32111-1 |
| [92] |
KANWAL F, KRAMER J, ASCH SM, et al. Risk of hepatocellular cancer in HCV patients treated with direct-acting antiviral agents[J]. Gastroenterology, 2017, 153(4): 996-1005. e1. DOI: 10.1053/j.gastro.2017.06.012 |
| [93] |
SARASIN FP, GIOSTRA E, HADENGUE A. Cost-effectiveness of screening for detection of small hepatocellular carcinoma in western patients with Child-Pugh class A cirrhosis[J]. Am J Med, 1996, 101(4): 422-434. DOI: 10.1016/S0002-9343(96)00197-0 |
| [94] |
KANWAL F, KRAMER JR, ASCH SM, et al. Long-term risk of hepatocellular carcinoma in HCV patients treated with direct acting antiviral agents[J]. Hepatology, 2020, 71(1): 44-55. DOI: 10.1002/hep.30823 |
| [95] |
Chinese Society of Hepatology and Chinese Society of Infectious Diseases, Chinese Medical Association. The guideline of prevention and treatment for hepatitis C (2019 version)[J]. J Clin Hepatol, 2019, 35(12): 2670-2686. (in Chinese) DOI: 10.3969/j.issn.1001-5256.2019.12.008 |
| [96] |
O'SHEA RS, DASARATHY S, MCCULLOUGH AJ, et al. Alcoholic liver disease[J]. Hepatology, 2010, 51(1): 307-328. DOI: 10.1002/hep.23258 |
| [97] |
National Workshop on Fatty Liver and Alcoholic Liver Disease, Chinese Society of Hepatology, Chinese Medical Association; Fatty Liver Expert Committee, Chinese Medical Doctor Association. Guidelines of prevention and treatment for alcoholic liver disease: A 2018 update[J]. J Clin Hepatol, 2018, 34(5): 939-946. (in Chinese) DOI: 10.3969/j.issn.1001-5256.2018.05.006 |
| [98] |
National Workshop on Fatty Liver and Alcoholic Liver Disease, Chinese Society of Hepatology, Chinese Medical Association; Fatty Liver Expert Committee, Chinese Medical Doctor Association. Guidelines of prevention and treatment for nonalcoholic fatty liver disease: A 2018 update[J]. J Clin Hepatol, 2018, 34(5): 947-957. (in Chinese) DOI: 10.3969/j.issn.1001-5256.2018.05.007 |
| [99] |
MARGINI C, DUFOUR JF. The story of HCC in NAFLD: From epidemiology, across pathogenesis, to prevention and treatment[J]. Liver Int, 2016, 36(3): 317-324. DOI: 10.1111/liv.13031 |
| [100] |
YUN YH, LIM MK, WON YJ, et al. Dietary preference, physical activity, and cancer risk in men: National health insurance corporation study[J]. BMC Cancer, 2008, 8: 366. DOI: 10.1186/1471-2407-8-366 |
| [101] |
|
| [102] |
DONADON V, BALBI M, MAS MD, et al. Metformin and reduced risk of hepatocellular carcinoma in diabetic patients with chronic liver disease[J]. Liver Int, 2010, 30(5): 750-758. DOI: 10.1111/j.1478-3231.2010.02223.x |
| [103] |
WANG JS, SHEN X, HE X, et al. Protective alterations in phase 1 and 2 metabolism of aflatoxin B1 by oltipraz in residents of Qidong, People's Republic of China[J]. J Natl Cancer Inst, 1999, 91(4): 347-354. DOI: 10.1093/jnci/91.4.347 |
| [104] |
EGNER PA, WANG JB, ZHU YR, et al. Chlorophyllin intervention reduces aflatoxin-DNA adducts in individuals at high risk for liver cancer[J]. Proc Natl Acad Sci U S A, 2001, 98(25): 14601-14606. DOI: 10.1073/pnas.251536898 |
| [105] |
Chinese Society of Infectious Diseases, Chinese Medical Association; Committee of experts of consensus statement by the expert committee for prevention and management of liver inflammation in China. Consensus statement by the expert committee for prevention and management of liver inflammation in China[J]. Chin J Hepatol, 2014, 22(2): 94-103. (in Chinese) https://www.cnki.com.cn/Article/CJFDTOTAL-SYNK201402016.htm |
| [106] |
|
| [107] |
|
| [108] |
|
| [109] |
|
| [110] |
|






 DownLoad:
DownLoad: