| [1] |
Pancreas Study Group, Chinese Society of Gastroenterology, Chinese Medical Association; Editorial Board of Chinese Journal of Pancreatology; Editorial Board of Chinese Journal of Digestion. Chinese guidelines for the management of acute pancreatitis (Shenyang, 2019)[J]. J Clin Hepatol, 2019, 35(12): 2706-2711. (in Chinese)
中华医学会消化病学分会胰腺疾病学组, 《中华胰腺病杂志》编委会, 《中华消化杂志》编委会. 中国急性胰腺炎诊治指南(2019年, 沈阳)[J]. 临床肝胆病杂志, 2019, 35(12): 2706-2711.
|
| [2] |
LEPPÄNIEMI A, TOLONEN M, TARASCONI A, et al. 2019 WSES guidelines for the management of severe acute pancreatitis[J]. World J Emerg Surg, 2019, 14: 27. DOI: 10.1186/s13017-019-0247-0 |
| [3] |
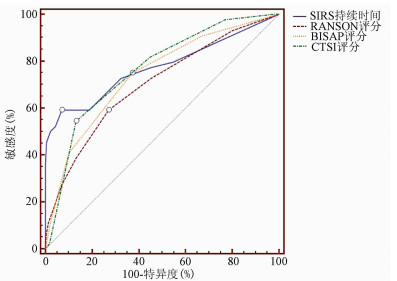
TAN C, YANG L, SHI F, et al. Early systemic inflammatory response syndrome duration predicts infected pancreatic necrosis[J]. J Gastrointest Surg, 2020, 24(3): 590-597. DOI: 10.1007/s11605-019-04149-5 |
| [4] |
SILVA-VAZ P, ABRANTES AM, MORGADO-NUNES S, et al. Evaluation of prognostic factors of severity in acute biliary pancreatitis[J]. Int J Mol Sci, 2020, 21(12) : 4300. DOI: 10.3390/ijms21124300 |
| [5] |
|
| [6] |
SOULOUNTSI V, SCHIZODIMOS T. Use of antibiotics in acute pancreatitis: Ten major concerns[J]. Scand J Gastroenterol, 2020, 55(10): 1211-1218. DOI: 10.1080/00365521.2020.1804995 |
| [7] |
CASE BM, JENSEN KK, BAKIS G, et al. Endoscopic interventions in acute pancreatitis: What the advanced endoscopist wants to know[J]. Radiographics, 2018, 38(7): 2002-2018. DOI: 10.1148/rg.2018180066 |
| [8] |
ARVANITAKIS M, DUMONCEAU JM, ALBERT J, et al. Endoscopic management of acute necrotizing pancreatitis: European Society of Gastrointestinal Endoscopy (ESGE) evidence-based multidisciplinary guidelines[J]. Endoscopy, 2018, 50(5): 524-546. DOI: 10.1055/a-0588-5365 |
| [9] |
TRIKUDANATHAN G, WOLBRINK D, van SANTVOORT HC, et al. Current concepts in severe acute and necrotizing pancreatitis: An evidence-based approach[J]. Gastroenterology, 2019, 156(7): 1994-2007. DOI: 10.1053/j.gastro.2019.01.269 |
| [10] |
SHARMA D, JAKKAMPUDI A, REDDY R, et al. Association of systemic inflammatory and anti-inflammatory responses with adverse outcomes in acute pancreatitis: Preliminary results of an ongoing study[J]. Dig Dis Sci, 2017, 62(12): 3468-3478. DOI: 10.1007/s10620-017-4813-6 |
| [11] |
SENDLER M, van den BRANDT C, GLAUBITZ J, et al. NLRP3 inflammasome regulates development of systemic inflammatory response and compensatory anti-inflammatory response syndromes in mice with acute pancreatitis[J]. Gastroenterology, 2020, 158(1): 253-269. DOI: 10.1053/j.gastro.2019.09.040 |
| [12] |
YANG R, TENHUNEN J, TONNESSEN TI. HMGB1 and histones play a significant role in inducing systemic inflammation and multiple organ dysfunctions in severe acute pancreatitis[J]. Int J Inflam, 2017, 2017: 1817564. http://www.ncbi.nlm.nih.gov/pubmed/28316860 |
| [13] |
|
| [14] |
IYER S, BAWA EP, TARIQUE M, et al. Know thy enemy-understanding the role of inflammation in severe acute pancreatitis[J]. Gastroenterology, 2020, 158(1): 46-48. DOI: 10.1053/j.gastro.2019.11.039 |
| [15] |
DIXIT A, CHEEMA H, GEORGE J, et al. Extracellular release of ATP promotes systemic inflammation during acute pancreatitis[J]. Am J Physiol Gastrointest Liver Physiol, 2019, 317(4): g463-g475. DOI: 10.1152/ajpgi.00395.2018 |
| [16] |
DUMNICKA P, MADUZIA D, CERANOWICZ P, et al. The interplay between inflflammation, coagulation and endothelial injury in the early phase of acute pancreatitis: Clinical implications[J]. Int J Mol Sci, 2017, 18(2): 354. DOI: 10.3390/ijms18020354 |
| [17] |
GAD MM, SIMONS-LINARES CR. Is aggressive intravenous fluid resuscitation beneficial in acute pancreatitis? A meta-analysis of randomized control trials and cohort studies[J]. World J Gastroenterol, 2020, 26(10): 1098-1106. DOI: 10.3748/wjg.v26.i10.1098 |
| [18] |
YE B, MAO W, CHEN Y, et al. Aggressive resuscitation is associated with the development of acute kidney injury in acute pancreatitis[J]. Dig Dis Sci, 2019, 64(2): 544-552. DOI: 10.1007/s10620-018-5328-5 |
| [19] |
CHOOSAKUL S, HARINWAN K, CHIRAPONGSATHORN S, et al. Comparison of normal saline versus Lactated Ringer's solution for fluid resuscitation in patients with mild acute pancreatitis, A randomized controlled trial[J]. Pancreatology, 2018, 18(5): 507-512. DOI: 10.1016/j.pan.2018.04.016 |
| [20] |
FROGHI F, SOGGIU F, RICCIARDI F, et al. Ward-based goal-directed fluid therapy (GDFT) in acute pancreatitis (GAP) trial: Study protocol for a feasibility randomised controlled trial[J]. BMJ Open, 2019, 9(10): e028783. DOI: 10.1136/bmjopen-2018-028783 |
| [21] |
WOLBRINK D, GRUNDSELL JR, WITTEMAN B, et al. Are omega-3 fatty acids safe and effective in acute pancreatitis or sepsis? A systematic review and meta-analysis[J]. Clin Nutr, 2020, 39(9): 2686-2694. DOI: 10.1016/j.clnu.2019.12.006 |
| [22] |
RUIZ-REBOLLO ML, MUÑOZ-MORENO MF, MAYO-ISCAR A, et al. Statin intake can decrease acute pancreatitis severit[J]. Pancreatology, 2019, 19(6): 807-812. DOI: 10.1016/j.pan.2019.07.004 |
| [23] |
|
| [24] |
TIAN H, CHEN L, WU X, et al. Infectious complications in severe acute pancreatitis: Pathogens, drug resistance, and status of nosocomial infection in a university-affiliated teaching hospital[J]. Dig Dis Sci, 2020, 65(7): 2079-2088. DOI: 10.1007/s10620-019-05924-9 |
| [25] |
BARON TH, DIMAIO CJ, WANG AY, et al. American Gastroenterological association clinical practice update: Management of pancreatic necrosis[J]. Gastroenterology, 2020, 158(1): 67-75. DOI: 10.1053/j.gastro.2019.07.064 |
| [26] |
SUSAK YM, DIRDA OO, FEDORCHUK OG, et al. Infectious complications of acute pancreatitis is associated with peripheral blood phagocyte functional exhaustion[J]. Dig Dis Sci, 2020.[Online ahead of print]
|
| [27] |
LU JD, CAO F, DING YX, et al. Timing, distribution, and microbiology of infectious complications after necrotizing pancreatitis[J]. World J Gastroenterol, 2019, 25(34): 5162-5173. DOI: 10.3748/wjg.v25.i34.5162 |
| [28] |
AUSANIA F, SENRA DEL RÍO P, BORIN A, et al. Factors associated with mortality in patients with infected pancreatic necrosis: The "surgery effect"[J]. Updates Surg, 2020, 72(4): 1097-1103. DOI: 10.1007/s13304-020-00764-z |
| [29] |
ZHANG ZH, DING YX, WU YD, et al. A meta-analysis and systematic review of percutaneous catheter drainage in treating infected pancreatitis necrosis[J]. Medicine (Baltimore), 2018, 97(47): e12999. DOI: 10.1097/MD.0000000000012999 |
| [30] |
DARRIVERE L, LAPIDUS N, COLIGNON N, et al. Minimally invasive drainage in critically ill patients with severe necrotizing pancreatitis is associated with better outcomes: An observational study[J]. Crit Care, 2018, 22(1): 321. DOI: 10.1186/s13054-018-2256-x |
| [31] |
SUN B, LI GQ. Surgical intervention strategies for local complications of severe acute pancreatitis[J]. Chin J Dig Surg, 2020, 19(4): 379-383. (in Chinese)
|













 DownLoad:
DownLoad: