| [1] |
Chinese Society of Hepatology, Chinese Medical Association. Chinese guidelines on the management of liver cirrhosis[J]. J Clin Hepatol, 2019, 35(11): 2408-2425. DOI: 10.3969/j.issn.1001-5256.2019.11.006. |
| [2] |
SASS DA, CHOPRA KB. Portal hypertension and variceal hemorrhage[J]. Med Clin North Am, 2009, 93(4): 837-853, ⅶ-ⅷ. DOI: 10.1016/j.mcna.2009.03.008. |
| [3] |
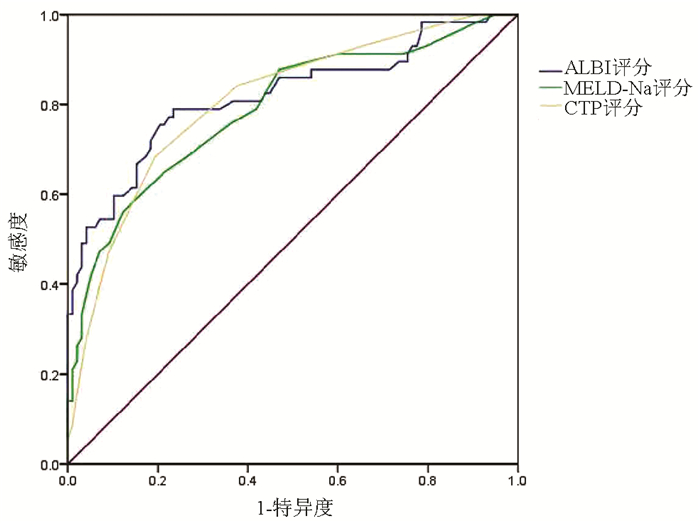
WAN SZ, NIE Y, ZHANG Y, et al. Assessing the prognostic performance of the Child-Pugh, Model for End-Stage Liver Disease, and Albumin-Bilirubin scores in patients with decompensated cirrhosis: A large asian cohort from gastroenterology department[J]. Dis Markers, 2020, 2020: 5193028. DOI: 10.1155/2020/5193028. |
| [4] |
KAMATH PS, WIESNER RH, MALINCHOC M, et al. A model to predict survival in patients with end-stage liver disease[J]. Hepatology, 2001, 33(2): 464-470. DOI: 10.1053/jhep.2001.22172. |
| [5] |
PUGH RN, MURRAY-LYON IM, DAWSON JL, et al. Transection of the oesophagus for bleeding oesophageal varices[J]. Br J Surg, 1973, 60(8): 646-649. DOI: 10.1002/bjs.1800600817. |
| [6] |
CREMERS I, RIBEIRO S. Management of variceal and nonvariceal upper gastrointestinal bleeding in patients with cirrhosis[J]. Therap Adv Gastroenterol, 2014, 7(5): 206-216. DOI: 10.1177/1756283X14538688. |
| [7] |
D'AMICO G, GARCIA-TSAO G, PAGLIARO L. Natural history and prognostic indicators of survival in cirrhosis: A systematic review of 118 studies[J]. J Hepatol, 2006, 44(1): 217-231. DOI: 10.1016/j.jhep.2005.10.013. |
| [8] |
JOHNSON PJ, BERHANE S, KAGEBAYASHI C, et al. Assessment of liver function in patients with hepatocellular carcinoma: A new evidence-based approach-the ALBI grade[J]. J Clin Oncol, 2015, 33(6): 550-558. DOI: 10.1200/JCO.2014.57.9151. |
| [9] |
BIYIK M, UCAR R, SOLAK Y, et al. Blood neutrophil-to-lymphocyte ratio independently predicts survival in patients with liver cirrhosis[J]. Eur J Gastroenterol Hepatol, 2013, 25(4): 435-441. DOI: 10.1097/MEG.0b013e32835c2af3. |
| [10] |
MALINCHOC M, KAMATH PS, GORDON FD, et al. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts[J]. Hepatology, 2000, 31(4): 864-871. DOI: 10.1053/he.2000.5852. |
| [11] |
XAVIER SA, VILAS-BOAS R, BOAL CARVALHO P, et al. Assessment of prognostic performance of Albumin-Bilirubin, Child-Pugh, and Model for End-stage Liver Disease scores in patients with liver cirrhosis complicated with acute upper gastrointestinal bleeding[J]. Eur J Gastroenterol Hepatol, 2018, 30(6): 652-658. DOI: 10.1097/MEG.0000000000001087. |
| [12] |
PORTE RJ, LISMAN T, TRIPODI A, et al. The International Normalized Ratio (INR) in the MELD score: Problems and solutions[J]. Am J Transplant, 2010, 10(6): 1349-1353. DOI: 10.1111/j.1600-6143.2010.03064.x. |
| [13] |
KNOX JJ. Addressing the interplay of liver disease and hepatocellular carcinoma on patient survival: The ALBI scoring model[J]. J Clin Oncol, 2015, 33(6): 529-531. DOI: 10.1200/JCO.2014.59.0521. |
| [14] |
LEI Q, ZHANG Y, KE C, et al. Value of the albumin-bilirubin score in the evaluation of hepatitis B virus-related acute-on-chronic liver failure, liver cirrhosis, and hepatocellular carcinoma[J]. Exp Ther Med, 2018, 15(3): 3074-3079. DOI: 10.3892/etm.2018.5748. |
| [15] |
CHAN AW, CHAN RC, WONG GL, et al. New simple prognostic score for primary biliary cirrhosis: Albumin-bilirubin score[J]. J Gastroenterol Hepatol, 2015, 30(9): 1391-1396. DOI: 10.1111/jgh.12938. |
| [16] |
ZOU D, QI X, ZHU C, et al. Albumin-bilirubin score for predicting the in-hospital mortality of acute upper gastrointestinal bleeding in liver cirrhosis: A retrospective study[J]. Turk J Gastroenterol, 2016, 27(2): 180-186. DOI: 10.5152/tjg.2016.15502. |
| [17] |
LU JJ, ZHANG L, DING SG, et al. The prognosis of liver cirrhotic patients with acute esophageal variceal bleeding: A Cox regression analysis[J]. Chin J Dig, 2011, 31(4): 217-220. DOI: 10.3760/cma.j.issn.0254-1432.2011.04.001. |
| [18] |
CUI S, WANG F, LYU HM, et al. Value of Glasgow-Blatchford score in predicting early prognosis of cirrhotic patients with esophagogastric variceal bleeding[J]. J Clin Hepatol, 2017, 33(10): 1939-1943. DOI: 10.3969/j.issn.1001-5256.2017.10.018. |








 本站查看
本站查看






 DownLoad:
DownLoad: