| [1] |
KOKUDO N, TAKEMURA N, ITO K, et al. The history of liver surgery: Achievements over the past 50 years[J]. Ann Gastroenterol Surg, 2020, 4(2): 109-117. DOI: 10.1002/ags3.12322. |
| [2] |
BUELL JF, CHERQUI D, GELLER DA, et al. The international position on laparoscopic liver surgery: The Louisville Statement, 2008[J]. Ann Surg, 2009, 250(5): 825-830. DOI: 10.1097/sla.0b013e3181b3b2d8. |
| [3] |
WAKABAYASHI G, CHERQUI D, GELLER DA, et al. Recommendations for laparoscopic liver resection: A report from the second international consensus conference held in Morioka[J]. Ann Surg, 2015, 261(4): 619-629. DOI: 10.1097/SLA.0000000000001184. |
| [4] |
KOMATSU S, SCATTON O, GOUMARD C, et al. Development process and technical aspects of laparoscopic hepatectomy: Learning curve based on 15 years of experience[J]. J Am Coll Surg, 2017, 224(5): 841-850. DOI: 10.1016/j.jamcollsurg.2016.12.037. |
| [5] |
BROWN KM, GELLER DA. What is the learning curve for laparoscopic major hepatectomy?[J]. J Gastrointest Surg, 2016, 20(5): 1065-1071. DOI: 10.1007/s11605-016-3100-8. |
| [6] |
ABU HILAL M, ALDRIGHETTI L, DAGHER I, et al. The Southampton Consensus Guidelines for laparoscopic liver surgery: From indication to implementation[J]. Ann Surg, 2018, 268(1): 11-18. DOI: 10.1097/SLA.0000000000002524. |
| [7] |
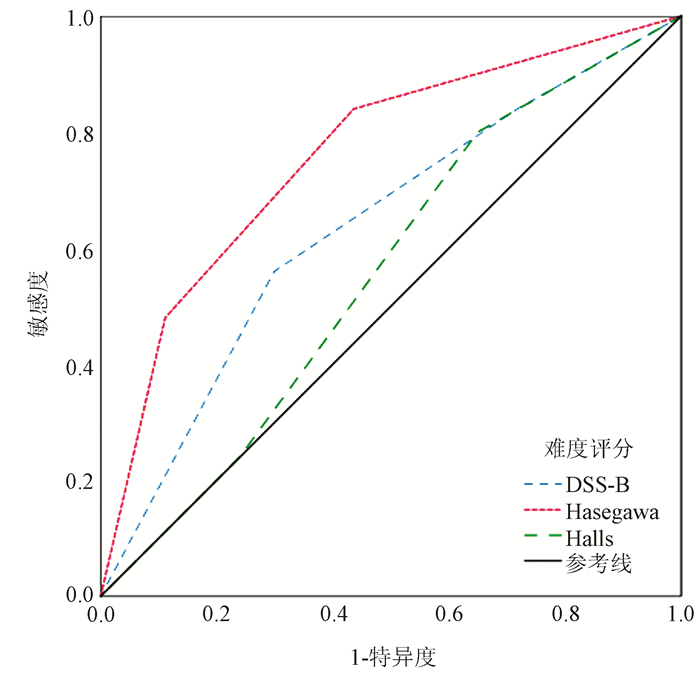
BAN D, TANABE M, ITO H, et al. A novel difficulty scoring system for laparoscopic liver resection[J]. J Hepatobiliary Pancreat Sci, 2014, 21(10): 745-753. DOI: 10.1002/jhbp.166. |
| [8] |
GUO Y, LIAO R, LUO F. Establishment of surgical difficulty scoring system for laparoscopic liver resection and its application[J]. Chin J Gen Surg, 2018, 27(1): 22-28. DOI: 10.3978/j.issn.1005-6947.2018.01.004. |
| [9] |
KAWAGUCHI Y, FUKS D, KOKUDO N, et al. Difficulty of laparoscopic liver resection: Proposal for a new classification[J]. Ann Surg, 2018, 267(1): 13-17. DOI: 10.1097/SLA.0000000000002176. |
| [10] |
HASEGAWA Y, WAKABAYASHI G, NITTA H, et al. A novel model for prediction of pure laparoscopic liver resection surgical difficulty[J]. Surg Endosc, 2017, 31(12): 5356-5363. DOI: 10.1007/s00464-017-5616-8. |
| [11] |
HALLS MC, BERARDI G, CIPRIANI F, et al. Development and validation of a difficulty score to predict intraoperative complications during laparoscopic liver resection[J]. Br J Surg, 2018, 105(9): 1182-1191. DOI: 10.1002/bjs.10821. |
| [12] |
The Hepatic Surgery Group of Chinese Medical Association. Expert consensus on laparoscopic hepatectomy and guideline for operative procedure (2013 edition)[J]. Chin J Dig Surg, 2013, 12(3): 161-165. DOI: 10.3760/cma.j.issn.1673-9752.2013.03.001. |
| [13] |
BELGHITI J, CLAVIEN P, GADZIJEV E, et al. The Brisbane 2000 terminology of liver anatomy and resections[J]. HPB, 2000, 2(3): 333-339. DOI: 10.1016/S1365-182X(17)30755-4. |
| [14] |
CLAVIEN PA, BARKUN J, de OLIVEIRA ML, et al. The Clavien-Dindo classification of surgical complications: Five-year experience[J]. Ann Surg, 2009, 250(2): 187-196. DOI: 10.1097/SLA.0b013e3181b13ca2. |
| [15] |
|
| [16] |
HAN HS, SHEHTA A, AHN S, et al. Laparoscopic versus open liver resection for hepatocellular carcinoma: Case-matched study with propensity score matching[J]. J Hepatol, 2015, 63(3): 643-650. DOI: 10.1016/j.jhep.2015.04.005. |
| [17] |
CIRIA R, CHERQUI D, GELLER DA, et al. Comparative short-term benefits of laparoscopic liver resection: 9000 cases and climbing[J]. Ann Surg, 2016, 263(4): 761-777. DOI: 10.1097/SLA.0000000000001413. |
| [18] |
XIANG L, LI J, CHEN J, et al. Prospective cohort study of laparoscopic and open hepatectomy for hepatocellular carcinoma[J]. Br J Surg, 2016, 103(13): 1895-1901. DOI: 10.1002/bjs.10294. |
| [19] |
YOON YI, KIM KH, CHO HD, et al. Long-term perioperative outcomes of pure laparoscopic liver resection versus open liver resection for hepatocellular carcinoma: A retrospective study[J]. Surg Endosc, 2020, 34(2): 796-805. DOI: 10.1007/s00464-019-06831-w. |
| [20] |
ZHANG NP, ZHANG XJ. Evaluation of different hepatic blood flow blocking methods in laparoscopic hepatectomy of patients with liver cancer[J/CD]. Chin J Liver Dis (Electronic Version), 2019, 11(3): 58-63. DOI: 10.3969/j.issn.1674-7380.2019.03.011. |
| [21] |
CIRIA R, AYLLON MD, BRICEÑO J. Difficulty scores in laparoscopic liver surgery-getting closer to a powerful and necessary tool[J]. Hepatobiliary Surg Nutr, 2019, 8(4): 428-430. DOI: 10.21037/hbsn.2019.02.11. |
| [22] |
IM C, CHO JY, HAN HS, et al. Validation of difficulty scoring system for laparoscopic liver resection in patients who underwent laparoscopic left lateral sectionectomy[J]. Surg Endosc, 2017, 31(1): 430-436. DOI: 10.1007/s00464-016-4994-7. |
| [23] |
LEE SY, GOH B, SEPIDEH G, et al. Laparoscopic liver resection difficulty score-a validation study[J]. J Gastrointest Surg, 2019, 23(3): 545-555. DOI: 10.1007/s11605-018-4036-y. |
| [24] |
XIA AD, WANG W, BAI G, et al. Practicability of surgical difficulty scoring model for laparoscopic liver resection[J/CD]. Chin J Laparoscopic Surgery (Electronic Edition), 2020, 13(3): 166-172. DOI: 10.3877/cma.j.issn.1674-6899.2020.03.009. |
| [25] |
YANG J, YANG Z, JIA G, et al. Clinical practicality study of the difficulty scoring systems DSS-B and DSS-ER in laparoscopic liver resection[J]. J Laparoendosc Adv Surg Tech A, 2019, 29(1): 12-18. DOI: 10.1089/lap.2018.0150. |
| [26] |
RUSSOLILLO N, MAINA C, FLERES F, et al. Comparison and validation of three difficulty scoring systems in laparoscopic liver surgery: A retrospective analysis on 300 cases[J]. Surg Endosc, 2020, 34(12): 5484-5494. DOI: 10.1007/s00464-019-07345-1. |
| [27] |
RATTI F, D'ALESSANDRO V, CIPRIANI F, et al. Influence of body habitus on feasibility and outcome of laparoscopic liver resections: A prospective study[J]. J Hepatobiliary Pancreat Sci, 2016, 23(6): 373-381. DOI: 10.1002/jhbp.350. |
| [28] |
TRIPKE V, HUBER T, MITTLER J, et al. Prediction of complexity and complications of laparoscopic liver surgery: The comparison of the Halls-score to the IWATE-score in 100 consecutive laparoscopic liver resections[J]. J Hepatobiliary Pancreat Sci, 2020, 27(7): 380-387. DOI: 10.1002/jhbp.731. |













 DownLoad:
DownLoad: