| [1] |
LOOSEN SH, CASTOLDI M, JÖRDENS MS, et al. Serum levels of circulating microRNA-107 are elevated in patients with early-stage HCC[J]. PLoS One, 2021, 16(3): e0247917. DOI: 10.1371/journal.pone.0247917. |
| [2] |
GAO Y, LYU L, FENG Y, et al. A review of cutting-edge therapies for hepatocellular carcinoma (HCC): Perspectives from patents[J]. Int J Med Sci, 2021, 18(14): 3066-3081. DOI: 10.7150/ijms.59930. |
| [3] |
XING M, WANG X, KIKEN RA, et al. Immunodiagnostic biomarkers for hepatocellular carcinoma (HCC): The first step in detection and treatment[J]. Int J Mol Sci, 2021, 22(11) : 6139. DOI: 10.3390/ijms22116139. |
| [4] |
SUPINSKI GS, SCHRODER EA, CALLAHAN LA. Mitochondria and critical illness[J]. Chest, 2020, 157(2): 310-322. DOI: 10.1016/j.chest.2019.08.2182. |
| [5] |
MIDDLETON P, VERGIS N. Mitochondrial dysfunction and liver disease: Role, relevance, and potential for therapeutic modulation[J]. Therap Adv Gastroenterol, 2021, 14: 17562848211031394. DOI: 10.1177/17562848211031394. |
| [6] |
LIAO ZB, TAN XL, DONG KS, et al. miRNA-448 inhibits cell growth by targeting BCL-2 in hepatocellular carcinoma[J]. Dig Liver Dis, 2019, 51(5): 703-711. DOI: 10.1016/j.dld.2018.09.021. |
| [7] |
YIN PH, LEE HC, CHAU GY, et al. Alteration of the copy number and deletion of mitochondrial DNA in human hepatocellular carcinoma[J]. Br J Cancer, 2004, 90(12): 2390-2396. DOI: 10.1038/sj.bjc.6601838. |
| [8] |
HERNÁNDEZ-ALVAREZ MI, ZORZANO A. Mitochondrial dynamics and liver cancer[J]. Cancers (Basel), 2021, 13(11): 2571. DOI: 10.3390/cancers13112571. |
| [9] |
LI Y, GUO X, GUO S, et al. Next generation sequencing-based analysis of mitochondrial DNA characteristics in plasma extracellular vesicles of patients with hepatocellular carcinoma[J]. Oncol Lett, 2020, 20(3): 2820-2828. DOI: 10.3892/ol.2020.11831. |
| [10] |
JIN M, WANG J, JI X, et al. MCUR1 facilitates epithelial-mesenchymal transition and metastasis via the mitochondrial calcium dependent ROS/Nrf2/Notch pathway in hepatocellular carcinoma[J]. J Exp Clin Cancer Res, 2019, 38(1): 136. DOI: 10.1186/s13046-019-1135-x. |
| [11] |
SUN H, YU J, WEN Z, et al. Decreased expression of Beclin-1 in patients with hepatocellular carcinoma[J]. J BUON, 2019, 24(2): 634-641.
|
| [12] |
FUNK K, CZAUDERNA C, KLESSE R, et al. BAX redistribution induces apoptosis resistance and selective stress sensitivity in human HCC[J]. Cancers (Basel), 2020, 12(6) : 1437. DOI: 10.3390/cancers12061437. |
| [13] |
LE PH, HUANG SC, LIM SN, et al. Complex Ⅳ subunit 1 defect predicts postoperative survival in hepatocellular carcinoma[J]. Oncol Lett, 2014, 7(5): 1430-1438. DOI: 10.3892/ol.2014.1966. |
| [14] |
XIAO MH, LIN YF, XIE PP, et al. Downregulation of a mitochondrial micropeptide, MPM, promotes hepatoma metastasis by enhancing mitochondrial complex I activity[J]. Mol Ther, 2022, 30(2): 714-725. DOI: 10.1016/j.ymthe.2021.08.032. |
| [15] |
WANG T, XIE X, LIU H, et al. Pyridine nucleotide-disulphide oxidoreductase domain 2 (PYROXD2): Role in mitochondrial function[J]. Mitochondrion, 2019, 47: 114-124. DOI: 10.1016/j.mito.2019.05.007. |
| [16] |
LI Y, LIN S, LI L, et al. PDSS2 Deficiency Induces hepatocarcinogenesis by decreasing mitochondrial respiration and reprogramming glucose metabolism[J]. Cancer Res, 2018, 78(16): 4471-4481. DOI: 10.1158/0008-5472.CAN-17-2172. |
| [17] |
ZHANG Z, LI TE, CHEN M, et al. MFN1-dependent alteration of mitochondrial dynamics drives hepatocellular carcinoma metastasis by glucose metabolic reprogramming[J]. Br J Cancer, 2020, 122(2): 209-220. DOI: 10.1038/s41416-019-0658-4. |
| [18] |
WANG X, LIU Y, SUN J, et al. Mitofusin-2 acts as biomarker for predicting poor prognosis in hepatitis B virus related hepatocellular carcinoma[J]. Infect Agent Cancer, 2018, 13: 36. DOI: 10.1186/s13027-018-0212-7. |
| [19] |
ANDERSON S, BANKIER AT, BARRELL BG, et al. Sequence and organization of the human mitochondrial genome[J]. Nature, 1981, 290(5806): 457-465. DOI: 10.1038/290457a0. |
| [20] |
GUO ZS, JIN CL, YAO ZJ, et al. Analysis of the mitochondrial 4977 bp deletion in patients with hepatocellular carcinoma[J]. Balkan J Med Genet, 2017, 20(1): 81-86. DOI: 10.1515/bjmg-2017-0006. |
| [21] |
HUNG WY, LIN JC, LEE LM, et al. Tandem duplication/triplication correlated with poly-cytosine stretch variation in human mitochondrial DNA D-loop region[J]. Mutagenesis, 2008, 23(2): 137-142. DOI: 10.1093/mutage/gen002. |
| [22] |
HIGURASHI M, MARUYAMA T, NOGAMI Y, et al. High expression of FOXM1 critical for sustaining cell proliferation in mitochondrial DNA-less liver cancer cells[J]. Exp Cell Res, 2020, 389(1): 111889. DOI: 10.1016/j.yexcr.2020.111889. |
| [23] |
ROMERO-GARCIA S, PRADO-GARCIA H. Mitochondrial calcium: Transport and modulation of cellular processes in homeostasis and cancer (Review)[J]. Int J Oncol, 2019, 54(4): 1155-1167. DOI: 10.3892/ijo.2019.4696. |
| [24] |
LI CJ, LIN HY, KO CJ, et al. A novel biomarker driving poor-prognosis liver cancer: overexpression of the mitochondrial calcium gatekeepers[J]. Biomedicines, 2020, 8(11): 451. DOI: 10.3390/biomedicines8110451. |
| [25] |
KOIKE K. Molecular basis of hepatitis C virus-associated hepatocarcinogenesis: Lessons from animal model studies[J]. Clin Gastroenterol Hepatol, 2005, 3(10 Suppl 2): S132-S135. DOI: 10.1016/s1542-3565(05)00700-7. |
| [26] |
ZHANG R, ZHANG F, WANG C, et al. Identification of sequence polymorphism in the D-Loop region of mitochondrial DNA as a risk factor for hepatocellular carcinoma with distinct etiology[J]. J Exp Clin Cancer Res, 2010, 29: 130. DOI: 10.1186/1756-9966-29-130. |
| [27] |
JIN Y, YU Q, ZHOU D, et al. The mitochondrial DNA 9-bp deletion polymorphism is a risk factor for hepatocellular carcinoma in the Chinese population[J]. Genet Test Mol Biomarkers, 2012, 16(5): 330-334. DOI: 10.1089/gtmb.2011.0208. |
| [28] |
AHMED HS, WAHAB EA, ELHADY HA, et al. Association of genetic polymorphism of BCL-2 (rs2279115) with susceptibility to HCV-related hepatocellular carcinoma[J]. Immunol Res, 2020, 68(4): 189-197. DOI: 10.1007/s12026-020-09143-7. |
| [29] |
HUANG Q, ZHAN L, CAO H, et al. Increased mitochondrial fission promotes autophagy and hepatocellular carcinoma cell survival through the ROS-modulated coordinated regulation of the NFKB and TP53 pathways[J]. Autophagy, 2016, 12(6): 999-1014. DOI: 10.1080/15548627.2016.1166318. |
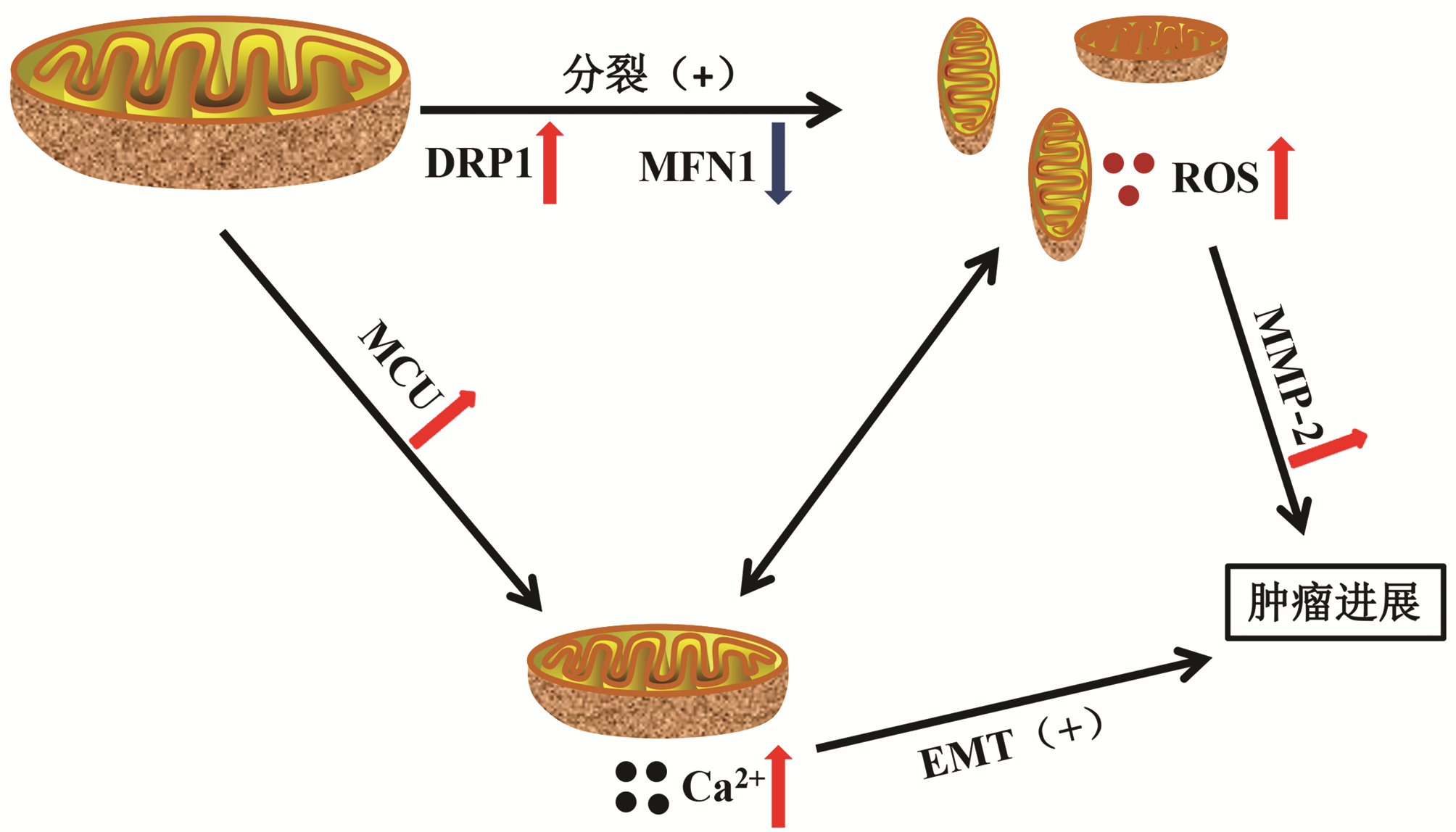
| [30] |
REN T, ZHANG H, WANG J, et al. MCU-dependent mitochondrial Ca 2+ inhibits NAD +/SIRT3/SOD2 pathway to promote ROS production and metastasis of HCC cells[J]. Oncogene, 2017, 36(42): 5897-5909. DOI: 10.1038/onc.2017.167. |
| [31] |
HU W, FU J, LU SX, et al. Decrease of Bcl-xL/Bcl-2-associated death promoter in hepatocellular carcinoma indicates poor prognosis[J]. Am J Cancer Res, 2015, 5(5): 1805-1813.
|
| [32] |
LI S, WAN P, PENG T, et al. Associations between sequence variations in the mitochondrial DNA D-loop region and outcome of hepatocellular carcinoma[J]. Oncol Lett, 2016, 11(6): 3723-3728. DOI: 10.3892/ol.2016.4466. |
| [33] |
JIAN C, FU J, CHENG X, et al. Low-dose sorafenib acts as a mitochondrial uncoupler and ameliorates nonalcoholic steatohepatitis[J]. Cell Metab, 2020, 31(5): 892-908. e11. DOI: 10.1016/j.cmet.2020.04.011. |
| [34] |
CHIOU JF, TAI CJ, WANG YH, et al. Sorafenib induces preferential apoptotic killing of a drug- and radio-resistant Hep G2 cells through a mitochondria-dependent oxidative stress mechanism[J]. Cancer Biol Ther, 2009, 8(20): 1904-1913. DOI: 10.4161/cbt.8.20.9436. |
| [35] |
LI Y, XIA J, SHAO F, et al. Sorafenib induces mitochondrial dysfunction and exhibits synergistic effect with cysteine depletion by promoting HCC cells ferroptosis[J]. Biochem Biophys Res Commun, 2021, 534: 877-884. DOI: 10.1016/j.bbrc.2020.10.083. |
| [36] |
ZHANG C, HU J, SHENG L, et al. Metformin delays AKT/c-Met-driven hepatocarcinogenesis by regulating signaling pathways for de novo lipogenesis and ATP generation[J]. Toxicol Appl Pharmacol, 2019, 365: 51-60. DOI: 10.1016/j.taap.2019.01.004. |
| [37] |
YE RR, PENG W, CHEN BC, et al. Mitochondria-targeted artesunate conjugated cyclometalated iridium(iii) complexes as potent anti-HepG2 hepatocellular carcinoma agents[J]. Metallomics, 2020, 12(7): 1131-1141. DOI: 10.1039/d0mt00060d. |
| [38] |
PITTALA S, KRELIN Y, SHOSHAN-BARMATZ V. Targeting liver cancer and associated pathologies in mice with a mitochondrial VDAC1-based peptide[J]. Neoplasia, 2018, 20(6): 594-609. DOI: 10.1016/j.neo.2018.02.012. |







 DownLoad:
DownLoad: