| [1] |
ESLAM M, NEWSOME PN, SARIN SK, et al. A new definition for metabolic dysfunction-associated fatty liver disease: An international expert consensus statement[J]. J Hepatol, 2020, 73(1): 202-209. DOI: 10.1016/j.jhep.2020.03.039. |
| [2] |
COTTER TG, RINELLA M. Nonalcoholic fatty liver disease 2020: The state of the disease[J]. Gastroenterology, 2020, 158(7): 1851-1864. DOI: 10.1053/j.gastro.2020.01.052. |
| [3] |
ZHOU F, ZHOU J, WANG W, et al. Unexpected rapid increase in the burden of NAFLD in China from 2008 to 2018: A systematic review and Meta-analysis[J]. Hepatology, 2019, 70(4): 1119-1133. DOI: 10.1002/hep.30702. |
| [4] |
XIAO QQ, WANG MY, FAN JG. Brief introduction of APASL clinical practice guidelines on metabolic associated fatty liver disease (Treatment Part)[J]. J Clin Hepatol, 2021, 37(1): 41-45. DOI: 10.3969/j.issn.1001-5256.2021.01.009. |
| [5] |
ANDERSON JL, MAY HT, HORNE BD, et al. Relation of vitamin D deficiency to cardiovascular risk factors, disease status, and incident events in a general healthcare population[J]. Am J Cardiol, 2010, 106(7): 963-968. DOI: 10.1016/j.amjcard.2010.05.027. |
| [6] |
MA JT, CAI S, WAN L, et al. Research progress in the effect of vitamin D deficiency on skeletal and extraskeletal health[J]. Chin J Osteoporosis, 2020, 26(1): 109-113. DOI: 10.3969/j.issn.1006-7108.
|
| [7] |
PACIFICO L, OSBORN JF, BONCI E, et al. Association between vitamin D levels and nonalcoholic fatty liver disease: Potential confounding variables[J]. Mini Rev Med Chem, 2019, 19(4): 310-332. DOI: 10.2174/1389557518666181025153712. |
| [8] |
van SCHOOR N, LIPS P. Global overview of vitamin D status[J]. Endocrinol Metab Clin North Am, 2017, 46(4): 845-870. DOI: 10.1016/j.ecl.2017.07.002. |
| [9] |
LI M, LV F, ZHANG Z, et al. Establishment of a normal reference value of parathyroid hormone in a large healthy Chinese population and evaluation of its relation to bone turnover and bone mineral density[J]. Osteoporos Int, 2016, 27(5): 1907-1916. DOI: 10.1007/s00198-015-3475-5. |
| [10] |
WAN B, GAO Y, ZHENG Y, et al. Association between serum 25-hydroxy vitamin D level and metabolic associated fatty liver disease (MAFLD)-a population-based study[J]. Endocr J, 2021, 68(6): 631-637. DOI: 10.1507/endocrj.EJ20-0758. |
| [11] |
NELSON JE, ROTH CL, WILSON LA, et al. Vitamin D deficiency is associated with increased risk of non-alcoholic steatohepatitis in adults with non-alcoholic fatty liver disease: possible role for MAPK and NF-κB?[J]. Am J Gastroenterol, 2016, 111(6): 852-863. DOI: 10.1038/ajg.2016.51. |
| [12] |
ARAI T, ATSUKAWA M, TSUBOTA A, et al. Association of vitamin D levels and vitamin D-related gene polymorphisms with liver fibrosis in patients with biopsy-proven nonalcoholic fatty liver disease[J]. Dig Liver Dis, 2019, 51(7): 1036-1042. DOI: 10.1016/j.dld.2018.12.022. |
| [13] |
YANG BB, CHEN YH, ZHANG C, et al. Low vitamin D status is associated with advanced liver fibrosis in patients with nonalcoholic fatty liver disease[J]. Endocrine, 2017, 55(2): 582-590. DOI: 10.1007/s12020-016-1152-x. |
| [14] |
ZHAI HL, WANG NJ, HAN B, et al. Low vitamin D levels and non-alcoholic fatty liver disease, evidence for their independent association in men in East China: a cross-sectional study (Survey on Prevalence in East China for Metabolic Diseases and Risk Factors (SPECT-China))[J]. Br J Nutr, 2016, 115(8): 1352-1359. DOI: 10.1017/S0007114516000386. |
| [15] |
DUTRA J, LISBOA QC, FEROLLA SM, et al. Vitamin D levels are not associated with non-alcoholic fatty liver disease severity in a Brazilian population[J]. Int J Vitam Nutr Res, 2021, 91(5-6): 411-418. DOI: 10.1024/0300-9831/a000667. |
| [16] |
LI L, ZHANG L, PAN S, et al. No significant association between vitamin D and nonalcoholic fatty liver disease in a Chinese population[J]. Dig Dis Sci, 2013, 58(8): 2376-2382. DOI: 10.1007/s10620-013-2658-1. |
| [17] |
BUZZETTI E, PINZANI M, TSOCHATZIS EA. The multiple-hit pathogenesis of non-alcoholic fatty liver disease (NAFLD)[J]. Metabolism, 2016, 65(8): 1038-1048. DOI: 10.1016/j.metabol.2015.12.012. |
| [18] |
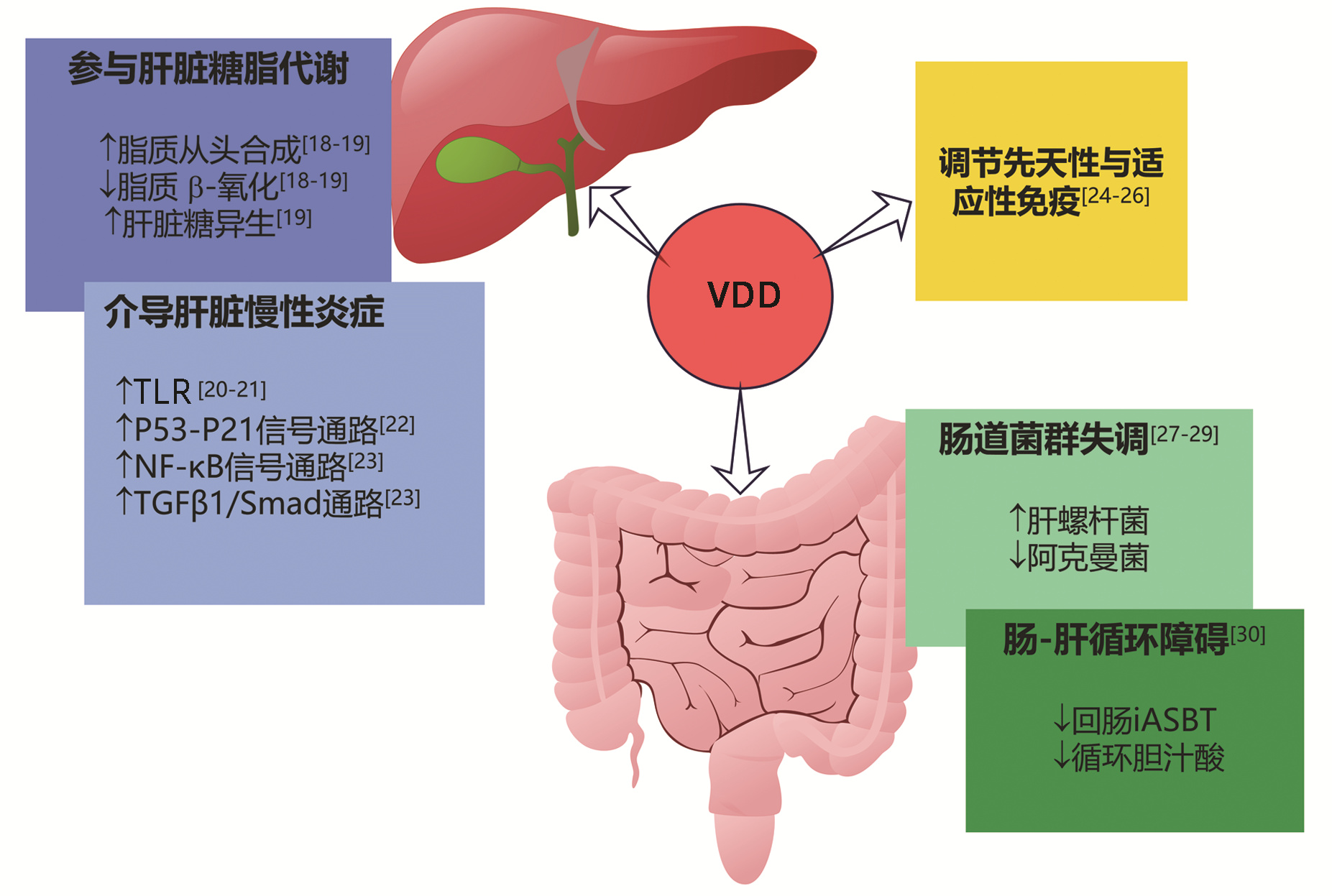
YIN Y, YU Z, XIA M, et al. Vitamin D attenuates high fat diet-induced hepatic steatosis in rats by modulating lipid metabolism[J]. Eur J Clin Invest, 2012, 42(11): 1189-1196. DOI: 10.1111/j.1365-2362.2012.02706.x. |
| [19] |
ELHAFIZ M, ZHAO G, ISMAIL M, et al. Imbalanced insulin substrate-1 and insulin substrate-2 signaling trigger hepatic steatosis in vitamin D deficient rats: 8-methoxypsoralen, a vitamin D receptor ligand with a promising anti-steatotic action[J]. Biochim Biophys Acta Mol Cell Biol Lipids, 2020, 1865(6): 158657. DOI: 10.1016/j.bbalip.2020.158657. |
| [20] |
ROTH CL, ELFERS CT, FIGLEWICZ DP, et al. Vitamin D deficiency in obese rats exacerbates nonalcoholic fatty liver disease and increases hepatic resistin and Toll-like receptor activation[J]. Hepatology, 2012, 55(4): 1103-1111. DOI: 10.1002/hep.24737. |
| [21] |
WANG H, ZHANG Q, CHAI Y, et al. 1, 25(OH) 2D 3 downregulates the Toll-like receptor 4-mediated inflammatory pathway and ameliorates liver injury in diabetic rats[J]. J Endocrinol Invest, 2015, 38(10): 1083-1091. DOI: 10.1007/s40618-015-0287-6. |
| [22] |
MA M, LONG Q, CHEN F, et al. Active vitamin D impedes the progression of non-alcoholic fatty liver disease by inhibiting cell senescence in a rat model[J]. Clin Res Hepatol Gastroenterol, 2020, 44(4): 513-523. DOI: 10.1016/j.clinre.2019.10.007. |
| [23] |
TANG HQ, LI XT, YAN X, et al. Effect of dihydroxyvitamin D3 in regulating NF-κB and TGF-β1/Smad pathway in mice of non-alcoholic steatohepatitis and liver fibrosis[J]. Med J Natl Defend Forces Northwest China, 2016, 37(8): 497-500. DOI: 10.16021/j.cnki.1007-8622.2016.08.003. |
| [24] |
KAMEN DL, TANGPRICHA V. Vitamin D and molecular actions on the immune system: modulation of innate and autoimmunity[J]. J Mol Med (Berl), 2010, 88(5): 441-450. DOI: 10.1007/s00109-010-0590-9. |
| [25] |
LI HJ, HU SL, LIU Y, et al. Correlation between serum 25 hydroxyvitamin D3 level and peripheral blood T lymphocyte subsets in patients with chronic hepatitis B[J]. Clin J Med Offic, 2022, 50(2): 205-207, 210. DOI: 10.16680/j.1671-3826.2022.02.27. |
| [26] |
DRORI A, ROTNEMER-GOLINKIN D, AVNI S, et al. Attenuating the rate of total body fat accumulation and alleviating liver damage by oral administration of vitamin D-enriched edible mushrooms in a diet-induced obesity murine model is mediated by an anti-inflammatory paradigm shift[J]. BMC Gastroenterol, 2017, 17(1): 130. DOI: 10.1186/s12876-017-0688-4. |
| [27] |
|
| [28] |
FAKHOURY H, KVIETYS PR, ALKATTAN W, et al. Vitamin D and intestinal homeostasis: Barrier, microbiota, and immune modulation[J]. J Steroid Biochem Mol Biol, 2020, 200: 105663. DOI: 10.1016/j.jsbmb.2020.105663. |
| [29] |
SU D, NIE Y, ZHU A, et al. Vitamin D signaling through induction of paneth cell defensins maintains gut microbiota and improves metabolic disorders and hepatic steatosis in animal models[J]. Front Physiol, 2016, 7: 498. DOI: 10.3389/fphys.2016.00498. |
| [30] |
KONG M, ZHU L, BAI L, et al. Vitamin D deficiency promotes nonalcoholic steatohepatitis through impaired enterohepatic circulation in animal model[J]. Am J Physiol Gastrointest Liver Physiol, 2014, 307(9): G883-G893. DOI: 10.1152/ajpgi.00427.2013. |
| [31] |
BARCHETTA I, CIMINI FA, CAVALLO MG. Vitamin D and metabolic dysfunction-associated fatty liver disease (MAFLD): An update[J]. Nutrients, 2020, 12(11): 3302. DOI: 10.3390/nu12113302. |
| [32] |
DONG B, ZHOU Y, WANG W, et al. Vitamin D receptor activation in liver macrophages ameliorates hepatic inflammation, steatosis, and insulin resistance in mice[J]. Hepatology, 2020, 71(5): 1559-1574. DOI: 10.1002/hep.30937. |
| [33] |
BOZIC M, GUZMÁN C, BENET M, et al. Hepatocyte vitamin D receptor regulates lipid metabolism and mediates experimental diet-induced steatosis[J]. J Hepatol, 2016, 65(4): 748-757. DOI: 10.1016/j.jhep.2016.05.031. |
| [34] |
BARCHETTA I, CAROTTI S, LABBADIA G, et al. Liver vitamin D receptor, CYP2R1, and CYP27A1 expression: relationship with liver histology and vitamin D 3 levels in patients with nonalcoholic steatohepatitis or hepatitis C virus[J]. Hepatology, 2012, 56(6): 2180-2187. DOI: 10.1002/hep.25930. |
| [35] |
NOBILI V, REIF S. Vitamin D and liver fibrosis: let's start soon before it's too late[J]. Gut, 2015, 64(5): 698-699. DOI: 10.1136/gutjnl-2014-308175. |
| [36] |
GUO XF, WANG C, YANG T, et al. Vitamin D and non-alcoholic fatty liver disease: a meta-analysis of randomized controlled trials[J]. Food Funct, 2020, 11(9): 7389-7399. DOI: 10.1039/d0fo01095b. |
| [37] |
LUKENDA ZANKO V, DOMISLOVIC V, TRKULJA V, et al. Vitamin D for treatment of non-alcoholic fatty liver disease detected by transient elastography: A randomized, double-blind, placebo-controlled trial[J]. Diabetes Obes Metab, 2020, 22(11): 2097-2106. DOI: 10.1111/dom.14129. |
| [38] |
GEIER A, EICHINGER M, STIRNIMANN G, et al. Treatment of non-alcoholic steatohepatitis patients with vitamin D: a double-blinded, randomized, placebo-controlled pilot study[J]. Scand J Gastroenterol, 2018, 53(9): 1114-1120. DOI: 10.1080/00365521.2018.1501091. |
| [39] |
DASARATHY J, VARGHESE R, FELDMAN A, et al. Patients with nonalcoholic fatty liver disease have a low response rate to vitamin D supplementation[J]. J Nutr, 2017, 147(10): 1938-1946. DOI: 10.3945/jn.117.254292. |
| [40] |
TABRIZI R, MOOSAZADEH M, LANKARANI KB, et al. The effects of vitamin D supplementation on metabolic profiles and liver function in patients with non-alcoholic fatty liver disease: A systematic review and meta-analysis of randomized controlled trials[J]. Diabetes Metab Syndr, 2017, 11(Suppl 2): S975-S982. DOI: 10.1016/j.dsx.2017.07.025. |
| [41] |
DABBAGHMANESH MH, DANAFAR F, ESHRAGHIAN A, et al. Vitamin D supplementation for the treatment of non-alcoholic fatty liver disease: A randomized double blind placebo controlled trial[J]. Diabetes Metab Syndr, 2018, 12(4): 513-517. DOI: 10.1016/j.dsx.2018.03.006. |
| [42] |
BOUCHER BJ. Why do so many trials of vitamin D supplementation fail?[J]. Endocr Connect, 2020, 9(9): R195-R206. DOI: 10.1530/EC-20-0274. |
| [43] |
EL-SHERBINY M, ELDOSOKY M, EL-SHAFEY M, et al. Vitamin D nanoemulsion enhances hepatoprotective effect of conventional vitamin D in rats fed with a high-fat diet[J]. Chem Biol Interact, 2018, 288: 65-75. DOI: 10.1016/j.cbi.2018.04.010. |
| [44] |
NAKANO T, CHENG YF, LAI CY, et al. Impact of artificial sunlight therapy on the progress of non-alcoholic fatty liver disease in rats[J]. J Hepatol, 2011, 55(2): 415-425. DOI: 10.1016/j.jhep.2010.11.028. |
| [45] |
LUGER M, KRUSCHITZ R, KIENBACHER C, et al. Vitamin D 3 loading is superior to conventional supplementation after weight loss surgery in vitamin D-deficient morbidly obese patients: A double-blind randomized placebo-controlled trial[J]. Obes Surg, 2017, 27(5): 1196-1207. DOI: 10.1007/s11695-016-2437-0. |







 DownLoad:
DownLoad: