| [1] |
PINTER M, SCHEINER B, PECK-RADOSAVLJEVIC M. Immunotherapy for advanced hepatocellular carcinoma: a focus on special subgroups[J]. Gut, 2021, 70(1): 204-214. DOI: 10.1136/gutjnl-2020-321702. |
| [2] |
FANG CH, CAI W. Application of artificial intelligence in the diagnosis and treatment of primary liver cancer[J]. J Clin Hepatol, 2022, 38(1): 26-29. DOI: 10.3969/j.issn.1001-5256.2022.01.004. |
| [3] |
FINN RS, QIN S, IKEDA M, et al. Atezolizumab plus Bevacizumab in unresectable hepatocellular carcinoma[J]. N Engl J Med, 2020, 382(20): 1894-1905. DOI: 10.1056/NEJMoa1915745. |
| [4] |
RIZVI S, WANG J, EL-KHOUEIRY AB. Liver cancer immunity[J]. Hepatology, 2021, 73(Suppl 1): 86-103. DOI: 10.1002/hep.31416. |
| [5] |
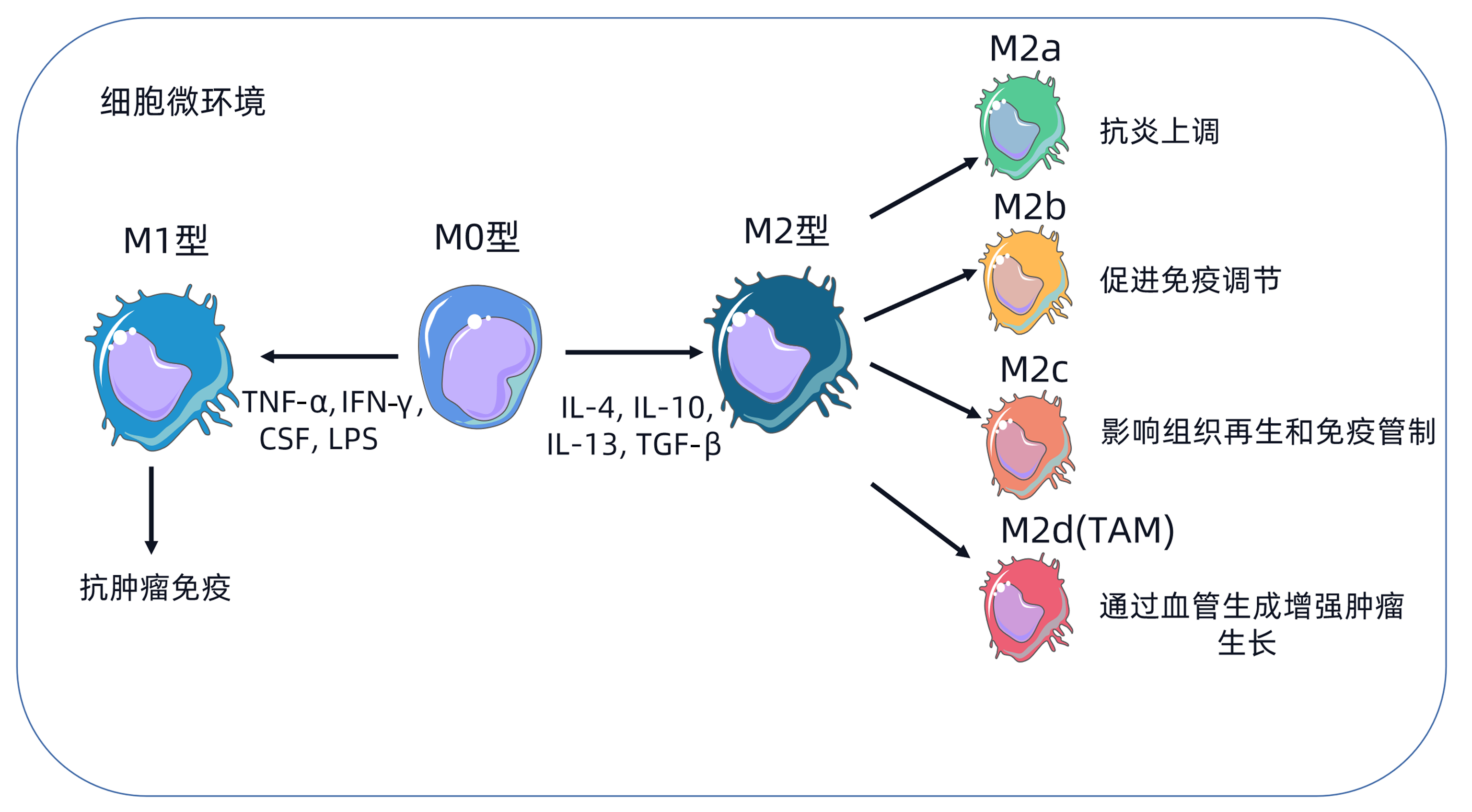
RITZ T, KRENKEL O, TACKE F. Dynamic plasticity of macrophage functions in diseased liver[J]. Cell Immunol, 2018, 330: 175-182. DOI: 10.1016/j.cellimm.2017.12.007. |
| [6] |
ESHGHJOO S, KIM DM, JAYARAMAN A, et al. Macrophage polarization in atherosclerosis[J]. Genes (Basel), 2022, 13(5): 756. DOI: 10.3390/genes13050756. |
| [7] |
ANDERSON NR, MINUTOLO NG, GILL S, et al. Macrophage-based approaches for cancer immunotherapy[J]. Cancer Res, 2021, 81(5): 1201-1208. DOI: 10.1158/0008-5472.CAN-20-2990. |
| [8] |
SHAPOURI-MOGHADDAM A, MOHAMMADIAN S, VAZINI H, et al. Macrophage plasticity, polarization, and function in health and disease[J]. J Cell Physiol, 2018, 233(9): 6425-6440. DOI: 10.1002/jcp.26429. |
| [9] |
OSIPOV A, MURPHY A, ZHENG L. From immune checkpoints to vaccines: The past, present and future of cancer immunotherapy[J]. Adv Cancer Res, 2019, 143: 63-144. DOI: 10.1016/bs.acr.2019.03.002. |
| [10] |
REICHEL D, TRIPATHI M, PEREZ JM. Biological effects of nanoparticles on macrophage polarization in the tumor microenvironment[J]. Nanotheranostics, 2019, 3(1): 66-88. DOI: 10.7150/ntno.30052. |
| [11] |
XIANG W, SHI R, KANG X, et al. Monoacylglycerol lipase regulates cannabinoid receptor 2-dependent macrophage activation and cancer progression[J]. Nat Commun, 2018, 9(1): 2574. DOI: 10.1038/s41467-018-04999-8. |
| [12] |
HAM S, LIMA LG, LEK E, et al. The impact of the cancer microenvironment on macrophage phenotypes[J]. Front Immunol, 2020, 11: 1308. DOI: 10.3389/fimmu.2020.01308. |
| [13] |
MEI J, XIAO Z, GUO C, et al. Prognostic impact of tumor-associated macrophage infiltration in non-small cell lung cancer: A systemic review and meta-analysis[J]. Oncotarget, 2016, 7(23): 34217-34228. DOI: 10.18632/oncotarget.9079. |
| [14] |
CHEN Y, SONG Y, DU W, et al. Tumor-associated macrophages: an accomplice in solid tumor progression[J]. J Biomed Sci, 2019, 26(1): 78. DOI: 10.1186/s12929-019-0568-z. |
| [15] |
BOHN T, RAPP S, LUTHER N, et al. Tumor immunoevasion via acidosis-dependent induction of regulatory tumor-associated macrophages[J]. Nat Immunol, 2018, 19(12): 1319-1329. DOI: 10.1038/s41590-018-0226-8. |
| [16] |
YANG Y, YE YC, CHEN Y, et al. Crosstalk between hepatic tumor cells and macrophages via Wnt/β-catenin signaling promotes M2-like macrophage polarization and reinforces tumor malignant behaviors[J]. Cell Death Dis, 2018, 9(8): 793. DOI: 10.1038/s41419-018-0818-0. |
| [17] |
CHEN MM, XIAO X, LAO XM, et al. Polarization of tissue-resident TFH-like cells in human hepatoma bridges innate monocyte inflammation and M2b macrophage polarization[J]. Cancer Discov, 2016, 6(10): 1182-1195. DOI: 10.1158/2159-8290.CD-16-0329. |
| [18] |
ZHANG YL, LI Q, YANG XM, et al. SPON2 promotes M1-like macrophage recruitment and inhibits hepatocellular carcinoma metastasis by distinct integrin-Rho GTPase-Hippo pathways[J]. Cancer Res, 2018, 78(9): 2305-2317. DOI: 10.1158/0008-5472.CAN-17-2867. |
| [19] |
LIU N, WANG X, STEER CJ, et al. MicroRNA-206 promotes the recruitment of CD8 + T cells by driving M1 polarisation of Kupffer cells[J]. Gut, 2022, 71(8): 1642-1655. DOI: 10.1136/gutjnl-2021-324170. |
| [20] |
XU J, LIN H, WU G, et al. IL-6/STAT3 is a promising therapeutic target for hepatocellular carcinoma[J]. Front Oncol, 2021, 11: 760971. DOI: 10.3389/fonc.2021.760971. |
| [21] |
WANG TT, YUAN JH, MA JZ, et al. CTGF secreted by mesenchymal-like hepatocellular carcinoma cells plays a role in the polarization of macrophages in hepatocellular carcinoma progression[J]. Biomed Pharmacother, 2017, 95: 111-119. DOI: 10.1016/j.biopha.2017.08.004. |
| [22] |
SUN Y, WU L, ZHONG Y, et al. Single-cell landscape of the ecosystem in early-relapse hepatocellular carcinoma[J]. Cell, 2021, 184(2): 404-421. DOI: 10.1016/j.cell.2020.11.041. |
| [23] |
LI X, YAO W, YUAN Y, et al. Targeting of tumour-infiltrating macrophages via CCL2/CCR2 signalling as a therapeutic strategy against hepatocellular carcinoma[J]. Gut, 2017, 66(1): 157-167. DOI: 10.1136/gutjnl-2015-310514. |
| [24] |
LI X, CHEN L, PENG X, et al. Progress of tumor-associated macrophages in the epithelial-mesenchymal transition of tumor[J]. Front Oncol, 2022, 12: 911410. DOI: 10.3389/fonc.2022.911410. |
| [25] |
GUO B, LI L, GUO J, et al. M2 tumor-associated macrophages produce interleukin-17 to suppress oxaliplatin-induced apoptosis in hepatocellular carcinoma[J]. Oncotarget, 2017, 8(27): 44465-44476. DOI: 10.18632/oncotarget.17973. |
| [26] |
WEI Y, SHI D, LIANG Z, et al. IL-17A secreted from lymphatic endothelial cells promotes tumorigenesis by upregulation of PD-L1 in hepatoma stem cells[J]. J Hepatol, 2019, 71(6): 1206-1215. DOI: 10.1016/j.jhep.2019.08.034. |
| [27] |
SIA D, JIAO Y, MARTINEZ-QUETGLAS I, et al. Identification of an immune-specific class of hepatocellular carcinoma, based on molecular features[J]. Gastroenterology, 2017, 153(3): 812-826. DOI: 10.1053/j.gastro.2017.06.007. |
| [28] |
KE M, ZHANG Z, CONG L, et al. MicroRNA-148b-colony-stimulating factor-1 signaling-induced tumor-associated macrophage infiltration promotes hepatocellular carcinoma metastasis[J]. Biomed Pharmacother, 2019, 120: 109523. DOI: 10.1016/j.biopha.2019.109523. |
| [29] |
LI Z, LI H, ZHAO ZB, et al. SIRT4 silencing in tumor-associated macrophages promotes HCC development via PPARδ signalling-mediated alternative activation of macrophages[J]. J Exp Clin Cancer Res, 2019, 38(1): 469. DOI: 10.1186/s13046-019-1456-9. |
| [30] |
PU Z, DUDA DG, ZHU Y, et al. VCP interaction with HMGB1 promotes hepatocellular carcinoma progression by activating the PI3K/AKT/mTOR pathway[J]. J Transl Med, 2022, 20(1): 212. DOI: 10.1186/s12967-022-03416-5. |
| [31] |
DEBACKER JM, GONDRY O, LAHOUTTE T, et al. The prognostic value of CD206 in solid malignancies: A systematic review and meta-analysis[J]. Cancers (Basel), 2021, 13(14): 3422. DOI: 10.3390/cancers13143422. |
| [32] |
WU X, LUO H, SHI B, et al. Combined antitumor effects of sorafenib and GPC3-CAR T cells in mouse models of hepatocellular carcinoma[J]. Mol Ther, 2019, 27(8): 1483-1494. DOI: 10.1016/j.ymthe.2019.04.020. |
| [33] |
CHEN R, LI Q, XU S, et al. Modulation of the tumour microenvironment in hepatocellular carcinoma by tyrosine kinase inhibitors: from modulation to combination therapy targeting the microenvironment[J]. Cancer Cell Int, 2022, 22(1): 73. DOI: 10.1186/s12935-021-02435-4. |
| [34] |
LEE TK, GUAN XY, MA S. Cancer stem cells in hepatocellular carcinoma - from origin to clinical implications[J]. Nat Rev Gastroenterol Hepatol, 2022, 19(1): 26-44. DOI: 10.1038/s41575-021-00508-3. |
| [35] |
YIN Z, MA T, LIN Y, et al. IL-6/STAT3 pathway intermediates M1/M2 macrophage polarization during the development of hepatocellular carcinoma[J]. J Cell Biochem, 2018, 119(11): 9419-9432. DOI: 10.1002/jcb.27259. |
| [36] |
ZHONG CQ, ZHANG XP, MA N, et al. FABP4 suppresses proliferation and invasion of hepatocellular carcinoma cells and predicts a poor prognosis for hepatocellular carcinoma[J]. Cancer Med, 2018, 7(6): 2629-2640. DOI: 10.1002/cam4.1511. |
| [37] |
XUE ST, LI K, GAO Y, et al. The role of the key autophagy kinase ULK1 in hepatocellular carcinoma and its validation as a treatment target[J]. Autophagy, 2020, 16(10): 1823-1837. DOI: 10.1080/15548627.2019.1709762. |
| [38] |
LIU LZ, ZHANG Z, ZHENG BH, et al. CCL15 recruits suppressive monocytes to facilitate immune escape and disease progression in hepatocellular carcinoma[J]. Hepatology, 2019, 69(1): 143-159. DOI: 10.1002/hep.30134. |
| [39] |
LIU C, CHIKINA M, DESHPANDE R, et al. Treg cells promote the SREBP1-dependent metabolic fitness of tumor-promoting macrophages via repression of CD8 + T cell-derived interferon-γ[J]. Immunity, 2019, 51(2): 381-397. DOI: 10.1016/j.immuni.2019.06.017. |
| [40] |
SUNG PS, YOON SK, JANG JW, et al. Inflammation-induced IgA plus tumor-associated macrophages express PD-L1 and causes impaired T cell functionality in hepatocellular carcinoma[J]. Hepatology, 2020, 72(Suppl 1): 780A-781A.
|
| [41] |
HSU BE, ROY J, MOUHANNA J, et al. C3a elicits unique migratory responses in immature low-density neutrophils[J]. Oncogene, 2020, 39(12): 2612-2623. DOI: 10.1038/s41388-020-1169-8. |
| [42] |
ZHOU Z, WANG P, SUN R, et al. Tumor-associated neutrophils and macrophages interaction contributes to intrahepatic cholangiocarcinoma progression by activating STAT3[J]. J Immunother Cancer, 2021, 9(3): e001946. DOI: 10.1136/jitc-2020-001946. |
| [43] |
PENG ZP, JIANG ZZ, GUO HF, et al. Glycolytic activation of monocytes regulates the accumulation and function of neutrophils in human hepatocellular carcinoma[J]. J Hepatol, 2020, 73(4): 906-917. DOI: 10.1016/j.jhep.2020.05.004. |
| [44] |
ZHOU SL, DAI Z, ZHOU ZJ, et al. Overexpression of CXCL5 mediates neutrophil infiltration and indicates poor prognosis for hepatocellular carcinoma[J]. Hepatology, 2012, 56(6): 2242-2254. DOI: 10.1002/hep.25907. |
| [45] |
WU G, MA Z, CHENG Y, et al. Targeting Gas6/TAM in cancer cells and tumor microenvironment[J]. Mol Cancer, 2018, 17(1): 20. DOI: 10.1186/s12943-018-0769-1. |
| [46] |
YANG F, WEI Y, HAN D, et al. Interaction with CD68 and regulation of GAS6 expression by endosialin in fibroblasts drives recruitment and polarization of macrophages in hepatocellular carcinoma[J]. Cancer Res, 2020, 80(18): 3892-3905. DOI: 10.1158/0008-5472. |






 DownLoad:
DownLoad:
