| [1] |
KLEIN AP. Pancreatic cancer epidemiology: Understanding the role of lifestyle and inherited risk factors[J]. Nat Rev Gastroenterol Hepatol, 2021, 18( 7): 493- 502. DOI: 10.1038/s41575-021-00457-x. |
| [2] |
RAHIB L, SMITH BD, AIZENBERG R, et al. Projecting cancer incidence and deaths to 2030: The unexpected burden of thyroid, liver, and pancreas cancers in the United States[J]. Cancer Res, 2014, 74( 11): 2913- 2921. DOI: 10.1158/0008-5472.CAN-14-0155. |
| [3] |
HALBROOK CJ, LYSSIOTIS CA, PASCA DI MAGLIANO M, et al. Pancreatic cancer: Advances and challenges[J]. Cell, 2023, 186( 8): 1729- 1754. DOI: 10.1016/j.cell.2023.02.014. |
| [4] |
GE WY, WANG HX. Immunotherapy for pancreatic ductal adenocarcinoma: Challenges and opportunities[J]. J Clin Hepatol, 2019, 35( 5): 958- 963. DOI: 10.3969/j.issn.1001-5256.2019.05.005. |
| [5] |
KLEEFF J, KORC M, APTE M, et al. Pancreatic cancer[J]. Nat Rev Dis Primers, 2016, 2: 16022. DOI: 10.1038/nrdp.2016.22. |
| [6] |
HE J, AHUJA N, MAKARY MA, et al. 2564 resected periampullary adenocarcinomas at a single institution: Trends over three decades[J]. HPB, 2014, 16( 1): 83- 90. DOI: 10.1111/hpb.12078. |
| [7] |
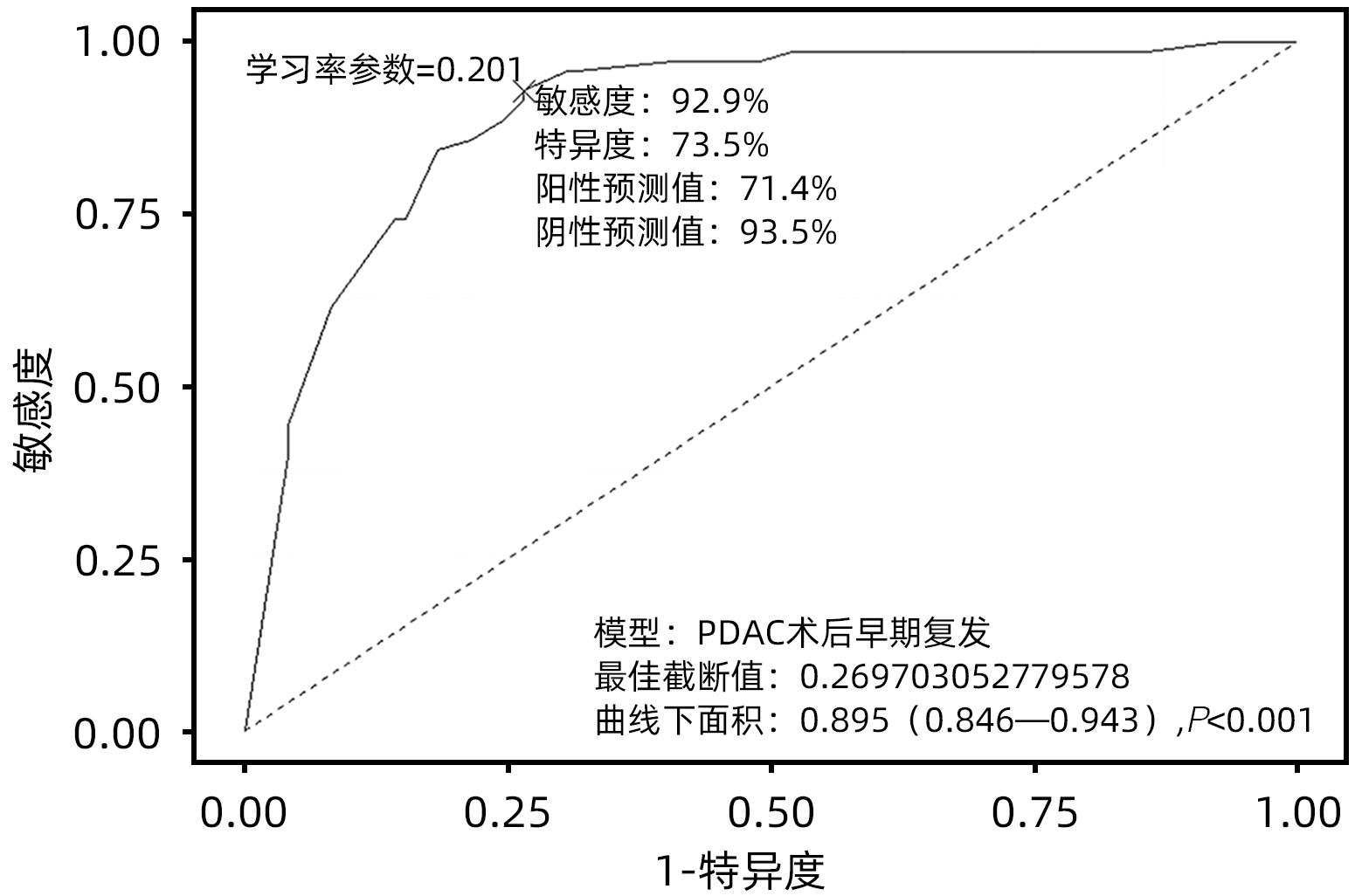
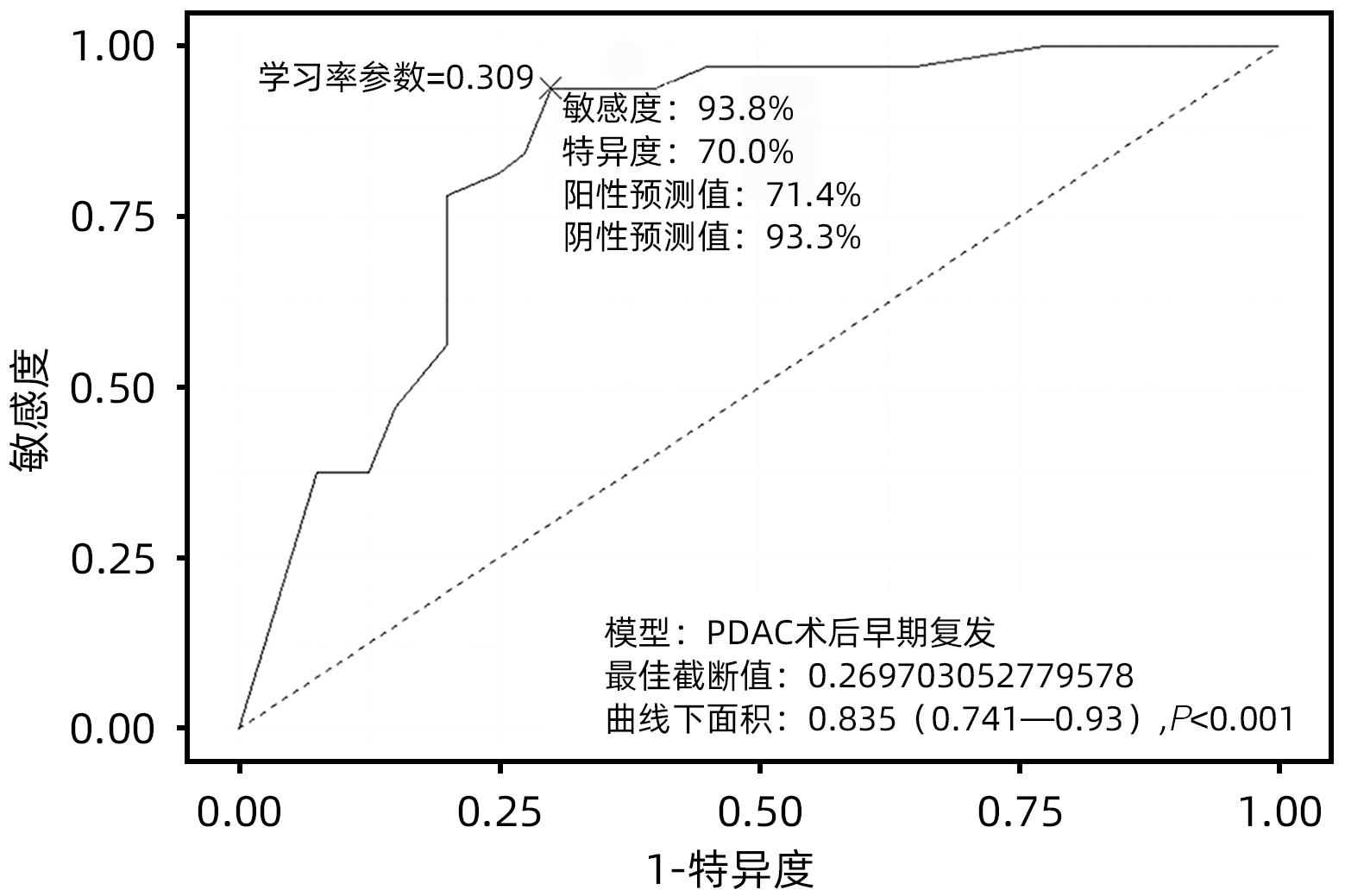
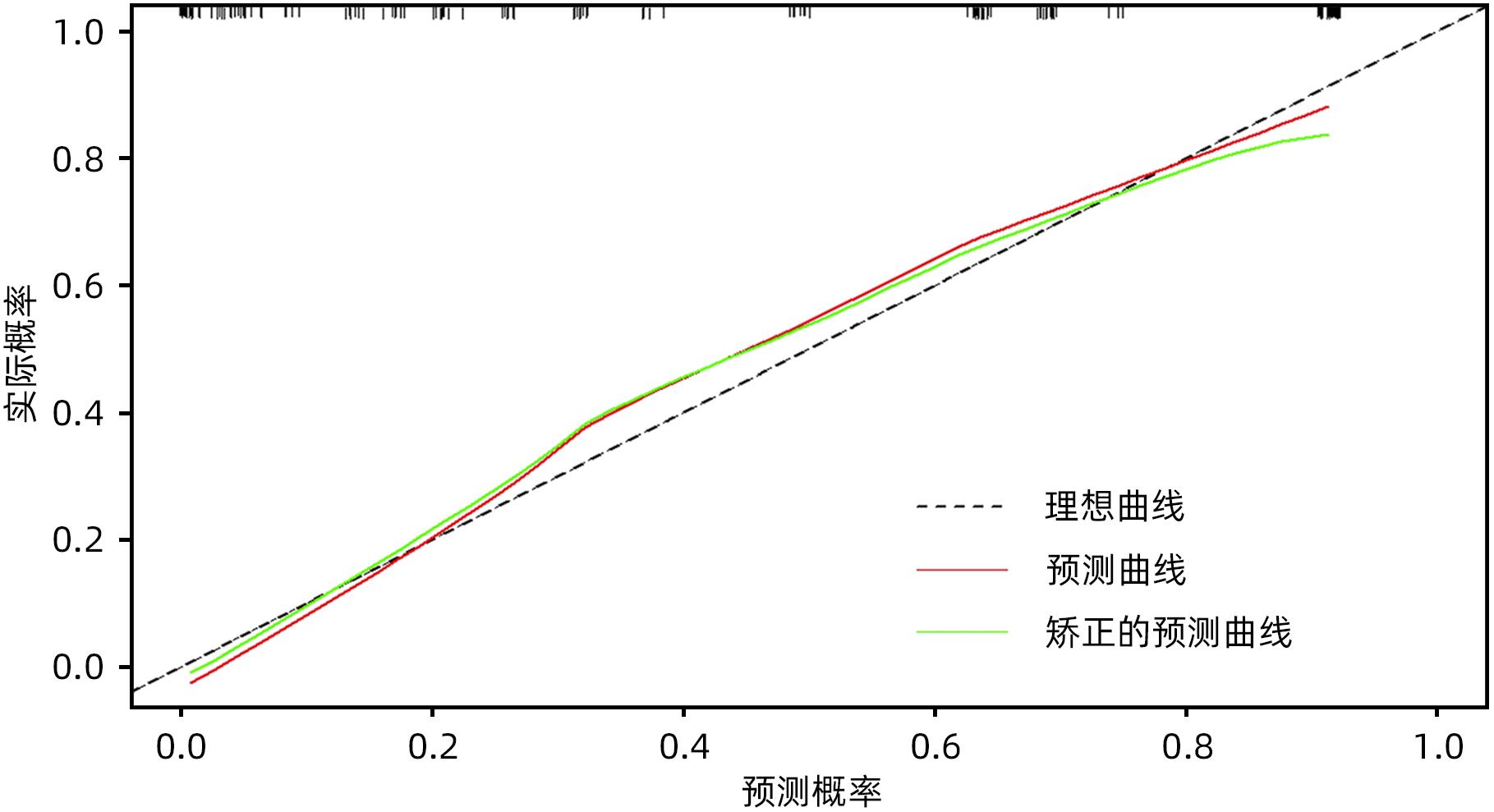
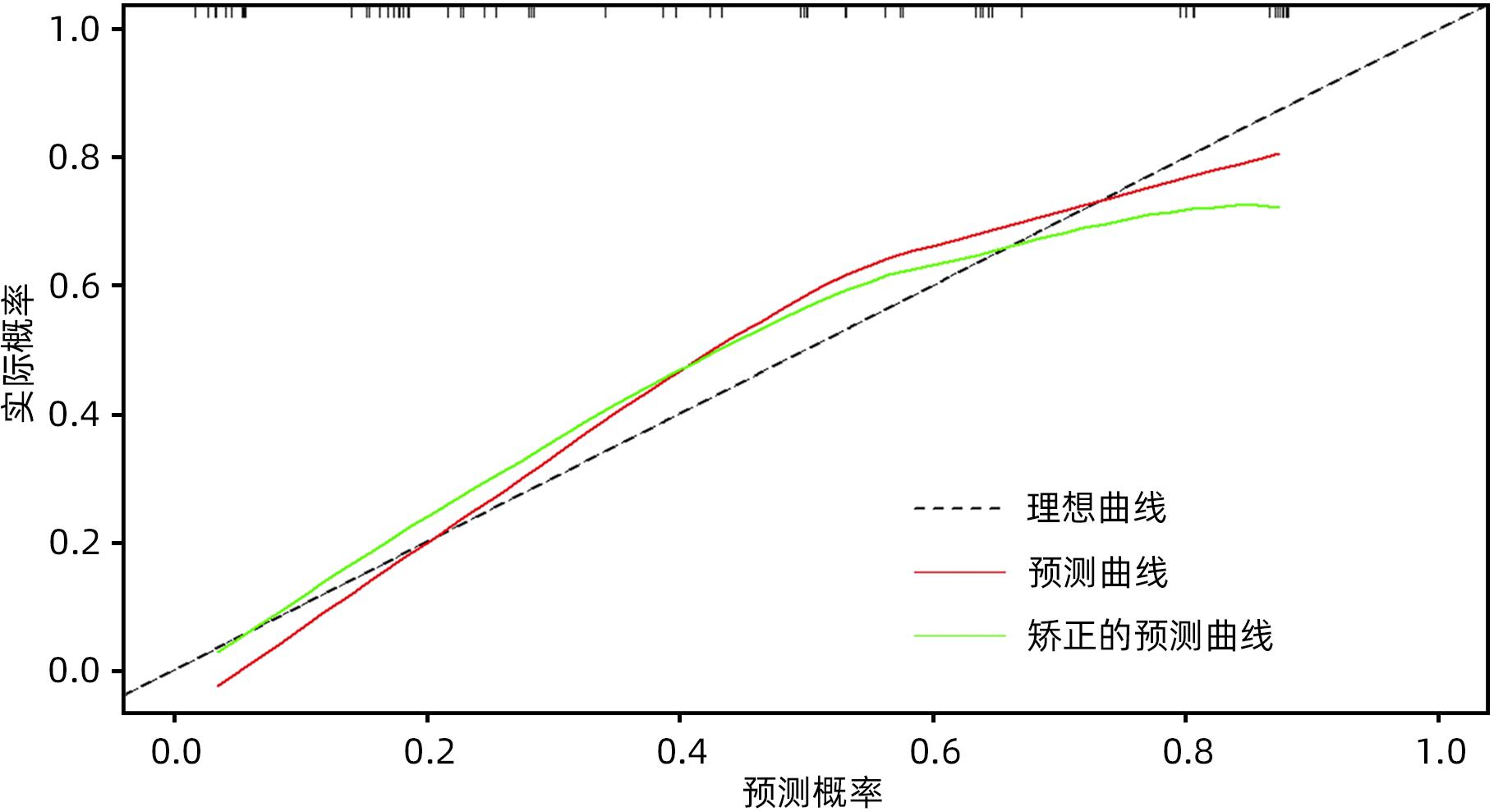
ZHANG XP, XU S, GAO YX, et al. Early and late recurrence patterns of pancreatic ductal adenocarcinoma after pancreaticoduodenectomy: A multicenter study[J]. Int J Surg, 2023, 109( 4): 785- 793. DOI: 10.1097/JS9.0000000000000296. |
| [8] |
JONES RP, PSARELLI EE, JACKSON R, et al. Patterns of recurrence after resection of pancreatic ductal adenocarcinoma: A secondary analysis of the ESPAC-4 randomized adjuvant chemotherapy trial[J]. JAMA Surg, 2019, 154( 11): 1038- 1048. DOI: 10.1001/jamasurg.2019.3337. |
| [9] |
GROOT VP, REZAEE N, WU WC, et al. Patterns, timing, and predictors of recurrence following pancreatectomy for pancreatic ductal adenocarcinoma[J]. Ann Surg, 2018, 267( 5): 936- 945. DOI: 10.1097/SLA.0000000000002234. |
| [10] |
GROOT VP, GEMENETZIS G, BLAIR AB, et al. Implications of the pattern of disease recurrence on survival following pancreatectomy for pancreatic ductal adenocarcinoma[J]. Ann Surg Oncol, 2018, 25( 8): 2475- 2483. DOI: 10.1245/s10434-018-6558-7. |
| [11] |
TEMPERO MA, MALAFA MP, AL-HAWARY M, et al. Pancreatic adenocarcinoma, version 2.2021, NCCN clinical practice guidelines in oncology[J]. J Natl Compr Canc Netw, 2021, 19( 4): 439- 457. DOI: 10.6004/jnccn.2021.0017. |
| [12] |
WANG SP, LIU SY, ZHANG W, et al. The value of“posterior approach, uncinate process priority, artery first” in laparoscopic pancreatoduodenectomy[J]. Natl Med J China, 2020, 100( 42): 3328- 3331. DOI: 10.3760/cma.j.cn112137-20200316-00789 |
| [13] |
WENTE MN, VEIT JA, BASSI C, et al. Postpancreatectomy hemorrhage(PPH): An International Study Group of Pancreatic Surgery(ISGPS) definition[J]. Surgery, 2007, 142( 1): 20- 25. DOI: 10.1016/j.surg.2007.02.001. |
| [14] |
BASSI C, MARCHEGIANI G, DERVENIS C, et al. The 2016 update of the International Study Group(ISGPS) definition and grading of postoperative pancreatic fistula: 11 Years After[J]. Surgery, 2017, 161( 3): 584- 591. DOI: 10.1016/j.surg.2016.11.014. |
| [15] |
KOCH M, GARDEN OJ, PADBURY R, et al. Bile leakage after hepatobiliary and pancreatic surgery: A definition and grading of severity by the International Study Group of Liver Surgery[J]. Surgery, 2011, 149( 5): 680- 688. DOI: 10.1016/j.surg.2010.12.002. |
| [16] |
Study Group of Pancreatic Surgery in Chinese Society of Surgery of Chinese Medical Association, Pancreatic Disease Committee of Chinese Research Hospital Association, Editorial Board of Chinese Journal of Surgery. A consensus statement on the diagnosis, treatment, and prevention of common complications after pancreatic surgery(2017)[J]. Chin J Surg, 2017, 55( 5): 328- 334. DOI: 10.3760/cma.j.issn.0529-5815.2017.05.003. |
| [17] |
LOU WH, LIU YB, LIANG TB, et al. Expert consensus on diagnosis, treatment and prevention of common complications after pancreatic surgery(2017)[J]. Med J Peking Union Med Coll Hosp, 2017, 8( S1): 139- 146.
楼文晖, 刘颖斌, 梁廷波, 等. 胰腺术后外科常见并发症诊治及预防的专家共识(2017)[J]. 协和医学杂志, 2017, 8( S1): 139- 146.
|
| [18] |
|
| [19] |
BULDANLI MZ, UÇANER B, ÇIFTÇI MS, et al. Laparoscopic Nissen fundoplication: A five-year single-center clinical experience and results[J]. Eur Rev Med Pharmacol Sci, 2023, 27( 4): 1346- 1351. DOI: 10.26355/eurrev_202302_31368. |
| [20] |
BURASAKARN P, THIENHIRAN A, FUENGFOO P, et al. Analysis of preoperative risk factors for early recurrence after curative pancreatoduodenectomy for resectable pancreatic adenocarcinoma[J]. Innov Surg Sci, 2022, 7( 1): 5- 11. DOI: 10.1515/iss-2021-0034. |
| [21] |
DAAMEN LA, DORLAND G, BRADA LJH, et al. Preoperative predictors for early and very early disease recurrence in patients undergoing resection of pancreatic ductal adenocarcinoma[J]. HPB, 2022, 24( 4): 535- 546. DOI: 10.1016/j.hpb.2021.09.004. |
| [22] |
MATSUMOTO I, MURAKAMI Y, SHINZEKI M, et al. Proposed preoperative risk factors for early recurrence in patients with resectable pancreatic ductal adenocarcinoma after surgical resection: A multi-center retrospective study[J]. Pancreatology, 2015, 15( 6): 674- 680. DOI: 10.1016/j.pan.2015.09.008. |
| [23] |
GROOT VP, GEMENETZIS G, BLAIR AB, et al. Defining and predicting early recurrence in 957 patients with resected pancreatic ductal adenocarcinoma[J]. Ann Surg, 2019, 269( 6): 1154- 1162. DOI: 10.1097/SLA.0000000000002734. |
| [24] |
IMAMURA M, NAGAYAMA M, KYUNO D, et al. Perioperative predictors of early recurrence for resectable and borderline-resectable pancreatic cancer[J]. Cancers, 2021, 13( 10): 2285. DOI: 10.3390/cancers13102285. |
| [25] |
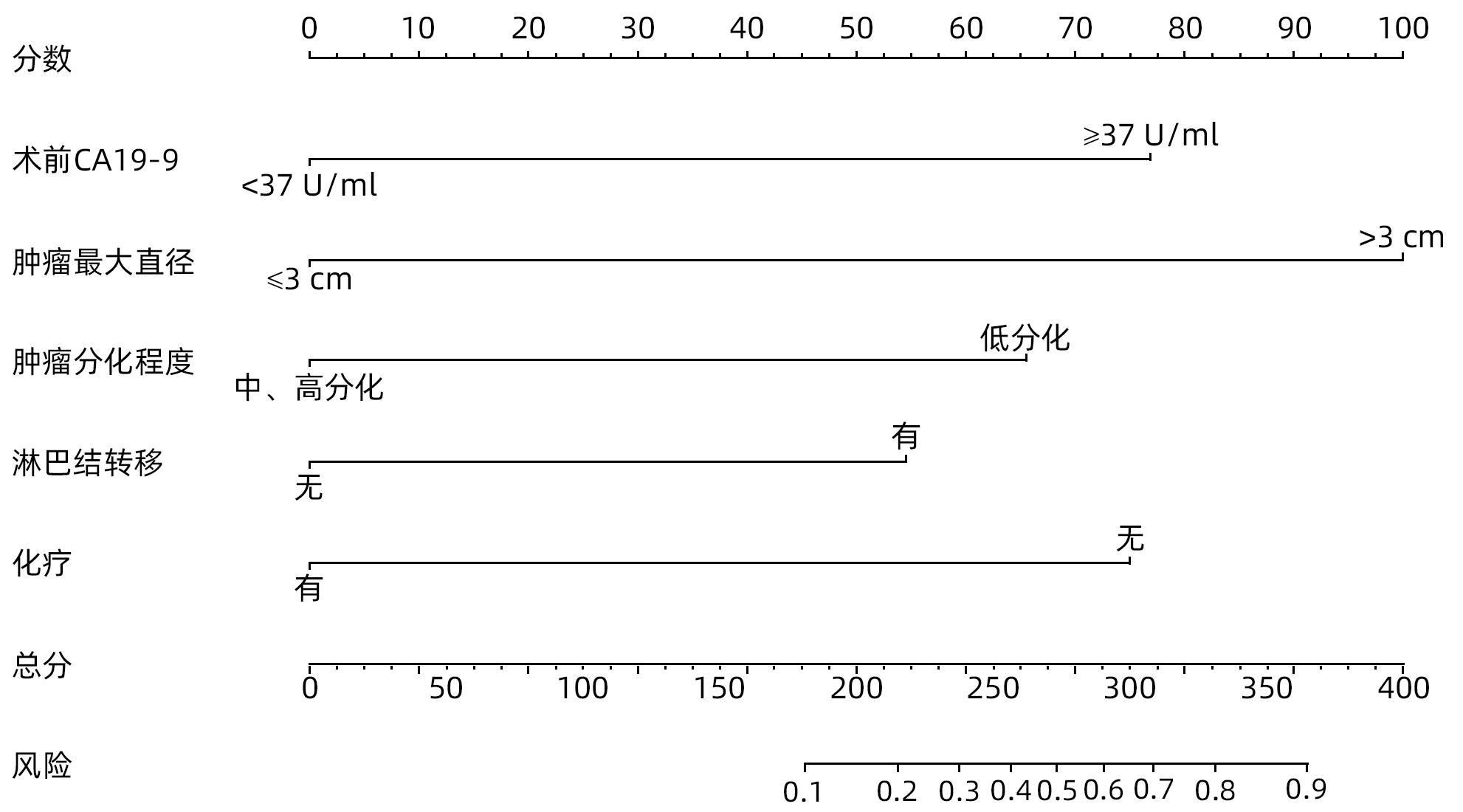
WANG YW, CUI CH, LI MT, et al. Construction and validation of a nomogram prediction model for early recurrence of patients undergoing radical pancreaticoduodenectomy for pancreatic ductal adenocarcinoma[J]. Chin J Hepatobiliary Surg, 2023, 29( 7): 538- 543. DOI: 10.3760/cma.j.cn113884-20221028-00404 |
| [26] |
SIEGEL RL, MILLER KD, JEMAL A. Cancer statistics, 2016[J]. CA Cancer J Clin, 2016, 66( 1): 7- 30. DOI: 10.3322/caac.21332. |
| [27] |
MA YS, YANG YM. An excerpt of pancreatic cancer: French clinical practice guidelines for diagnosis, treatment and follow-up(2018)[J]. J Clin Hepatol, 2019, 35( 1): 67- 71. DOI: 10.3969/j.issn.1001-5256.2019.01.012 |
| [28] |
CHEN RF, ZHONG CR, ZHOU QB. Current status and perspectives of minimally invasive surgical treatment of pancreatic head carcinoma[J]. J Clin Hepatol, 2019, 35( 5): 953- 957. DOI: 10.3969/j.issn.1001-5256.2019.05.004. |
| [29] |
CHOI SH, KIM HY, HWANG HK, et al. Oncologic impact of local recurrence in resected pancreatic cancer and topographic preference in local recurrence patterns according to tumor location[J]. Pancreas, 2020, 49( 10): 1290- 1296. DOI: 10.1097/MPA.0000000000001679. |
| [30] |
ZHANG TP, LIU YZ, REN B. Current status and challenges of total neoadjuvant therapy for pancreatic cancer[J]. Chin J Dig Surg, 2022, 21( 4): 461- 464. DOI: 10.3760/cma.j.cn115610-20220320-00141. |
| [31] |
ZHU LX, MAO L, DU J, et al. Clinical efficacy of radical resection of pancreatic cancer after neoadjuvant conversion therapy[J]. Chin J Dig Surg, 2023, 22( 7): 916- 923. DOI: 10.3760/cma.j.cn115610-20230512-00204. |
| [32] |
LUO GP, JIN KZ, DENG SM, et al. Roles of CA19-9 in pancreatic cancer: Biomarker, predictor and promoter[J]. Biochim Biophys Acta Rev Cancer, 2021, 1875( 2): 188409. DOI: 10.1016/j.bbcan.2020.188409. |
| [33] |
MAHAJAN UM, OEHRLE B, SIRTL S, et al. Independent validation and assay standardization of improved metabolic biomarker signature to differentiate pancreatic ductal adenocarcinoma from chronic pancreatitis[J]. Gastroenterology, 2022, 163( 5): 1407- 1422. DOI: 10.1053/j.gastro.2022.07.047. |
| [34] |
ZHANG XP, GAO YX, XU S, et al. A novel online calculator to predict early recurrence and long-term survival of patients with resectable pancreatic ductal adenocarcinoma after pancreaticoduodenectomy: A multicenter study[J]. Int J Surg, 2022, 106: 106891. DOI: 10.1016/j.ijsu.2022.106891. |
| [35] |
XU S, ZHANG XP, ZHAO GD, et al. Development and validation of an online calculator to predict early recurrence and long-term survival in patients with distal cholangiocarcinoma after pancreaticoduodenectomy[J]. J Hepatobiliary Pancreat Sci, 2022, 29( 11): 1214- 1225. DOI: 10.1002/jhbp.1058. |
| [36] |
CAPELLO M, BANTIS LE, SCELO G, et al. Sequential validation of blood-based protein biomarker candidates for early-stage pancreatic cancer[J]. J Natl Cancer Inst, 2017, 109( 4): djw266. DOI: 10.1093/jnci/djw266. |
| [37] |
AZIZIAN A, RÜHLMANN F, KRAUSE T, et al. CA19-9 for detecting recurrence of pancreatic cancer[J]. Sci Rep, 2020, 10( 1): 1332. DOI: 10.1038/s41598-020-57930-x. |
| [38] |
YOKOYAMA S, HAMADA T, HIGASHI M, et al. Predicted prognosis of patients with pancreatic cancer by machine learning[J]. Clin Cancer Res, 2020, 26( 10): 2411- 2421. DOI: 10.1158/1078-0432.CCR-19-1247. |
| [39] |
ZHAO TS, XIAO D, JIN FJ, et al. ESE3-positive PSCs drive pancreatic cancer fibrosis, chemoresistance and poor prognosis via tumour-stromal IL-1β/NF-κB/ESE3 signalling axis[J]. Br J Cancer, 2022, 127( 8): 1461- 1472. DOI: 10.1038/s41416-022-01927-y. |
| [40] |
OVERBEEK KA, GOGGINS MG, DBOUK M, et al. Timeline of development of pancreatic cancer and implications for successful early detection in high-risk individuals[J]. Gastroenterology, 2022, 162( 3): 772- 785.e4. DOI: 10.1053/j.gastro.2021.10.014. |
| [41] |
HEID I, STEIGER K, TRAJKOVIC-ARSIC M, et al. Co-clinical assessment of tumor cellularity in pancreatic cancer[J]. Clin Cancer Res, 2017, 23( 6): 1461- 1470. DOI: 10.1158/1078-0432.CCR-15-2432. |
| [42] |
YOU MS, LEE SH, CHOI YH, et al. Lymph node ratio as valuable predictor in pancreatic cancer treated with R0 resection and adjuvant treatment[J]. BMC Cancer, 2019, 19( 1): 952. DOI: 10.1186/s12885-019-6193-0. |
| [43] |
JAMG TOL, GOUMA DJ, BASSI C, et al. Definition of a standard lymphadenectomy in surgery for pancreatic ductal adenocarcinoma: A consensus statement by the International Study Group on Pancreatic Surgery(ISGPS)[J]. Surgery, 2014, 156( 3): 591- 600. DOI: 10.1016/j.surg.2014.06.016. |
| [44] |
General Office of National Health Commission. Standard for diagnosis and treatment of pancreatic cancer(2022 edition)[J]. J Clin Hepatol, 2022, 38( 5): 1006- 1015. DOI: 10.3969/j.issn.1001-5256.2022.05.007. |
| [45] |
Chinese Pancreatic Surgery Association, Chinese Society of Surgery, Chinese Medical Association. Guidelines for the diagnosis and treatment of pancreatic cancer in China(2021)[J]. Chin J Pract Surg, 2021, 41( 7): 725- 738. DOI: 10.19538/j.cjps.issn1005-2208.2021.07.02. |






 DownLoad:
DownLoad: