| [1] |
RUMGAY H, ARNOLD M, FERLAY J, et al. Global burden of primary liver cancer in 2020 and predictions to 2040[J]. J Hepatol, 2022, 77( 6): 1598- 1606. DOI: 10.1016/j.jhep.2022.08.021. |
| [2] |
TOH MR, WONG EYT, WONG SH, et al. Global epidemiology and genetics of hepatocellular carcinoma[J]. Gastroenterology, 2023, 164( 5): 766- 782. DOI: 10.1053/j.gastro.2023.01.033. |
| [3] |
LIEVENS Y, DEFOURNY N, CORRAL J, et al. How public health services pay for radiotherapy in Europe: An ESTRO-HERO analysis of reimbursement[J]. Lancet Oncol, 2020, 21( 1): e42- e54. DOI: 10.1016/S1470-2045(19)30794-6. |
| [4] |
BASKAR R, ITAHANA K. Radiation therapy and cancer control in developing countries: Can we save more lives?[J]. Int J Med Sci, 2017, 14( 1): 13- 17. DOI: 10.7150/ijms.17288. |
| [5] |
KOAY EJ, OWEN D, DAS P. Radiation-induced liver disease and modern radiotherapy[J]. Semin Radiat Oncol, 2018, 28( 4): 321- 331. DOI: 10.1016/j.semradonc.2018.06.007. |
| [6] |
ZHOU YJ, TANG Y, LIU SJ, et al. Radiation-induced liver disease: Beyond DNA damage[J]. Cell Cycle, 2023, 22( 5): 506- 526. DOI: 10.1080/15384101.2022.2131163. |
| [7] |
NAGARAJU GP, DARIYA B, KASA P, et al. Epigenetics in hepatocellular carcinoma[J]. Semin Cancer Biol, 2022, 86( Pt 3): 622- 632. DOI: 10.1016/j.semcancer.2021.07.017. |
| [8] |
CANTÓ C, MENZIES KJ, AUWERX J. NAD(+) metabolism and the control of energy homeostasis: A balancing act between mitochondria and the nucleus[J]. Cell Metab, 2015, 22( 1): 31- 53. DOI: 10.1016/j.cmet.2015.05.023. |
| [9] |
AVALOS JL, BOEKE JD, WOLBERGER C. Structural basis for the mechanism and regulation of Sir2 enzymes[J]. Mol Cell, 2004, 13( 5): 639- 648. DOI: 10.1016/s1097-2765(04)00082-6. |
| [10] |
|
| [11] |
MORENO-YRUELA C, BÆK M, MONDA F, et al. Chiral posttranslational modification to lysine ε-amino groups[J]. Acc Chem Res, 2022, 55( 10): 1456- 1466. DOI: 10.1021/acs.accounts.2c00115. |
| [12] |
|
| [13] |
PAN CC, KAVANAGH BD, DAWSON LA, et al. Radiation-associated liver injury[J]. Int J Radiat Oncol Biol Phys, 2010, 76( 3 Suppl): S94- S100. DOI: 10.1016/j.ijrobp.2009.06.092. |
| [14] |
MUNOZ-SCHUFFENEGGER P, NG S, DAWSON LA. Radiation-induced liver toxicity[J]. Semin Radiat Oncol, 2017, 27( 4): 350- 357. DOI: 10.1016/j.semradonc.2017.04.002. |
| [15] |
GUHA CD, KAVANAGH BD. Hepatic radiation toxicity: Avoidance and amelioration[J]. Semin Radiat Oncol, 2011, 21( 4): 256- 263. DOI: 10.1016/j.semradonc.2011.05.003. |
| [16] |
General Office of National Health Commission. Standard for diagnosis and treatment of primary liver cancer(2022 edition)[J]. J Clin Hepatol, 2022, 38( 2): 288- 303. DOI: 10.3969/j.issn.1001-5256.2022.02.009. |
| [17] |
KIM J, JUNG Y. Radiation-induced liver disease: Current understanding and future perspectives[J]. Exp Mol Med, 2017, 49( 7): e359. DOI: 10.1038/emm.2017.85. |
| [18] |
WEIGEL C, SCHMEZER P, PLASS C, et al. Epigenetics in radiation-induced fibrosis[J]. Oncogene, 2015, 34( 17): 2145- 2155. DOI: 10.1038/onc.2014.145. |
| [19] |
DE LA PINTA ALONSO C. Radiation-induced liver disease in the era of SBRT: A review[J]. Expert Rev Gastroenterol Hepatol, 2020, 14( 12): 1195- 1201. DOI: 10.1080/17474124.2020.1814744. |
| [20] |
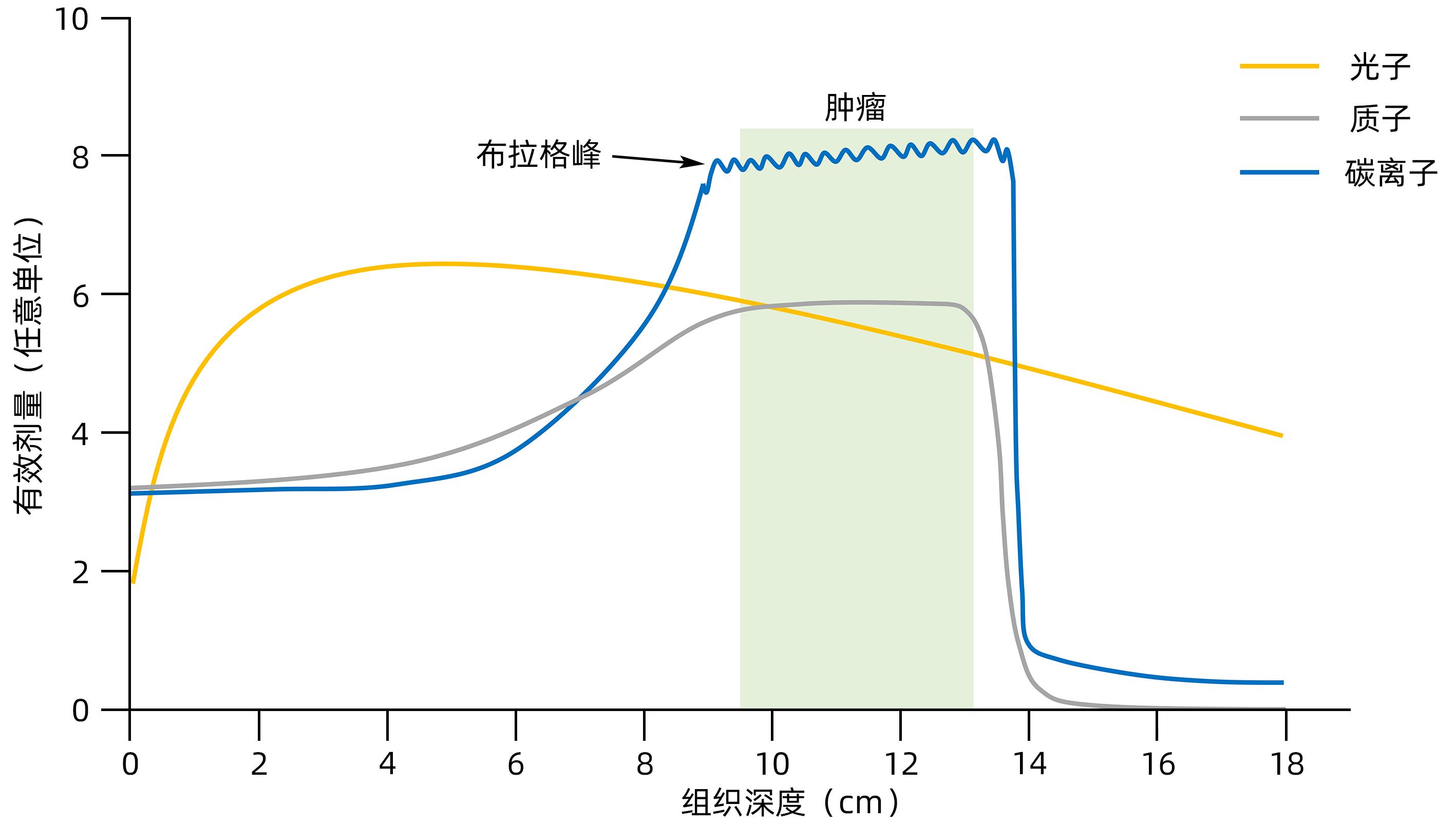
DURANTE M, ORECCHIA R, LOEFFLER JS. Charged-particle therapy in cancer: Clinical uses and future perspectives[J]. Nat Rev Clin Oncol, 2017, 14( 8): 483- 495. DOI: 10.1038/nrclinonc.2017.30. |
| [21] |
DURANTE M, FLANZ J. Charged particle beams to cure cancer: Strengths and challenges[J]. Semin Oncol, 2019, 46( 3): 219- 225. DOI: 10.1053/j.seminoncol.2019.07.007. |
| [22] |
FOKAS E, KRAFT G, AN HX, et al. Ion beam radiobiology and cancer: Time to update ourselves[J]. Biochim Biophys Acta, 2009, 1796( 2): 216- 229. DOI: 10.1016/j.bbcan.2009.07.005. |
| [23] |
WEI JL, WANG B, WANG HH, et al. Radiation-induced normal tissue damage: Oxidative stress and epigenetic mechanisms[J]. Oxid Med Cell Longev, 2019, 2019: 3010342. DOI: 10.1155/2019/3010342. |
| [24] |
LOMAX ME, FOLKES LK, O’NEILL P. Biological consequences of radiation-induced DNA damage: Relevance to radiotherapy[J]. Clin Oncol, 2013, 25( 10): 578- 585. DOI: 10.1016/j.clon.2013.06.007. |
| [25] |
MANGONI M, BORGHESI S, ARISTEI C, et al. Radiobiology of stereotactic radiotherapy[J]. Rep Pract Oncol Radiother, 2022, 27( 1): 57- 62. DOI: 10.5603/rpor.a2022.0005. |
| [26] |
WEI YL, WANG Y, JIA YM, et al. Liver homeostasis is maintained by midlobular zone 2 hepatocytes[J]. Science, 2021, 371( 6532): eabb1625. DOI: 10.1126/science.abb1625. |
| [27] |
LI TM, CAO YL, LI B, et al. The biological effects of radiation-induced liver damage and its natural protective medicine[J]. Prog Biophys Mol Biol, 2021, 167: 87- 95. DOI: 10.1016/j.pbiomolbio.2021.06.012. |
| [28] |
HUANG RX, ZHOU PK. DNA damage response signaling pathways and targets for radiotherapy sensitization in cancer[J]. Signal Transduct Target Ther, 2020, 5( 1): 60. DOI: 10.1038/s41392-020-0150-x. |
| [29] |
GONG LY, ZHANG YJ, LIU CC, et al. Application of radiosensitizers in cancer radiotherapy[J]. Int J Nanomedicine, 2021, 16: 1083- 1102. DOI: 10.2147/IJN.S290438. |
| [30] |
XIE YX, ZHANG JH, YE S, et al. SirT1 regulates radiosensitivity of hepatoma cells differently under normoxic and hypoxic conditions[J]. Cancer Sci, 2012, 103( 7): 1238- 1244. DOI: 10.1111/j.1349-7006.2012.02285.x. |
| [31] |
LAEMMLE A, LECHLEITER A, ROH V, et al. Inhibition of SIRT1 impairs the accumulation and transcriptional activity of HIF-1α protein under hypoxic conditions[J]. PLoS One, 2012, 7( 3): e33433. DOI: 10.1371/journal.pone.0033433. |
| [32] |
CHEN XJ, HUAN HB, LIU CG, et al. Deacetylation of β-catenin by SIRT1 regulates self-renewal and oncogenesis of liver cancer stem cells[J]. Cancer Lett, 2019, 463: 1- 10. DOI: 10.1016/j.canlet.2019.07.021. |
| [33] |
CUNEO KC, MORGAN MA, DAVIS MA, et al. Wee1 kinase inhibitor AZD1775 radiosensitizes hepatocellular carcinoma regardless of TP53 mutational status through induction of replication stress[J]. Int J Radiat Oncol Biol Phys, 2016, 95( 2): 782- 790. DOI: 10.1016/j.ijrobp.2016.01.028. |
| [34] |
de MATTEIS S, SCARPI E, GRANATO AM, et al. Role of SIRT-3, p-mTOR and HIF-1α in hepatocellular carcinoma patients affected by metabolic dysfunctions and in chronic treatment with metformin[J]. Int J Mol Sci, 2019, 20( 6): 1503. DOI: 10.3390/ijms20061503. |
| [35] |
FANG Y, ZHAN YZ, XIE YW, et al. Integration of glucose and cardiolipin anabolism confers radiation resistance of HCC[J]. Hepatology, 2022, 75( 6): 1386- 1401. DOI: 10.1002/hep.32177. |
| [36] |
LIU Y, QI M, LIU LC, et al. Blocking Adipor1 enhances radiation sensitivity in hepatoma carcinoma cells[J]. Arch Biochem Biophys, 2022, 718: 109152. DOI: 10.1016/j.abb.2022.109152. |
| [37] |
BAMODU OA, CHANG HL, ONG JR, et al. Elevated PDK1 expression drives PI3K/AKT/MTOR signaling promotes radiation-resistant and dedifferentiated phenotype of hepatocellular carcinoma[J]. Cells, 2020, 9( 3): 746. DOI: 10.3390/cells9030746. |
| [38] |
XU G, ZHU LH, WANG Y, et al. Stattic enhances radiosensitivity and reduces radio-induced migration and invasion in HCC cell lines through an apoptosis pathway[J]. Biomed Res Int, 2017, 2017: 1832494. DOI: 10.1155/2017/1832494. |
| [39] |
TAO RD, COLEMAN MC, PENNINGTON JD, et al. Sirt3-mediated deacetylation of evolutionarily conserved lysine 122 regulates MnSOD activity in response to stress[J]. Mol Cell, 2010, 40( 6): 893- 904. DOI: 10.1016/j.molcel.2010.12.013. |
| [40] |
REN T, ZHANG H, WANG J, et al. MCU-dependent mitochondrial Ca(2+) inhibits NAD(+)/SIRT3/SOD2 pathway to promote ROS production and metastasis of HCC cells[J]. Oncogene, 2017, 36( 42): 5897- 5909. DOI: 10.1038/onc.2017.167. |
| [41] |
LIU Y, LIU YL, CHENG W, et al. The expression of SIRT3 in primary hepatocellular carcinoma and the mechanism of its tumor suppressing effects[J]. Eur Rev Med Pharmacol Sci, 2017, 21( 5): 978- 998.
|
| [42] |
LIU XZ, REN SC, LI ZZ, et al. Sirt6 mediates antioxidative functions by increasing Nrf2 abundance[J]. Exp Cell Res, 2023, 422( 1): 113409. DOI: 10.1016/j.yexcr.2022.113409. |
| [43] |
FURUKAWA A, TADA-OIKAWA S, KAWANISHI S, et al. H2O2 accelerates cellular senescence by accumulation of acetylated p53 via decrease in the function of SIRT1 by NAD+ depletion[J]. Cell Physiol Biochem, 2007, 20( 1-4): 45- 54. DOI: 10.1159/000104152. |
| [44] |
YE TJ, LU YL, YAN XF, et al. High mobility group box-1 release from H2O2-injured hepatocytes due to sirt1 functional inhibition[J]. World J Gastroenterol, 2019, 25( 36): 5434- 5450. DOI: 10.3748/wjg.v25.i36.5434. |
| [45] |
LIU JX, LI D, ZHANG T, et al. SIRT3 protects hepatocytes from oxidative injury by enhancing ROS scavenging and mitochondrial integrity[J]. Cell Death Dis, 2017, 8( 10): e3158. DOI: 10.1038/cddis.2017.564. |
| [46] |
MELIN N, YARAHMADOV T, SANCHEZ-TALTAVULL D, et al. A new mouse model of radiation-induced liver disease reveals mitochondrial dysfunction as an underlying fibrotic stimulus[J]. JHEP Rep, 2022, 4( 7): 100508. DOI: 10.1016/j.jhepr.2022.100508. |
| [47] |
REN JH, CHEN X, ZHOU L, et al. Protective role of Sirtuin3(SIRT3) in oxidative stress mediated by hepatitis B virus X protein expression[J]. PLoS One, 2016, 11( 3): e0150961. DOI: 10.1371/journal.pone.0150961. |
| [48] |
HUANG RX, ZHOU PK. DNA damage repair: Historical perspectives, mechanistic pathways and clinical translation for targeted cancer therapy[J]. Signal Transduct Target Ther, 2021, 6( 1): 254. DOI: 10.1038/s41392-021-00648-7. |
| [49] |
PALACIOS JA, HERRANZ D, DE BONIS ML, et al. SIRT1 contributes to telomere maintenance and augments global homologous recombination[J]. J Cell Biol, 2010, 191( 7): 1299- 1313. DOI: 10.1083/jcb.201005160. |
| [50] |
GAO Y, TAN J, JIN JY, et al. SIRT6 facilitates directional telomere movement upon oxidative damage[J]. Sci Rep, 2018, 8( 1): 5407. DOI: 10.1038/s41598-018-23602-0. |
| [51] |
JEONG SM, XIAO CY, FINLEY LWS, et al. SIRT4 has tumor-suppressive activity and regulates the cellular metabolic response to DNA damage by inhibiting mitochondrial glutamine metabolism[J]. Cancer Cell, 2013, 23( 4): 450- 463. DOI: 10.1016/j.ccr.2013.02.024. |
| [52] |
MAO ZY, HINE C, TIAN X, et al. SIRT6 promotes DNA repair under stress by activating PARP1[J]. Science, 2011, 332( 6036): 1443- 1446. DOI: 10.1126/science.1202723. |
| [53] |
VAN METER M, SIMON M, TOMBLINE G, et al. JNK phosphorylates SIRT6 to stimulate DNA double-strand break repair in response to oxidative stress by recruiting PARP1 to DNA breaks[J]. Cell Rep, 2016, 16( 10): 2641- 2650. DOI: 10.1016/j.celrep.2016.08.006. |
| [54] |
VAZQUEZ BN, THACKRAY JK, SIMONET NG, et al. SIRT7 promotes genome integrity and modulates non-homologous end joining DNA repair[J]. EMBO J, 2016, 35( 14): 1488- 1503. DOI: 10.15252/embj.201593499. |
| [55] |
REZAZADEH S, YANG D, BIASHAD S ALI, et al. SIRT6 mono-ADP ribosylates KDM2A to locally increase H3K36me2 at DNA damage sites to inhibit transcription and promote repair[J]. Aging, 2020, 12( 12): 11165- 11184. DOI: 10.18632/aging.103567. |
| [56] |
CHEN Y, ZHANG HP, XU Z, et al. A PARP1-BRG1-SIRT1 axis promotes HR repair by reducing nucleosome density at DNA damage sites[J]. Nucleic Acids Res, 2019, 47( 16): 8563- 8580. DOI: 10.1093/nar/gkz592. |
| [57] |
YAMAGATA K, KITABAYASHI I. Sirt1 physically interacts with Tip60 and negatively regulates Tip60-mediated acetylation of H2AX[J]. Biochem Biophys Res Commun, 2009, 390( 4): 1355- 1360. DOI: 10.1016/j.bbrc.2009.10.156. |
| [58] |
LEE N, RYU HG, KWON JH, et al. SIRT6 depletion suppresses tumor growth by promoting cellular senescence induced by DNA damage in HCC[J]. PLoS One, 2016, 11( 11): e0165835. DOI: 10.1371/journal.pone.0165835. |
| [59] |
SERRANO L, MARTÍNEZ-REDONDO P, MARAZUELA-DUQUE A, et al. The tumor suppressor SirT2 regulates cell cycle progression and genome stability by modulating the mitotic deposition of H4K20 methylation[J]. Genes Dev, 2013, 27( 6): 639- 653. DOI: 10.1101/gad.211342.112. |
| [60] |
ZHANG WY, FENG YL, GUO QQ, et al. SIRT1 modulates cell cycle progression by regulating CHK2 acetylation-phosphorylation[J]. Cell Death Differ, 2020, 27( 2): 482- 496. DOI: 10.1038/s41418-019-0369-7. |
| [61] |
LIU TZ, LIN YH, LENG WC, et al. A divergent role of the SIRT1-TopBP1 axis in regulating metabolic checkpoint and DNA damage checkpoint[J]. Mol Cell, 2014, 56( 5): 681- 695. DOI: 10.1016/j.molcel.2014.10.007. |







 DownLoad:
DownLoad: