| [1] |
BUSQUETS J, FABREGAT J, BOROBIA FG, et al. Organ-preserving surgery for benign lesions and low-grade malignancies of the pancreatic head: A matched case-control study[J]. Surg Today, 2010, 40( 2): 125- 131. DOI: 10.1007/s00595-008-4038-6. |
| [2] |
BEGER HG, SIECH M, POCH B, et al. Limited surgery for benign tumours of the pancreas: A systematic review[J]. World J Surg, 2015, 39( 6): 1557- 1566. DOI: 10.1007/s00268-015-2976-x. |
| [3] |
BEGER HG, MAYER B, RAU BM. Parenchyma-sparing, limited pancreatic head resection for benign tumors and low-risk periampullary cancer: A systematic review[J]. J Gastrointest Surg, 2016, 20( 1): 206- 217. DOI: 10.1007/s11605-015-2981-2. |
| [4] |
BEGER HG, NAKAO A, MAYER B, et al. Duodenum-preserving total and partial pancreatic head resection for benign tumors: Systematic review and meta-analysis[J]. Pancreatology, 2015, 15( 2): 167- 178. DOI: 10.1016/j.pan.2015.01.009. |
| [5] |
BEGER HG, MAYER B, RAU BM. Parenchyma-sparing, limited pancreatic head resection for benign tumors and low-risk periampullary cancer—a systematic review[J]. J Gastrointest Surg, 2016, 20( 1): 206- 217. DOI: 10.1007/s11605-015-2981-2. |
| [6] |
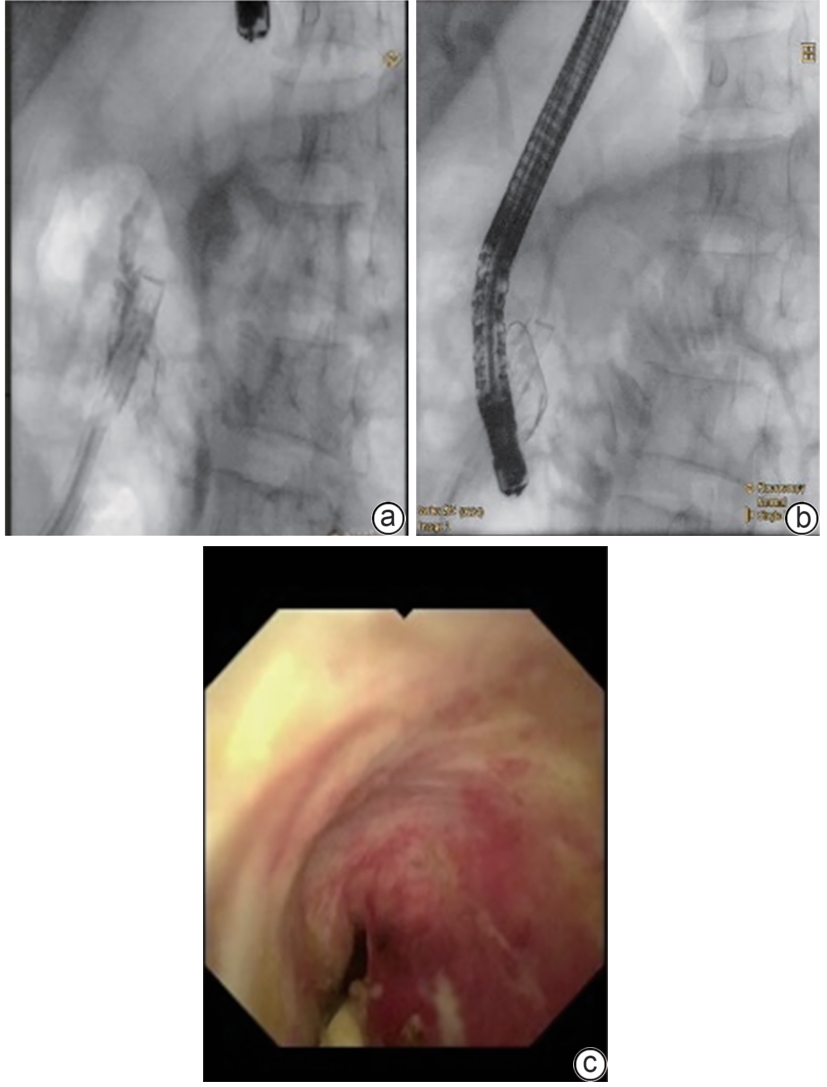
GU W, WANG Y, SHEN H, et al. Value of endoscopic biliary and pancreatic duct stents in local resection of intraductal papillary myxoma of pancreatic head[J]. J Hepatobiliary Surg, 2023, 31( 4): 296- 299. DOI: 10.3969/j.issn.1006-4761.2023.04016. |
| [7] |
LU C, XU BW, MOU YP, et al. Laparoscopic duodenum-preserving pancreatic head resection with real-time indocyanine green guidance of different dosage and timing: Enhanced safety with visualized biliary duct and its long-term metabolic morbidity[J]. Langenbecks Arch Surg, 2022, 407( 7): 2823- 2832. DOI: 10.1007/s00423-022-02570-0. |
| [8] |
de REUVER PR, GROSSMANN I, BUSCH OR, et al. Referral pattern and timing of repair are risk factors for complications after reconstructive surgery for bile duct injury[J]. Ann Surg, 2007, 245( 5): 763- 770. DOI: 10.1097/01.sla.0000252442.91839.44. |
| [9] |
BEKTAS H, SCHREM H, WINNY M, et al. Surgical treatment and outcome of iatrogenic bile duct lesions after cholecystectomy and the impact of different clinical classification systems[J]. Br J Surg, 2007, 94( 9): 1119- 1127. DOI: 10.1002/bjs.5752. |
| [10] |
RAZA A, OMER A, IQBAL S, et al. Efficacy of nasobiliary tubes and biliary stents in management of patients with bile leak after liver transplantation: A systematic review[J]. Clin Endosc, 2019, 52( 2): 159- 167. DOI: 10.5946/ce.2018.118. |
| [11] |
WEBER A, FEUSSNER H, WINKELMANN F, et al. Long-term outcome of endoscopic therapy in patients with bile duct injury after cholecystectomy[J]. J Gastroenterol Hepatol, 2009, 24( 5): 762- 769. DOI: 10.1111/j.1440-1746.2008.05713.x. |
| [12] |
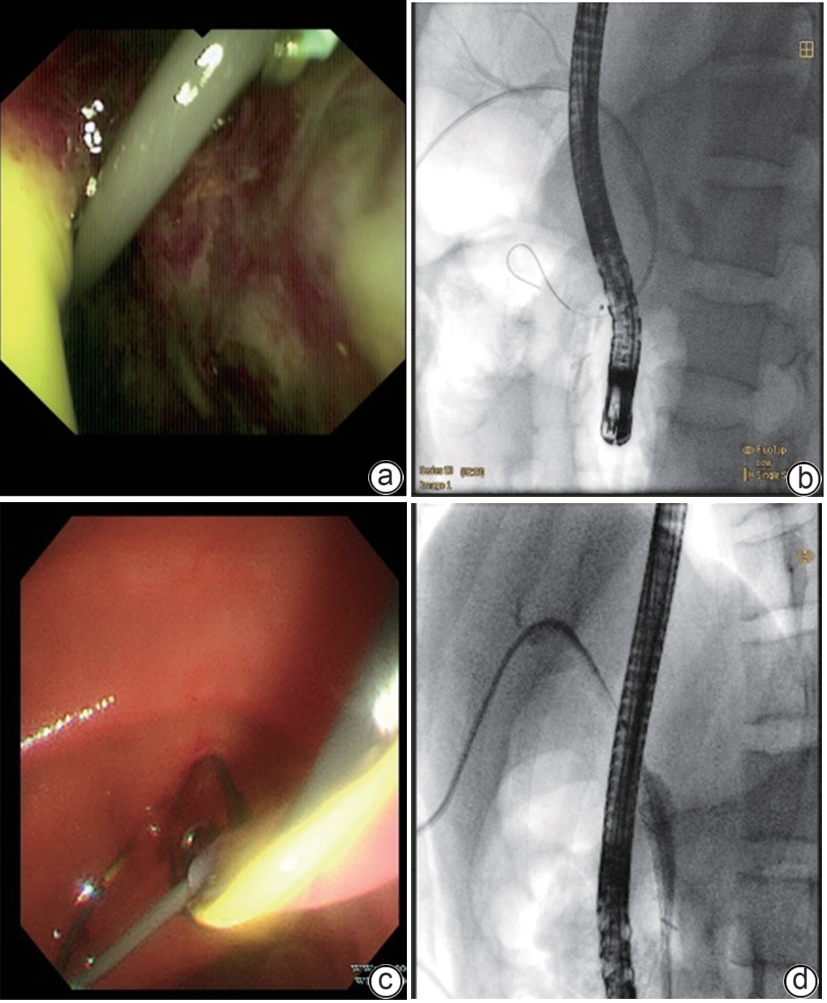
LEE Y, PARK CH, CHO E, et al. Management of post-liver transplantation biliary stricture inaccessible by endoscopic retrograde cholangiopancreatography: A case report[J]. World J Clin Cases, 2023, 11( 34): 8235- 8241. DOI: 10.12998/wjcc.v11.i34.8235. |
| [13] |
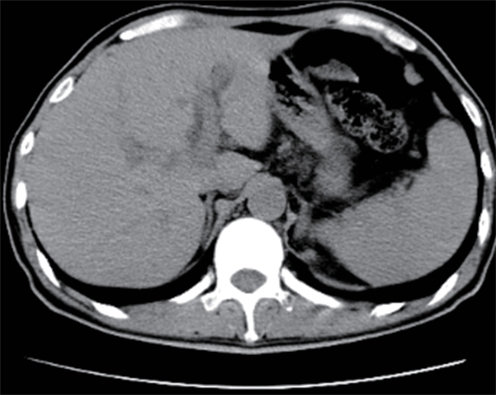
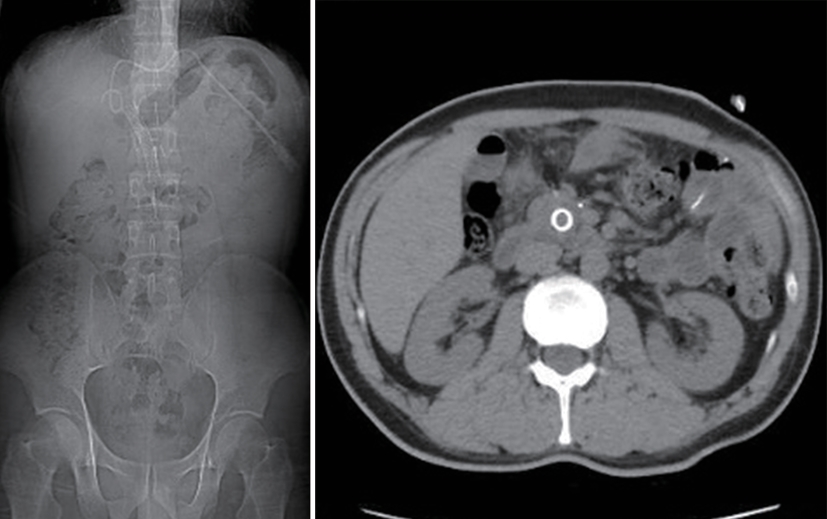
ISHIDA T, HAYASHI E, TOJIMA Y, et al. Rupture of the common bile duct due to blunt trauma, presenting difficulty in diagnosis[J]. BMJ Case Rep, 2018, 11( 1): e226467. DOI: 10.1136/bcr-2018-226467. |








 DownLoad:
DownLoad: