| [1] |
ZHENG RS, ZHANG SW, ZENG HM, et al. Cancer incidence and mortality in China, 2016[J]. J Natl Cancer Cent, 2022, 2( 1): 1- 9. DOI: 10.1016/j.jncc.2022.02.002. |
| [2] |
ZENG HM, CHEN WQ, ZHENG RS, et al. Changing cancer survival in China during 2003-15: A pooled analysis of 17 population-based cancer registries[J]. Lancet Glob Health, 2018, 6( 5): e555- e567. DOI: 10.1016/S2214-109X(18)30127-X. |
| [3] |
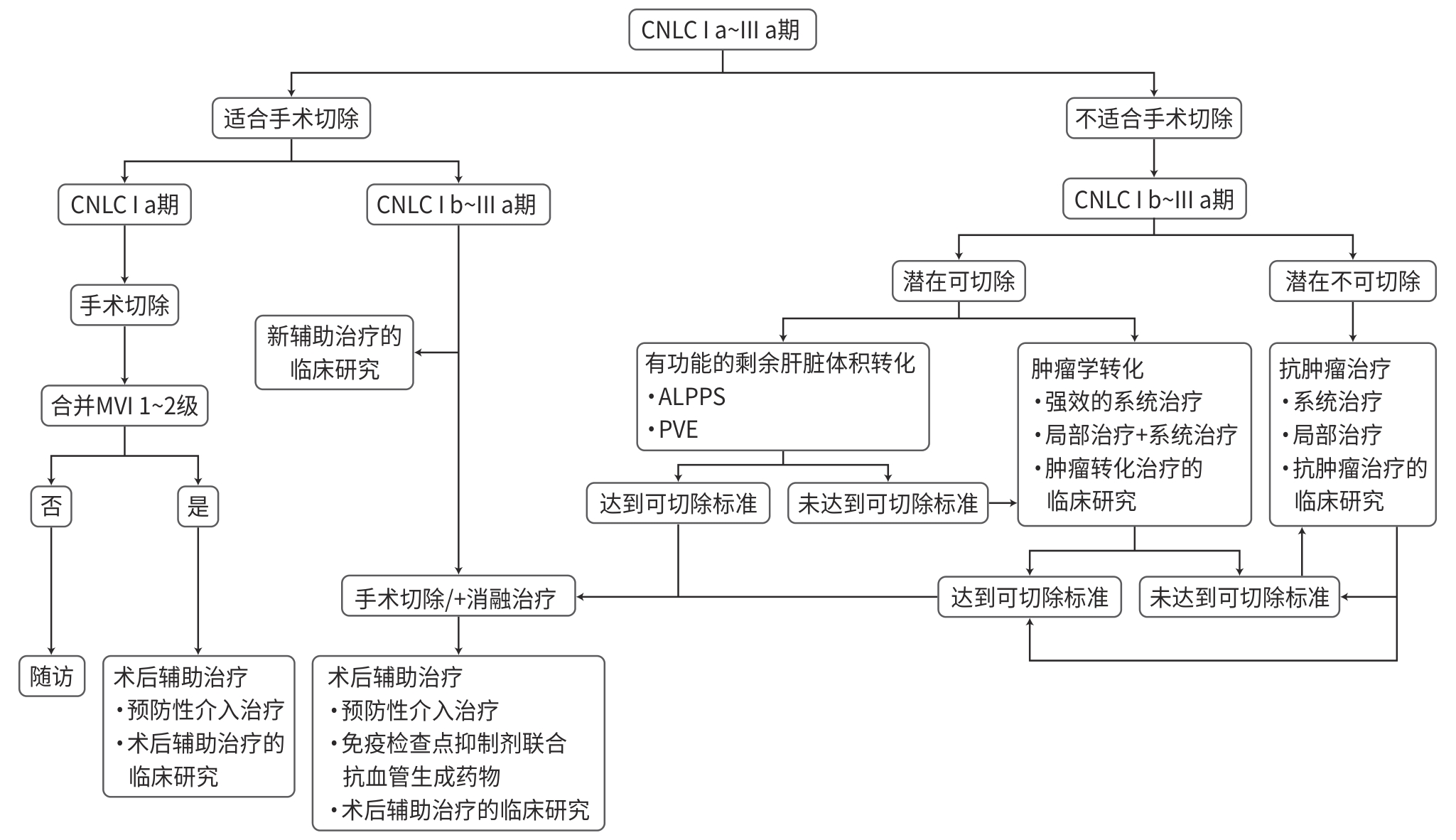
National Health Commission of the People’s Republic of China. Standard for diagnosis and treatment of primary liver cancer(2024 edition)[J]. J Clin Hepatol, 2024, 40( 5): 893- 918. DOI: 10.12449/JCH240508. 中华人民共和国国家卫生健康委员会. 原发性肝癌诊疗指南(2024年版)[J]. 临床肝胆病杂志, 2024, 40( 5): 893- 918. DOI: 10.12449/JCH240508. |
| [4] |
Society of Liver Cancer, Guangdong Provincial Anti-cancer Association. Establishment of multi-disciplinary team for comprehensive treatment of liver cancer-consensus of experts in Guangdong, China(1)[J]. J Clin Hepatol, 2014, 30( 11): 1112- 1115. DOI: 10.3969/j.issn.1001-5256.2014.11.004. |
| [5] |
Society of Liver Cancer, Guangdong Provincial Anti-cancer Association. Strategy and method of multi-disciplinary comprehensive treatment of liver cancer-consensus of experts in Guangdong, China(2)[J]. J Clin Hepatol, 2014, 30( 11): 1116- 1119. DOI: 10.3969/j.issn.1001-5256.2014.11.005. |
| [6] |
Chinese Society of Clinical Oncology(CSCO) Guidelines Committee. Guidelines of Chinese society of clinical oncology(CSCO) hepatocellular carcinoma[M]. Beijing: People’s Medical Publishing House, 2024.
中国临床肿瘤学会指南工作委员会. 中国临床肿瘤学会(CSCO)原发性肝癌诊疗指南2024[M]. 北京: 人民卫生出版社, 2024.
|
| [7] |
JIA WD. Multidisciplinary treatments for patients with hepatocellular carcinoma in the era of precise liver surgery[J]. J Pract Hepatol, 2015, 18( 2): 120- 123. DOI: 10.3969/j.issn.1672-5069.2015.02.004. |
| [8] |
CHEN MS, LI JQ, ZHENG Y, et al. A prospective randomized trial comparing percutaneous local ablative therapy and partial hepatectomy for small hepatocellular carcinoma[J]. Ann Surg, 2006, 243( 3): 321- 328. DOI: 10.1097/01.sla.0000201480.65519.b8. |
| [9] |
FENG K, YAN J, LI XW, et al. A randomized controlled trial of radiofrequency ablation and surgical resection in the treatment of small hepatocellular carcinoma[J]. J Hepatol, 2012, 57( 4): 794- 802. DOI: 10.1016/j.jhep.2012.05.007. |
| [10] |
PENG ZW, LIN XJ, ZHANG YJ, et al. Radiofrequency ablation versus hepatic resection for the treatment of hepatocellular carcinomas 2 cm or smaller: A retrospective comparative study[J]. Radiology, 2012, 262( 3): 1022- 1033. DOI: 10.1148/radiol.11110817. |
| [11] |
XU QH, KOBAYASHI S, YE X, et al. Comparison of hepatic resection and radiofrequency ablation for small hepatocellular carcinoma: A meta-analysis of 16, 103 patients[J]. Sci Rep, 2014, 4: 7252. DOI: 10.1038/srep07252. |
| [12] |
LIVRAGHI T, MELONI F, di STASI M, et al. Sustained complete response and complications rates after radiofrequency ablation of very early hepatocellular carcinoma in cirrhosis: Is resection still the treatment of choice?[J]. Hepatology, 2008, 47( 1): 82- 89. DOI: 10.1002/hep.21933. |
| [13] |
PENG ZW, ZHANG YJ, CHEN MS, et al. Radiofrequency ablation with or without transcatheter arterial chemoembolization in the treatment of hepatocellular carcinoma: A prospective randomized trial[J]. J Clin Oncol, 2013, 31( 4): 426- 432. DOI: 10.1200/JCO.2012.42.9936. |
| [14] |
ZHANG YJ, CHEN JB, ZHOU ZG, et al. Transarterial chemoembolization with radiofrequency ablation versus surgical resection for small late-recurrence hepatocellular carcinoma[J]. Radiology, 2025, 314( 2): e241096. DOI: 10.1148/radiol.241096. |
| [15] |
PAN YX, XI M, FU YZ, et al. Stereotactic body radiotherapy as a salvage therapy after incomplete radiofrequency ablation for hepatocellular carcinoma: A retrospective propensity score matching study[J]. Cancers(Basel), 2019, 11( 8): 1116. DOI: 10.3390/cancers11081116. |
| [16] |
XI M, YANG ZT, HU L, et al. Radiofrequency ablation versus stereotactic body radiotherapy for recurrent small hepatocellular carcinoma: A randomized, open-label, controlled trial[J]. J Clin Oncol, 2025, 43( 9): 1073- 1082. DOI: 10.1200/JCO-24-01532. |
| [17] |
WEI W, JIAN PE, LI SH, et al. Adjuvant transcatheter arterial chemoembolization after curative resection for hepatocellular carcinoma patients with solitary tumor and microvascular invasion: A randomized clinical trial of efficacy and safety[J]. Cancer Commun(Lond), 2018, 38( 1): 61. DOI: 10.1186/s40880-018-0331-y. |
| [18] |
LI SH, MEI J, CHENG Y, et al. Postoperative adjuvant hepatic arterial infusion chemotherapy with FOLFOX in hepatocellular carcinoma with microvascular invasion: A multicenter, phase III, randomized study[J]. J Clin Oncol, 2023, 41( 10): 1898- 1908. DOI: 10.1200/JCO.22.01142. |
| [19] |
OMATA M, CHENG AL, KOKUDO N, et al. Asia-Pacific clinical practice guidelines on the management of hepatocellular carcinoma: A 2017 update[J]. Hepatol Int, 2017, 11( 4): 317- 370. DOI: 10.1007/s12072-017-9799-9. |
| [20] |
METUSSIN A, PATANWALA I, CROSS TJ. Partial hepatectomy vs. transcatheter arterial chemoembolization for resectable multiple hepatocellular carcinoma beyond Milan criteria: a RCT[J]. J Hepatol, 2015, 62( 3): 747- 748. DOI: 10.1016/j.jhep.2014.08.057. |
| [21] |
ZHONG JH, KE Y, GONG WF, et al. Hepatic resection associated with good survival for selected patients with intermediate and advanced-stage hepatocellular carcinoma[J]. Ann Surg, 2014, 260( 2): 329- 340. DOI: 10.1097/SLA.0000000000000236. |
| [22] |
ZHOU C, PENG YF, ZHOU KQ, et al. Surgical resection plus radiofrequency ablation for the treatment of multifocal hepatocellular carcinoma[J]. Hepatobiliary Surg Nutr, 2019, 8( 1): 19- 28. DOI: 10.21037/hbsn.2018.11.19. |
| [23] |
YAN J, MAN ZS, LU Q, et al. Long-term survival in patients receiving combination therapy with resection and radiofrequency ablation for multi-focal hepatocellular carcinoma classified as Barcelona clinic liver cancer stage B: A retrospective controlled study[J]. Cancer Manag Res, 2020, 12: 2613- 2621. DOI: 10.2147/CMAR.S237635. |
| [24] |
PENG WY, CHEN JQ, LIU CW, et al. Loss of PTEN promotes resistance to T cell-mediated immunotherapy[J]. Cancer Discov, 2016, 6( 2): 202- 216. DOI: 10.1158/2159-8290.CD-15-0283. |
| [25] |
Chinese College of Interventionalists. Chinese Medical Doctor Association. Chinese Clinical Practice Guidelines for transarterial chemoembolization of hepatocellular carcinoma[J]. J Intervent Radiol, 2018, 27( 12): 1117- 1126. DOI: 10.3969/j.issn.1008-794X.2018.12.001. |
| [26] |
CHEN QW, YING HF, GAO S, et al. Radiofrequency ablation plus chemoembolization versus radiofrequency ablation alone for hepatocellular carcinoma: A systematic review and meta-analysis[J]. Clin Res Hepatol Gastroenterol, 2016, 40( 3): 309- 314. DOI: 10.1016/j.clinre.2015.07.008. |
| [27] |
KUDO M. A new treatment option for intermediate-stage hepatocellular carcinoma with high tumor burden: Initial lenvatinib therapy with subsequent selective TACE[J]. Liver Cancer, 2019, 8( 5): 299- 311. DOI: 10.1159/000502905. |
| [28] |
CHENG SQ, WU MC, CHEN H, et al. Tumor thrombus types influence the prognosis of hepatocellular carcinoma with the tumor thrombi in the portal vein[J]. Hepatogastroenterology, 2007, 54( 74): 499- 502.
|
| [29] |
XUE TC, XIE XY, ZHANG L, et al. Transarterial chemoembolization for hepatocellular carcinoma with portal vein tumor thrombus: A meta-analysis[J]. BMC Gastroenterol, 2013, 13: 60. DOI: 10.1186/1471-230X-13-60. |
| [30] |
HE MK, LI QJ, ZOU RH, et al. Sorafenib plus hepatic arterial infusion of oxaliplatin, fluorouracil, and leucovorin vs sorafenib alone for hepatocellular carcinoma with portal vein invasion: A randomized clinical trial[J]. JAMA Oncol, 2019, 5( 7): 953- 960. DOI: 10.1001/jamaoncol.2019.0250. |
| [31] |
ZHU KS, CHEN JW, LAI LS, et al. Hepatocellular carcinoma with portal vein tumor thrombus: Treatment with transarterial chemoembolization combined with sorafenib: A retrospective controlled study[J]. Radiology, 2014, 272( 1): 284- 293. DOI: 10.1148/radiol.14131946. |
| [32] |
Radiation Oncology Branch of the Chinese Medical Association Expert Committee on Liver Cancer and Digestive System of China Institute of Biomedical Engineering Liver Cancer Research Group of Radiation Oncology Branch of China Research Hospital. Consensus on radiation therapy for primary liver cancer in 2016[J]. Chin J Rad Oncol, 2016, 25( 11): 1141- 1150. DOI: 10.3760/cma.j.issn.1004-4221.2016.11.001. |
| [33] |
SUN JX, YANG L, SHI J, et al. Postoperative adjuvant IMRT for patients with HCC and portal vein tumor thrombus: An open-label randomized controlled trial[J]. Radiother Oncol, 2019, 140: 20- 25. DOI: 10.1016/j.radonc.2019.05.006. |
| [34] |
ZHANG HG, CHEN YX, HU Y, et al. Image-guided intensity-modulated radiotherapy improves short-term survival for abdominal lymph node metastases from hepatocellular carcinoma[J]. Ann Palliat Med, 2019, 8( 5): 717- 727. DOI: 10.21037/apm.2019.11.17. |
| [35] |
Chinese Society of Hepatology, Chinese Medical Association; Chinese Society of Infectious Diseases, Chinese Medical Association. Guidelines for the prevention and treatment of chronic hepatitis B(version 2022)[J]. J Pract Hepatol, 2023, 26( 3): S18- S39. DOI: 10.3969/j.issn.1672-5069.2023.03.040. |
| [36] |
Chinese Society of Hepatology, Chinese Medical Association. Guidelines on the management of ascites and complications in cirrhosis[J]. J Clin Hepatol, 2017, 33( 10): 1847- 1863. DOI: 10.3969/j.issn.1001-5256.2017.10.003. |
| [37] |
Chinese Society of Hepatology, Chinese Medical Association, Chinese Society of Gastroenterology, Chinese Medical Association. Clinical guidelines on nutrition in end-stage liver disease[J]. J Clin Hepatol, 2019, 35( 6): 1222- 1230. DOI: 10.3969/j.issn.1001-5256.2019.06.010. |
| [38] |
National Health Commission of the People’s Republic of China. Standard diagnosis and treatment of cancer pain(version 2018)[J]. Chin Clin Oncol, 2018, 23( 10): 937- 944.
中华人民共和国国家卫生健康委员会. 癌症疼痛诊疗规范(2018年版)[J]. 临床肿瘤学杂志, 2018, 23( 10): 937- 944.
|
| [39] |
KUMAR M, PANDA D. Role of supportive care for terminal stage hepatocellular carcinoma[J]. J Clin Exp Hepatol, 2014, 4( Suppl 3): S130- S139. DOI: 10.1016/j.jceh.2014.03.049. |
| [40] |
SAPISOCHIN G, BRUIX J. Liver transplantation for hepatocellular carcinoma: Outcomes and novel surgical approaches[J]. Nat Rev Gastroenterol Hepatol, 2017, 14( 4): 203- 217. DOI: 10.1038/nrgastro.2016.193. |








 DownLoad:
DownLoad: