| [1] |
Chinese Society of Hepatology of Chinese Medical Association. Chinese guidelines on the management of hepatic encephalopathy in cirrhosis(2024)[J]. Chin J Hepatol, 2024, 32( 9): 799- 812. DOI: 10.3760/cma.j.cn501113-20240630-00309. |
| [2] |
ELSAID MI, RUSTGI VK. Epidemiology of hepatic encephalopathy[J]. Clin Liver Dis, 2020, 24( 2): 157- 174. DOI: 10.1016/j.cld.2020.01.001. |
| [3] |
LIU RP, KANG JD, SARTOR RB, et al. Neuroinflammation in murine cirrhosis is dependent on the gut microbiome and is attenuated by fecal transplant[J]. Hepatology, 2020, 71( 2): 611- 626. DOI: 10.1002/hep.30827. |
| [4] |
USAMI M, MIYOSHI M, YAMASHITA H. Gut microbiota and host metabolism in liver cirrhosis[J]. World J Gastroenterol, 2015, 21( 41): 11597- 11608. DOI: 10.3748/wjg.v21.i41.11597. |
| [5] |
JIANG HN, MAO DW, YE QL, et al. Research progress on TCM syndrome differentiation and treatment of hepatic encephalopathy[J]. Shaanxi J Tradit Chin Med, 2020, 41( 11): 1678- 1680. DOI: 10.3969/j.issn.1000-7369.2020.11.042. |
| [6] |
LI JY, XIN XY, YANG HS. Experience of QIAN Ying in treating minimal hepatic encephalopathy[J]. China J Tradit Chin Med Pharm, 2021, 36( 7): 4022- 4024.
李晶滢, 辛喜艳, 杨华升. 钱英辨治轻微型肝性脑病经验[J]. 中华中医药杂志, 2021, 36( 7): 4022- 4024.
|
| [7] |
WANG MG, WANG N, MAO DW, et al. Analysis on TCM etiology and pathogenesis of mild hepatic encephalopathy[J]. Mod Tradit Chin Med, 2017, 37( 2): 55- 57. DOI: 10.13424/j.cnki.mtcm.2017.02.022. |
| [8] |
|
| [9] |
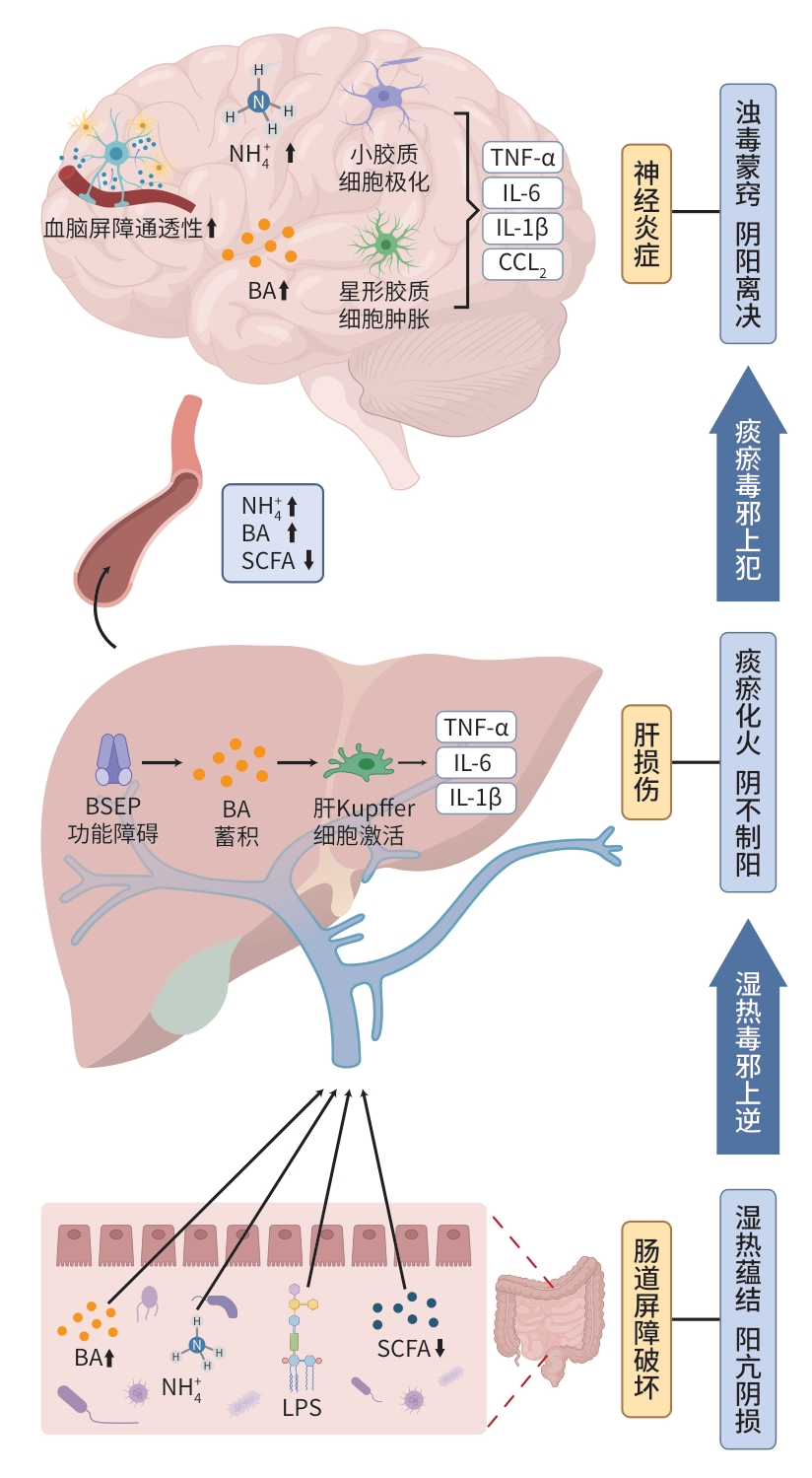
WU ZP, ZHANG YQ, YAO C, et al. Construction and practice of the theory of“turbid toxin pathogenesis” and related prevention and treatment strategies for hepatic encephalopathy in traditional Chinese medicine/Zhuang medicine[J]. J Clin Hepatol, 2025, 41( 2): 370- 374. DOI: 10.12449/JCH250226. 吴智鹏, 张钰琴, 姚春, 等. 肝性脑病中医/壮医“浊毒致病” 理论及防治策略的构建与实践[J]. 临床肝胆病杂志, 2025, 41( 2): 370- 374. DOI: 10.12449/JCH250226. |
| [10] |
XIE XX, DU LN, GUO ZY, et al. Role of apical sodium-dependent bile acid transporter in hepatobiliary diseases[J]. J Clin Hepatol, 2024, 40( 1): 199- 203. DOI: 10.12449/JCH240133. 谢晓暄, 杜丽娜, 郭紫云, 等. 顶端钠依赖性胆汁酸转运蛋白(ASBT)在肝胆疾病中的作用[J]. 临床肝胆病杂志, 2024, 40( 1): 199- 203. DOI: 10.12449/JCH240133. |
| [11] |
LARABI AB, MASSON HLP, BÄUMLER AJ. Bile acids as modulators of gut microbiota composition and function[J]. Gut Microbes, 2023, 15( 1): 2172671. DOI: 10.1080/19490976.2023.2172671. |
| [12] |
XIE XM, ZHANG BY, FENG S, et al. Activation of gut FXR improves the metabolism of bile acids, intestinal barrier, and microbiota under cholestatic condition caused by GCDCA in mice[J]. Microbiol Spectr, 2025, 13( 4): e0315024. DOI: 10.1128/spectrum.03150-24. |
| [13] |
WANG XN, XIE GX, ZHAO AH, et al. Serum bile acids are associated with pathological progression of hepatitis B-induced cirrhosis[J]. J Proteome Res, 2016, 15( 4): 1126- 1134. DOI: 10.1021/acs.jproteome.5b00217. |
| [14] |
ZHU F, ZHENG SD, ZHAO M, et al. The regulatory role of bile acid microbiota in the progression of liver cirrhosis[J]. Front Pharmacol, 2023, 14: 1214685. DOI: 10.3389/fphar.2023.1214685. |
| [15] |
WEN JB, ZHU FQ, CHEN WG, et al. Oxymatrine improves intestinal epithelial barrier function involving NF-κB-mediated signaling pathway in CCl 4-induced cirrhotic rats[J]. PLoS One, 2014, 9( 8): e106082. DOI: 10.1371/journal.pone.0106082. |
| [16] |
WANG Y, YU YB, LI LX, et al. Bile acid-dependent transcription factors and chromatin accessibility determine regional heterogeneity of intestinal antimicrobial peptides[J]. Nat Commun, 2023, 14( 1): 5093. DOI: 10.1038/s41467-023-40565-7. |
| [17] |
XIE GX, WANG XN, JIANG RQ, et al. Dysregulated bile acid signaling contributes to the neurological impairment in murine models of acute and chronic liver failure[J]. EBioMedicine, 2018, 37: 294- 306. DOI: 10.1016/j.ebiom.2018.10.030. |
| [18] |
XUE R, SU LY, LAI SY, et al. Bile acid receptors and the gut-liver axis in nonalcoholic fatty liver disease[J]. Cells, 2021, 10( 11): 2806. DOI: 10.3390/cells10112806. |
| [19] |
ZENG L, HUANG JX, WANG Y, et al. Oleanolic acid induces hepatic injury by disrupting hepatocyte tight junction and dysregulation of farnesoid X receptor-mediated bile acid efflux transporters[J]. J Appl Toxicol, 2024, 44( 11): 1725- 1741. DOI: 10.1002/jat.4667. |
| [20] |
LU JL, GAO YT, GONG Y, et al. Lycium barbarum L. Balanced intestinal flora with YAP1/FXR activation in drug-induced liver injury[J]. Int Immunopharmacol, 2024, 130: 111762. DOI: 10.1016/j.intimp.2024.111762. |
| [21] |
XIAO YT, WANG WP, PENG SC, et al. Farnesoid X receptor agonist tropifexor detoxifies ammonia by regulating the glutamine metabolism and urea cycles in cholestatic livers[J]. Eur J Pharmacol, 2024, 966: 176334. DOI: 10.1016/j.ejphar.2024.176334. |
| [22] |
XING C, HUANG X, WANG DX, et al. Roles of bile acids signaling in neuromodulation under physiological and pathological conditions[J]. Cell Biosci, 2023, 13( 1): 106. DOI: 10.1186/s13578-023-01053-z. |
| [23] |
|
| [24] |
QUINN M, MCMILLIN M, GALINDO C, et al. Bile acids permeabilize the blood brain barrier after bile duct ligation in rats via Rac1-dependent mechanisms[J]. Dig Liver Dis, 2014, 46( 6): 527- 534. DOI: 10.1016/j.dld.2014.01.159. |
| [25] |
MCMILLIN M, FRAMPTON G, GRANT S, et al. Bile acid-mediated sphingosine-1-phosphate receptor 2 signaling promotes neuroinflammation during hepatic encephalopathy in mice[J]. Front Cell Neurosci, 2017, 11: 191. DOI: 10.3389/fncel.2017.00191. |
| [26] |
NORENBERG MD, RAMA RAO KV, JAYAKUMAR AR. Mechanisms of ammonia-induced astrocyte swelling[J]. Metab Brain Dis, 2005, 20( 4): 303- 318. DOI: 10.1007/s11011-005-7911-7. |
| [27] |
CHEON SY, KIM MY, KIM J, et al. Hyperammonemia induces microglial NLRP3 inflammasome activation via mitochondrial oxidative stress in hepatic encephalopathy[J]. Biomed J, 2023, 46( 5): 100593. DOI: 10.1016/j.bj.2023.04.001. |
| [28] |
LIU PY, WANG YB, YANG G, et al. The role of short-chain fatty acids in intestinal barrier function, inflammation, oxidative stress, and colonic carcinogenesis[J]. Pharmacol Res, 2021, 165: 105420. DOI: 10.1016/j.phrs.2021.105420. |
| [29] |
LI GF, LIN J, ZHANG C, et al. Microbiota metabolite butyrate constrains neutrophil functions and ameliorates mucosal inflammation in inflammatory bowel disease[J]. Gut Microbes, 2021, 13( 1): 1968257. DOI: 10.1080/19490976.2021.1968257. |
| [30] |
ZHU RR, LIU LW, ZHANG GZ, et al. The pathogenesis of gut microbiota in hepatic encephalopathy by the gut-liver-brain axis[J]. Biosci Rep, 2023, 43( 6): BSR20222524. DOI: 10.1042/BSR20222524. |
| [31] |
WANG Q, CHEN CX, ZUO S, et al. Integrative analysis of the gut microbiota and faecal and serum short-chain fatty acids and tryptophan metabolites in patients with cirrhosis and hepatic encephalopathy[J]. J Transl Med, 2023, 21( 1): 395. DOI: 10.1186/s12967-023-04262-9. |
| [32] |
ZHANG SM, ZHAO JW, XIE F, et al. Dietary fiber-derived short-chain fatty acids: A potential therapeutic target to alleviate obesity-related nonalcoholic fatty liver disease[J]. Obes Rev, 2021, 22( 11): e13316. DOI: 10.1111/obr.13316. |
| [33] |
BASHIARDES S, SHAPIRO H, ROZIN S, et al. Non-alcoholic fatty liver and the gut microbiota[J]. Mol Metab, 2016, 5( 9): 782- 794. DOI: 10.1016/j.molmet.2016.06.003. |
| [34] |
FOCK E, PARNOVA R. Mechanisms of blood-brain barrier protection by microbiota-derived short-chain fatty acids[J]. Cells, 2023, 12( 4): 657. DOI: 10.3390/cells12040657. |
| [35] |
BLOOM PP, LUÉVANO JM Jr, MILLER KJ, et al. Deep stool microbiome analysis in cirrhosis reveals an association between short-chain fatty acids and hepatic encephalopathy[J]. Ann Hepatol, 2021, 25: 100333. DOI: 10.1016/j.aohep.2021.100333. |
| [36] |
LIU JM, JIN YJ, YE YL, et al. The neuroprotective effect of short chain fatty acids against sepsis-associated encephalopathy in mice[J]. Front Immunol, 2021, 12: 626894. DOI: 10.3389/fimmu.2021.626894. |
| [37] |
HARRISON IF, DEXTER DT. Epigenetic targeting of histone deacetylase: Therapeutic potential in Parkinson’s disease?[J]. Pharmacol Ther, 2013, 140( 1): 34- 52. DOI: 10.1016/j.pharmthera.2013.05.010. |
| [38] |
RIZZOLO D, KONG B, TAYLOR RE, et al. Bile acid homeostasis in female mice deficient in Cyp7a1 and Cyp27a1[J]. Acta Pharm Sin B, 2021, 11( 12): 3847- 3856. DOI: 10.1016/j.apsb.2021.05.023. |
| [39] |
DUCASTEL S, TOUCHE V, TRABELSI MS, et al. The nuclear receptor FXR inhibits Glucagon-Like Peptide-1 secretion in response to microbiota-derived Short-Chain Fatty Acids[J]. Sci Rep, 2020, 10( 1): 174. DOI: 10.1038/s41598-019-56743-x. |
| [40] |
PAN LY, YU Z, LIANG XL, et al. Sodium cholate ameliorates nonalcoholic steatohepatitis by activation of FXR signaling[J]. Hepatol Commun, 2023, 7( 2): e0039. DOI: 10.1097/HC9.0000000000000039. |
| [41] |
ZAUFEL A, van de WIEL SMW, YIN L, et al. Secondary( Iso)BAs cooperate with endogenous ligands to activate FXR under physiological and pathological conditions[J]. Biochim Biophys Acta Mol Basis Dis, 2021, 1867( 8): 166153. DOI: 10.1016/j.bbadis.2021.166153. |
| [42] |
WANG ZY, QIANG X, PENG YJ, et al. Design and synthesis of bile acid derivatives and their activity against colon cancer[J]. RSC Med Chem, 2022, 13( 11): 1391- 1409. DOI: 10.1039/d2md00220e. |
| [43] |
GU M, ZHAO P, ZHANG SY, et al. Betulinic acid alleviates endoplasmic reticulum stress-mediated nonalcoholic fatty liver disease through activation of farnesoid X receptors in mice[J]. Br J Pharmacol, 2019, 176( 7): 847- 863. DOI: 10.1111/bph.14570. |
| [44] |
KAEWARSAR E, CHAIYASUT C, LAILERD N, et al. Optimization of mixed inulin, fructooligosaccharides, and galactooligosaccharides as prebiotics for stimulation of probiotics growth and function[J]. Foods, 2023, 12( 8): 1591. DOI: 10.3390/foods12081591. |
| [45] |
WANG N, WANG MG, MAO DW, et al. Clinical observation of rhubarb decoction in the treatment of type A hepatic encephalopathy[J]. Lishizhen Med Mater Med Res, 2015, 26( 5): 1169- 1171. DOI: 10.3969/j.issn.1008-0805.2015.05.053. |
| [46] |
HU Z, CHENG XH, CAI J, et al. Emodin alleviates cholestatic liver injury by modulating Sirt1/Fxr signaling pathways[J]. Sci Rep, 2024, 14( 1): 16756. DOI: 10.1038/s41598-024-67882-1. |
| [47] |
HAN SQ, HA W, SHI YP. Research progress on anti-inflammatory effect of Rhei Radix et Rhizoma and its active components[J]. Chin Tradit Herb Drugs, 2023, 54( 1): 303- 316. DOI: 10.7501/ j.issn.0253-2670.2023.01.032.
韩思琪, 哈伟, 师彦平. 大黄及其有效成分抗炎作用的研究进展[J]. 中草药, 2023, 54( 1): 303- 316. DOI: 10.7501/ j.issn.0253-2670.2023.01.032.
|
| [48] |
LIU ZH, PENG Y, SUN CZ, et al. Evaluation of therapeutic effects of Mume Fructus powder and water decoction on Crohn’s rats based on in vitro human gastrointestinal metabolism[J]. Chin Tradit Herb Drugs, 2022, 53( 19): 6054- 6067. DOI: 10.7501/j.issn.0253- 2670.2022.19.012.
刘治华, 彭颖, 孙崇智, 等. 基于体外人源胃肠道代谢评价乌梅粉和水煎剂对克罗恩大鼠的治疗作用[J]. 中草药, 2022, 53( 19): 6054- 6067. DOI: 10.7501/j.issn.0253- 2670.2022.19.012.
|
| [49] |
WEN XD, WANG CL, XING SM, et al. Current advances in understanding neuroprotective effect of Wumei(mume fructus) in neurodegenerative diseases[J]. Chin Arch Tradit Chin Med, 2024, 42( 1): 41- 45. DOI: 10.13193/j.issn.1673-7717.2024.01.008. |
| [50] |
DU YQ, WANG M, XU J, et al. Investigation of therapeutic effects of rhubarb decoction retention Enema on minimal hepatic encephalopathy in rats based on 16S rDNA gene sequencing and bile acid metabolomics[J]. J Pharm Biomed Anal, 2023, 230: 115392. DOI: 10.1016/j.jpba.2023.115392. |







 DownLoad:
DownLoad: