| [1] |
|
| [2] |
DUAN Z, JIA JD, HOU J, et al. Current challenges and the management of chronic hepatitis C in mainland China[J]. J Clin Gastroenterol, 2014, 48(8): 679-686. DOI: 10.1097/MCG.0000000000000109. |
| [3] |
MCGLYNN KA, PETRICK JL, EL-SERAG HB. Epidemiology of hepatocellular carcinoma[J]. Hepatology, 2021, 73(Suppl 1): 4-13. DOI: 10.1002/hep.31288. |
| [4] |
FATTOVICH G, STROFFOLINI T, ZAGNI I, et al. Hepatocellular carcinoma in cirrhosis: Incidence and risk factors[J]. Gastroenterology, 2004, 127(5 Suppl 1): s35-s50. DOI: 10.1053/j.gastro.2004.09.014. |
| [5] |
KUMAR R, TEO EK, HOW CH, et al. A practical clinical approach to liver fibrosis[J]. Singapore Med J, 2018, 59(12): 628-633. DOI: 10.11622/smedj.2018145. |
| [6] |
GRGUREVIC I, BOZIN T, MADIR A. Hepatitis C is now curable, but what happens with cirrhosis and portal hypertension afterwards?[J]. Clin Exp Hepatol, 2017, 3(4): 181-186. DOI: 10.5114/ceh.2017.71491. |
| [7] |
KONG Y, SUN Y, ZHOU J, et al. Early steep decline of liver stiffness predicts histological reversal of fibrosis in chronic hepatitis B patients treated with entecavir[J]. J Viral Hepat, 2019, 26(5): 576-585. DOI: 10.1111/jvh.13058. |
| [8] |
STASI C, MILANI S. Evolving strategies for liver fibrosis staging: Non-invasive assessment[J]. World J Gastroenterol, 2017, 23(2): 191-196. DOI: 10.3748/wjg.v23.i2.191. |
| [9] |
CARMONA I, CORDERO P, AMPUERO J, et al. Role of assessing liver fibrosis in management of chronic hepatitis C virus infection[J]. Clin Microbiol Infect, 2016, 22(10): 839-845. DOI: 10.1016/j.cmi.2016.09.017. |
| [10] |
ZHENG J, CAI J, LI H, et al. Neutrophil to lymphocyte ratio and platelet to lymphocyte ratio as prognostic predictors for hepatocellular carcinoma patients with various treatments: A Meta-analysis and systematic review[J]. Cell Physiol Biochem, 2017, 44(3): 967-981. DOI: 10.1159/000485396. |
| [11] |
STOJKOVIC LALOSEVIC M, PAVLOVIC MARKOVIC A, STANKOVIC S, et al. Combined diagnostic efficacy of neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), and mean platelet volume (MPV) as biomarkers of systemic inflammation in the diagnosis of colorectal cancer[J]. Dis Markers, 2019, 2019: 6036979. DOI: 10.1155/2019/6036979. |
| [12] |
PAN YC, JIA ZF, CAO DH, et al. Preoperative lymphocyte-to-monocyte ratio (LMR) could independently predict overall survival of resectable gastric cancer patients[J]. Medicine (Baltimore), 2018, 97(52): e13896. DOI: 10.1097/MD.0000000000013896. |
| [13] |
LAI Q, CASTRO SANTA E, RICO JURI JM, et al. Neutrophil and platelet-to-lymphocyte ratio as new predictors of dropout and recurrence after liver transplantation for hepatocellular cancer[J]. Transpl Int, 2014, 27(1): 32-41. DOI: 10.1111/tri.12191. |
| [14] |
LIN L, YANG F, WANG Y, et al. Prognostic nomogram incorporating neutrophil-to-lymphocyte ratio for early mortality in decompensated liver cirrhosis[J]. Int Immunopharmacol, 2018, 56: 58-64. DOI: 10.1016/j.intimp.2018.01.007. |
| [15] |
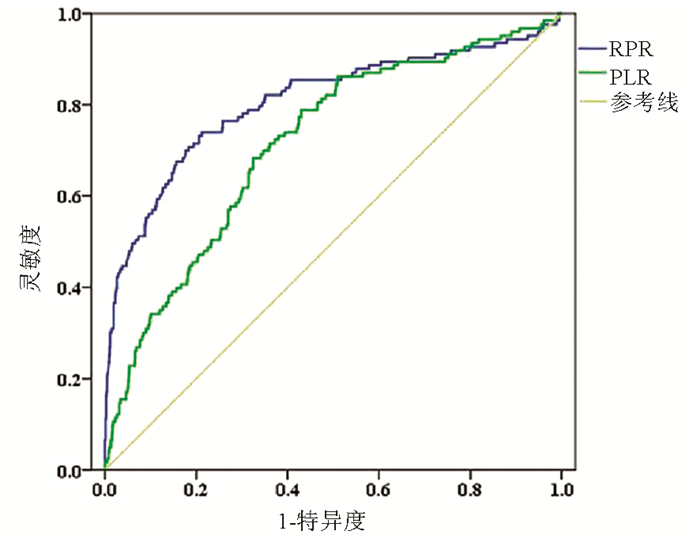
MILAS GP, KARAGEORGIOU V, CHOLONGITAS E. Red cell distribution width to platelet ratio for liver fibrosis: A systematic review and meta-analysis of diagnostic accuracy[J]. Expert Rev Gastroenterol Hepatol, 2019, 13(9): 877-891. DOI: 10.1080/17474124.2019.1653757. |
| [16] |
MENG X, WEI G, CHANG Q, et al. The platelet-to-lymphocyte ratio, superior to the neutrophil-to-lymphocyte ratio, correlates with hepatitis C virus infection[J]. Int J Infect Dis, 2016, 45: 72-77. DOI: 10.1016/j.ijid.2016.02.025. |
| [17] |
ZHAO Z, LIU J, WANG J, et al. Platelet-to-lymphocyte ratio (PLR) and neutrophil-to-lymphocyte ratio (NLR) are associated with chronic hepatitis B virus (HBV) infection[J]. Int Immunopharmacol, 2017, 51: 1-8. DOI: 10.1016/j.intimp.2017.07.007. |
| [18] |
PENG Y, LI Y, HE Y, et al. The role of neutrophil to lymphocyte ratio for the assessment of liver fibrosis and cirrhosis: a systematic review[J]. Expert Rev Gastroenterol Hepatol, 2018, 12(5): 503-513. DOI: 10.1080/17474124.2018.1463158. |
| [19] |
Chinese Society of Hepatology, Chinese Medical Association; Chinese Society of Infectious Diseases, Chinese Medical Association. Guidelines for the prevention and treatment of hepatitis C (2019 version)[J]. J Clin Hepatol, 2019, 35(12): 2670-2686. DOI: 10.3969/j.issn.1001-5256.2019.12.008. |
| [20] |
Chinese Society of Hepatology, Chinese Medical Association. Chinese guidelines on the management of liver cirrhosis[J]. J Clin Hepatol, 2019, 35(11): 2408-2425. DOI: 10.3969/j.issn.1001-5256.2019.11.006. |
| [21] |
|
| [22] |
D'AMICO G, GARCIA-TSAO G, PAGLIARO L. Natural history and prognostic indicators of survival in cirrhosis: A systematic review of 118 studies[J]. J Hepatol, 2006, 44(1): 217-231. DOI: 10.1016/j.jhep.2005.10.013. |
| [23] |
YANG M, PARIKH ND, LIU H, et al. Incidence and risk factors of hepatocellular carcinoma in patients with hepatitis C in China and the United States[J]. Sci Rep, 2020, 10(1): 20922. DOI: 10.1038/s41598-020-77515-y. |
| [24] |
BIAN DD, JIANG YY, ZHOU HY, et al. Current status of antiviral therapy for hepatitis C related cirrhosis and hepatocellular carcinoma in mainland China[J]. Chin J Gastroenterol Hepatol, 2019, 28(7): 750-754. DOI: 10.3969/j.issn.1006-5709.2019.07.007. |
| [25] |
|
| [26] |
LIPPI G, PLEBANI M. Red blood cell distribution width (RDW) and human pathology. One size fits all[J]. Clin Chem Lab Med, 2014, 52(9): 1247-1249. DOI: 10.1515/cclm-2014-0585. |
| [27] |
TEKCE H, KIN TEKCE B, AKTAS G, et al. The evaluation of red cell distribution width in chronic hemodialysis patients[J]. Int J Nephrol, 2014, 2014: 754370. DOI: 10.1155/2014/754370. |
| [28] |
JELKMANN W. Proinflammatory cytokines lowering erythropoietin production[J]. J Interferon Cytokine Res, 1998, 18(8): 555-559. DOI: 10.1089/jir.1998.18.555. |
| [29] |
WANG ZD, WU H. Pathogenesis and treatment of thrombocytopenia in patients with liver cirrhosis[J]. Prac J Clin Med, 2020, 17(1): 212-215. DOI: 10.3969/j.issn.1672-6170.2020.01.065. |
| [30] |
KUROKAWA T, OHKOHCHI N. Platelets in liver disease, cancer and regeneration[J]. World J Gastroenterol, 2017, 23(18): 3228-3239. DOI: 10.3748/wjg.v23.i18.3228. |
| [31] |
LI X, XU H, GAO P. Red Blood Cell Distribution width-to-platelet ratio and other laboratory indices associated with severity of histological hepatic fibrosis in patients with autoimmune hepatitis: A retrospective study at a single center[J]. Med Sci Monit, 2020, 26: e927946. DOI: 10.12659/MSM.927946. |
| [32] |
HE Q, HE Q, QIN X, et al. The relationship between inflammatory marker levels and hepatitis C virus severity[J]. Gastroenterol Res Pract, 2016, 2016: 2978479. DOI: 10.1155/2016/2978479. |
| [33] |
GOMEZ D, FARID S, MALIK HZ, et al. Preoperative neutrophil-to-lymphocyte ratio as a prognostic predictor after curative resection for hepatocellular carcinoma[J]. World J Surg, 2008, 32(8): 1757-1762. DOI: 10.1007/s00268-008-9552-6. |
| [34] |
LI X, WANG L, GAO P. Chronic hepatitis C virus infection: Relationships between inflammatory marker levels and compensated liver cirrhosis[J]. Medicine (Baltimore), 2019, 98(39): e17300. DOI: 10.1097/MD.0000000000017300. |
| [35] |
ABDEL-RAZIK A, MOUSA N, BESHEER T A, et al. Neutrophil to lymphocyte ratio as a reliable marker to predict insulin resistance and fibrosis stage in chronic hepatitis C virus infection[J]. Acta Gastroenterol Belg, 2015, 78(4): 386-392. DOI: 10.1109/APS.2006.1711016. |













 DownLoad:
DownLoad:
