| [1] |
LEE PJ, PAPACHRISTOU GI. New insights into acute pancreatitis[J]. Nat Rev Gastroenterol Hepatol, 2019, 16(8): 479-496. DOI: 10.1038/s41575-019-0158-2. |
| [2] |
|
| [3] |
ZHOU H, MEI X, HE X, et al. Severity stratification and prognostic prediction of patients with acute pancreatitis at early phase: A retrospective study[J]. Medicine (Baltimore), 2019, 98(16): e15275. DOI: 10.1097/MD.0000000000015275. |
| [4] |
KONG W, HE Y, BAO H, et al. Diagnostic value of neutrophil-lymphocyte ratio for predicting the severity of acute pancreatitis: A meta-analysis[J]. Dis Markers, 2020, 2020: 9731854. DOI: 10.1155/2020/9731854. |
| [5] |
LI M, XING XK, LU ZH, et al. Comparison of scoring systems in predicting severity and prognosis of hypertriglyceridemia-induced acute pancreatitis[J]. Dig Dis Sci, 2020, 65(4): 1206-1211. DOI: 10.1007/s10620-019-05827-9. |
| [6] |
UNAMUNO X, GÓMEZ-AMBROSI J, RODRÍGUEZ A, et al. Adipokine dysregulation and adipose tissue inflammation in human obesity[J]. Eur J Clin Invest, 2018, 48(9): e12997. DOI: 10.1111/eci.12997. |
| [7] |
CHEN SM, XIONG GS, WU SM. Is obesity an indicator of complications and mortality in acute pancreatitis? An updated meta-analysis[J]. J Dig Dis, 2012, 13(5): 244-251. DOI: 10.1111/j.1751-2980.2012.00587.x. |
| [8] |
WAKABAYASHI I, DAIMON T. The "cardiometabolic index" as a new marker determined by adiposity and blood lipids for discrimination of diabetes mellitus[J]. Clin Chim Acta, 2015, 438: 274-278. DOI: 10.1016/j.cca.2014.08.042. |
| [9] |
BANKS PA, BOLLEN TL, DERVENIS C, et al. Classification of acute pancreatitis--2012: revision of the Atlanta classification and definitions by international consensus[J]. Gut, 2013, 62(1): 102-111. DOI: 10.1136/gutjnl-2012-302779. |
| [10] |
SINGH RG, CERVANTES A, KIM JU, et al. Intrapancreatic fat deposition and visceral fat volume are associated with the presence of diabetes after acute pancreatitis[J]. Am J Physiol Gastrointest Liver Physiol, 2019, 316(6): G806-G815. DOI: 10.1152/ajpgi.00385.2018. |
| [11] |
PITT HA. Hepato-pancreato-biliary fat: the good, the bad and the ugly[J]. HPB (Oxford), 2007, 9(2): 92-97. DOI: 10.1080/13651820701286177. |
| [12] |
FAIN JN, MADAN AK, HILER ML, et al. Comparison of the release of adipokines by adipose tissue, adipose tissue matrix, and adipocytes from visceral and subcutaneous abdominal adipose tissues of obese humans[J]. Endocrinology, 2004, 145(5): 2273-2282. DOI: 10.1210/en.2003-1336. |
| [13] |
WANG C. Obesity, inflammation, and lung injury (OILI): the good[J]. Mediators Inflamm, 2014, 2014: 978463.
|
| [14] |
NATU A, STEVENS T, KANG L, et al. Visceral adiposity predicts severity of acute pancreatitis[J]. Pancreas, 2017, 46(6): 776-781. DOI: 10.1097/MPA.0000000000000845. |
| [15] |
PATEL K, TRIVEDI RN, DURGAMPUDI C, et al. Lipolysis of visceral adipocyte triglyceride by pancreatic lipases converts mild acute pancreatitis to severe pancreatitis independent of necrosis and inflammation[J]. Am J Pathol, 2015, 185(3): 808-819. DOI: 10.1016/j.ajpath.2014.11.019. |
| [16] |
KATUCHOVA J, BOBER J, HARBULAK P, et al. Obesity as a risk factor for severe acute pancreatitis patients[J]. Wien Klin Wochenschr, 2014, 126(7-8): 223-227. DOI: 10.1007/s00508-014-0507-7 |
| [17] |
SADR-AZODI O, ORSINI N, ANDRÉN-SANDBERG Å, et al. Abdominal and total adiposity and the risk of acute pancreatitis: a population-based prospective cohort study[J]. Am J Gastroenterol, 2013, 108(1): 133-139. DOI: 10.1038/ajg.2012.381. |
| [18] |
CHEN L, HUANG Y, YU H, et al. The association of parameters of body composition and laboratory markers with the severity of hypertriglyceridemia-induced pancreatitis[J]. Lipids Health Dis, 2021, 20(1): 9. DOI: 10.1186/s12944-021-01443-7 |
| [19] |
YOON SB, CHOI MH, LEE IS, et al. Impact of body fat and muscle distribution on severity of acute pancreatitis[J]. Pancreatology, 2017, 17(2): 188-193. DOI: 10.1016/j.pan.2017.02.002 |
| [20] |
FANG H, BERG E, CHENG X, et al. How to best assess abdominal obesity[J]. Curr Opin Clin Nutr Metab Care, 2018, 21(5): 360-365. DOI: 10.1097/MCO.0000000000000485 |
| [21] |
O'LEARY DP, O'NEILL D, MCLAUGHLIN P, et al. Effects of abdominal fat distribution parameters on severity of acute pancreatitis[J]. World J Surg, 2012, 36(7): 1679-1685. DOI: 10.1007/s00268-011-1414-y. |
| [22] |
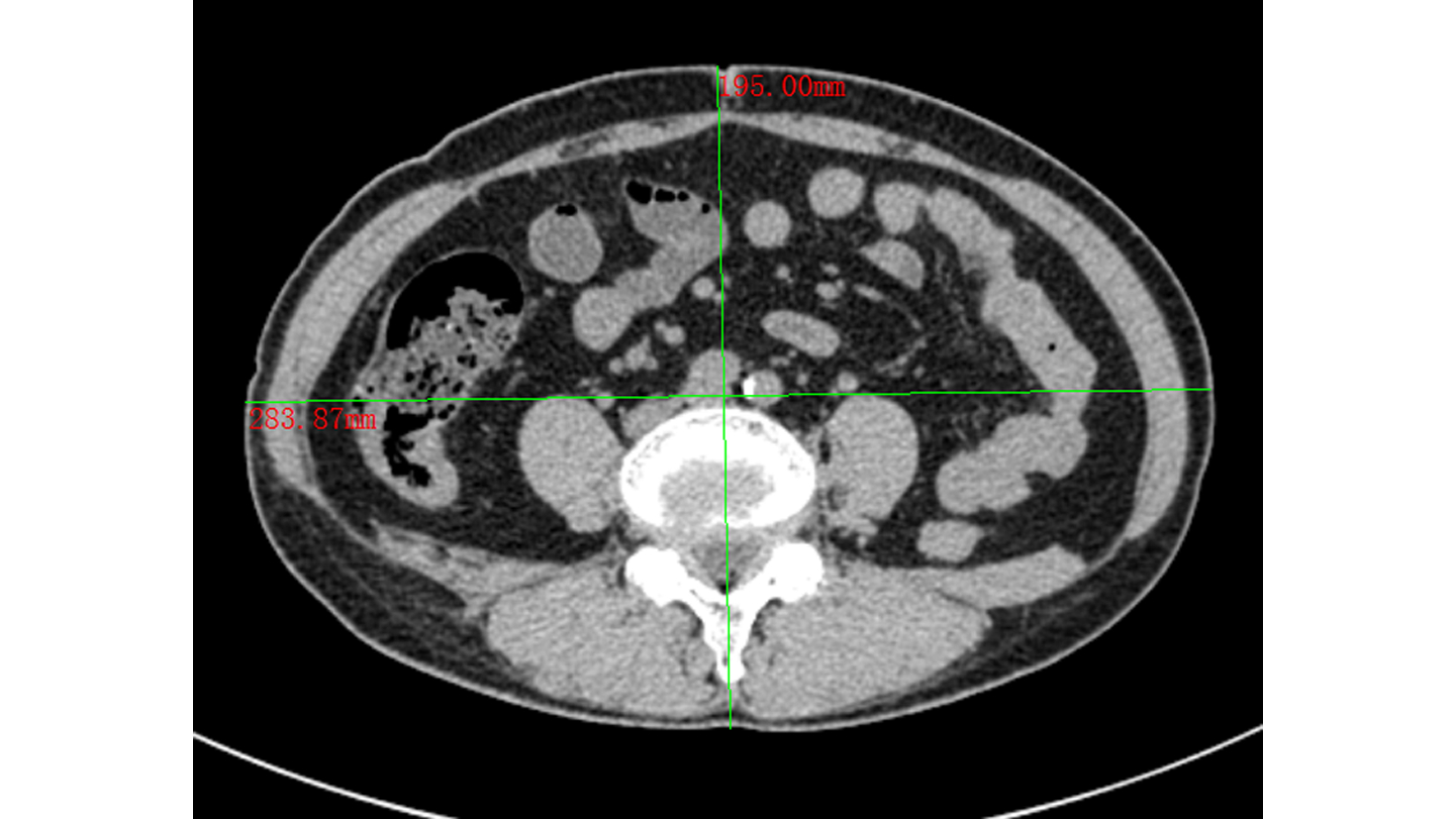
BORKAN GA, GERZOF SG, ROBBINS AH, et al. Assessment of abdominal fat content by computed tomography[J]. Am J Clin Nutr, 1982, 36(1): 172-177. DOI: 10.1093/ajcn/36.1.172. |
| [23] |
LEE SJ, JANSSEN I, HEYMSFIELD SB, et al. Relation between whole-body and regional measures of human skeletal muscle[J]. Am J Clin Nutr, 2004, 80(5): 1215-1221. DOI: 10.1093/ajcn/80.5.1215. |
| [24] |
MADICO C, HERPE G, VESSELLE G, et al. Intra peritoneal abdominal fat area measured from computed tomography is an independent factor of severe acute pancreatitis[J]. Diagn Interv Imaging, 2019, 100(7-8): 421-426. DOI: 10.1016/j.diii.2019.03.008. |
| [25] |
DUARTE-ROJO A, SOSA-LOZANO LA, SAU'L A, et al. Methods for measuring abdominal obesity in the prediction of severe acute pancreatitis, and their correlation with abdominal fat areas assessed by computed tomography[J]. Aliment Pharmacol Ther, 2010, 32(2): 244-253. DOI: 10.1111/j.1365-2036.2010.04321.x. |
| [26] |
AMATO MC, GIORDANO C, GALIA M, et al. Visceral adiposity index: a reliable indicator of visceral fat function associated with cardiometabolic risk[J]. Diabetes Care, 2010, 33(4): 920-922. DOI: 10.2337/dc09-1825. |
| [27] |
KAHN HS. The "lipid accumulation product" performs better than the body mass index for recognizing cardiovascular risk: a population-based comparison[J]. BMC Cardiovasc Disord, 2005, 5: 26. DOI: 10.1186/1471-2261-5-26. |
| [28] |
LEMIEUX I, PASCOT A, COUILLARD C, et al. Hypertriglyceridemic waist: A marker of the atherogenic metabolic triad (hyperinsulinemia; hyperapolipoprotein B; small, dense LDL) in men?[J]. Circulation, 2000, 102(2): 179-184. DOI: 10.1161/01.cir.102.2.179. |
| [29] |
XIA MF, CHEN Y, LIN HD, et al. A indicator of visceral adipose dysfunction to evaluate metabolic health in adult Chinese[J]. Sci Rep, 2016, 6: 38214. DOI: 10.1038/srep38214. |
| [30] |
XIA W, YU H, HUANG Y, et al. The visceral adiposity index predicts the severity of hyperlipidaemic acute pancreatitis[J]. Intern Emerg Med, 2022, 17(2): 417-422. DOI: 10.1007/s11739-021-02819-4. |
| [31] |
DING Y, ZHANG M, WANG L, et al. Association of the hypertriglyceridemic waist phenotype and severity of acute pancreatitis[J]. Lipids Health Dis, 2019, 18(1): 93. DOI: 10.1186/s12944-019-1019-2. |
| [32] |
BEYDOGAN E, GULLE S, GEZER C, et al. Effect of abdominal fat distribution on severity of acute pancreatitis[J]. Clin Exp Hepatol, 2021, 7(3): 264-269. DOI: 10.5114/ceh.2021.109345 |






 DownLoad:
DownLoad:
