| [1] |
ESLAM M, SANYAL AJ, GEORGE J, et al. MAFLD: A consensus-driven proposed nomenclature for metabolic associated fatty liver disease[J]. Gastroenterology, 2020, 158(7): 1999-2014. e1. DOI: 10.1053/j.gastro.2019.11.312. |
| [2] |
FOUAD Y, WAKED I, BOLLIPO S, et al. What's in a name? Renaming 'NAFLD' to 'MAFLD'[J]. Liver Int, 2020, 40(6): 1254-1261. DOI: 10.1111/liv.14478. |
| [3] |
ZHANG HJ, WANG YY, CHEN C, et al. Cardiovascular and renal burdens of metabolic associated fatty liver disease from serial US national surveys, 1999-2016[J]. Chin Med J (Engl), 2021, 134(13): 1593-1601. DOI: 10.1097/CM9.0000000000001513. |
| [4] |
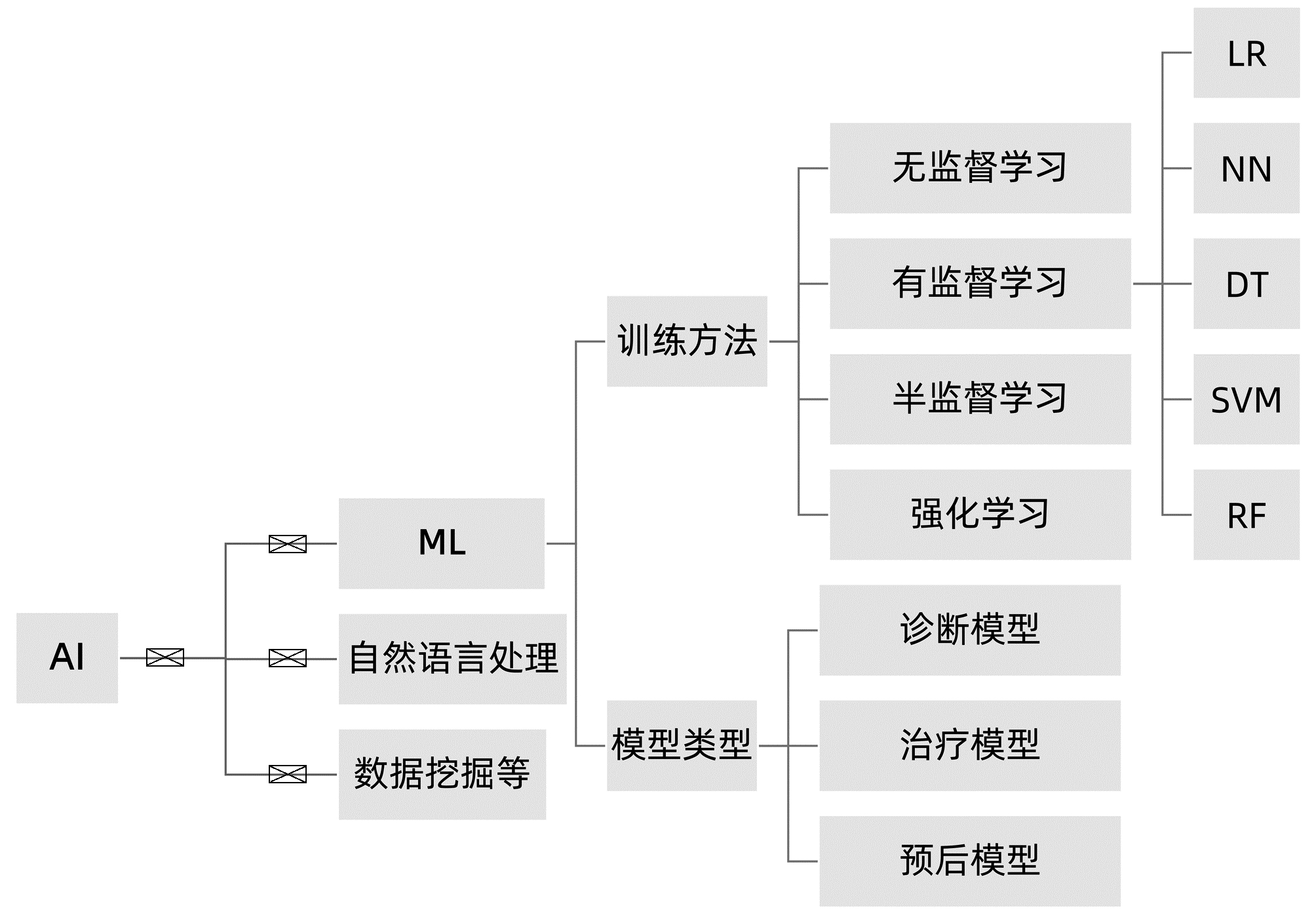
BADILLO S, BANFAI B, BIRZELE F, et al. An introduction to machine learning[J]. Clin Pharmacol Ther, 2020, 107(4): 871-885. DOI: 10.1002/cpt.1796. |
| [5] |
SU TH, WU CH, KAO JH. Artificial intelligence in precision medicine in hepatology[J]. J Gastroenterol Hepatol, 2021, 36(3): 569-580. DOI: 10.1111/jgh.15415. |
| [6] |
AHN JC, CONNELL A, SIMONETTO DA, et al. Application of artificial intelligence for the diagnosis and treatment of liver diseases[J]. Hepatology, 2020, 73(6): 2546-2563. DOI: 10.1002/hep.31603. |
| [7] |
CAO W, AN X, CONG L, et al. Application of deep learning in quantitative analysis of 2-dimensional ultrasound imaging of nonalcoholic fatty liver disease[J]. J Ultrasound Med, 2020, 39(1): 51-59. DOI: 10.1002/jum.15070. |
| [8] |
PERAKAKIS N, POLYZOS SA, YAZDANI A, et al. Non-invasive diagnosis of non-alcoholic steatohepatitis and fibrosis with the use of omics and supervised learning: A proof of concept study[J]. Metabolism, 2019, 101: 154005. DOI: 10.1016/j.metabol.2019.154005. |
| [9] |
GARCIA-CARRETERO R, VIGIL-MEDINA L, BARQUERO-PEREZ O, et al. Relevant features in nonalcoholic steatohepatitis determined using machine learning for feature selection[J]. Metab Syndr Relat Disord, 2019, 17(9): 444-451. DOI: 10.1089/met.2019.0052. |
| [10] |
GAWRIEH S, SETHUNATH D, CUMMINGS OW, et al. Automated quantification and architectural pattern detection of hepatic fibrosis in NAFLD[J]. Ann Diagn Pathol, 2020, 47: 151518. DOI: 10.1016/j.anndiagpath.2020.151518. |
| [11] |
HWANG A, SHI C, ZHU E, et al. Supervised learning reveals circulating biomarker levels diagnostic of hepatocellular carcinoma in a clinically relevant model of non-alcoholic steatohepatitis; An OAD to NASH[J]. PLoS One, 2018, 13(6): e0198937. DOI: 10.1371/journal.pone.0198937. |
| [12] |
RAMOT Y, ZANDANI G, MADAR Z, et al. Utilization of a deep learning algorithm for microscope-based fatty vacuole quantification in a fatty liver model in mice[J]. Toxicol Pathol, 2020, 48(5): 702-707. DOI: 10.1177/0192623320926478. |
| [13] |
FORLANO R, MULLISH BH, GIANNAKEAS N, et al. High-throughput, machine learning-based quantification of steatosis, inflammation, ballooning, and fibrosis in biopsies from patients with nonalcoholic fatty liver disease[J]. Clin Gastroenterol Hepatol, 2020, 18(9): 2081-2090. e9. DOI: 10.1016/j.cgh.2019.12.025. |
| [14] |
DEO RC. Machine learning in medicine[J]. Circulation, 2015, 132(20): 1920-1930. DOI: 10. M16/circuslationaha. 115. 001593.
|
| [15] |
KAVAKIOTIS I, TSAVE O, SALIFOGLOU A, et al. Machine learning and data mining methods in diabetes research[J]. Comput Struct Biotechnol J, 2017, 15: 104-116. DOI: 10.1016/j.csbj.2016.12.005. |
| [16] |
DINANI AM, KOWDLEY KV, NOUREDDIN M. Application of artificial intelligence for diagnosis and risk stratification in NAFLD and NASH: The state of the art[J]. Hepatology, 2021, 74(4): 2233-2240. DOI: 10.1002/hep.31869. |
| [17] |
van VLECK TT, CHAN L, COCA SG, et al. Augmented intelligence with natural language processing applied to electronic health records for identifying patients with non-alcoholic fatty liver disease at risk for disease progression[J]. Int J Med Inform, 2019, 129: 334-341. DOI: 10.1016/j.ijmedinf.2019.06.028. |
| [18] |
WANG K, LU X, ZHOU H, et al. Deep learning radiomics of shear wave elastography significantly improved diagnostic performance for assessing liver fibrosis in chronic hepatitis B: a prospective multicentre study[J]. Gut, 2019, 68(4): 729-741. DOI: 10.1136/gutjnl-2018-316204. |
| [19] |
TANG A, DESTREMPES F, KAZEMIRAD S, et al. Quantitative ultrasound and machine learning for assessment of steatohepatitis in a rat model[J]. Eur Radiol, 2019, 29(5): 2175-2184. DOI: 10.1007/s00330-018-5915-z. |
| [20] |
WU CC, YEH WC, HSU WD, et al. Prediction of fatty liver disease using machine learning algorithms[J]. Comput Methods Programs Biomed, 2019, 170: 23-29. DOI: 10.1016/j.cmpb.2018.12.032. |
| [21] |
HUO Y, TERRY JG, WANG J, et al. Fully automatic liver attenuation estimation combing CNN segmentation and morphological operations[J]. Med Phys, 2019, 46(8): 3508-3519. DOI: 10.1002/mp.13675. |
| [22] |
GRAFFY PM, SANDFORT V, SUMMERS RM, et al. Auto-mated liver fat quantification at nonenhanced abdominal CT for population-based steatosis assessment[J]. Radiology, 2019, 293(2): 334-342. DOI: 10. 1148/ radiol. 20191 90512.
|
| [23] |
FORLANO R, MULLISH BH, GIANNAKEAS N, et al. High-throughput, machine learning-based quantifica-tion of steatosis, inflammation, ballooning, and fibrosis in biopsies from patients with nonalcoholic fatty liver disease[J]. Clin Gastroen-terol Hepatol, 2020, 18(9): 2081-2090. DOI: 10. 1016/j. cgh. 2019. 12. 025.
|
| [24] |
QU H, MINACAPELLI CD, TAIT C, et al. Training of computational algorithms to predict NAFLD activity score and fibrosis stage from liver histopathology slides[J]. Comput Methods Programs Biomed, 2021, 207: 106153. DOI: 10.1016/j.cmpb.2021.106153. |
| [25] |
FENG G, ZHENG KI, LI YY, et al. Machine learning algorithm outperforms fibrosis markers in predicting significant fibrosis in biopsy-confirmed NAFLD[J]. J Hepatobiliary Pancreat Sci, 2021, 28(7): 593-603. DOI: 10.1002/jhbp.972. |
| [26] |
KOLECK TA, DREISBACH C, BOURNE PE, et al. Natural language processing of symptoms documented in free-text narratives of electronic health records: a systematic review[J]. J Am Med Inform Assoc, 2019, 26(4): 364-379. DOI: 10.1093/jamia/ocy173. |
| [27] |
VANDERBECK S, BOCKHORST J, KLEINER D, et al. Automatic quantification of lobular inflammation and hepatocyte ballooning in nonalcoholic fatty liver disease liver biopsies[J]. Hum Pathol, 2015, 46(5): 767-775. DOI: 10.1016/j.humpath.2015.01.019. |
| [28] |
VANDERBECK S, BOCKHORST J, KOMOROWSKI R, et al. Automatic classification of white regions in liver biopsies by supervised machine learning[J]. Hum Pathol, 2014, 45(4): 785-792. DOI: 10.1016/j.humpath.2013.11.011. |
| [29] |
YIP TC, MA AJ, WONG VW, et al. Laboratory parameter-based machine learning model for excluding non-alcoholic fatty liver disease (NAFLD) in the general population[J]. Aliment Pharmacol Ther, 2017, 46(4): 447-456. DOI: 10.1111/apt.14172. |
| [30] |
PERVEEN S, SHAHBAZ M, KESHAVJEE K, et al. A systematic machine learning based approach for the diagnosis of non-alcoholic fatty liver disease risk and progression[J]. Sci Rep, 2018, 8(1): 2112. DOI: 10.1038/s41598-018-20166-x. |
| [31] |
BERNÁ G, ROMERO-GOMEZ M. The role of nutrition in non-alcoholic fatty liver disease: Pathophysiology and management[J]. Liver Int, 2020, 40(Suppl 1): 102-108. DOI: 10.1111/liv.14360. |
| [32] |
ZEEVI D, KOREM T, ZMORA N, et al. Personalized nutrition by prediction of glycemic responses[J]. Cell, 2015, 163(5): 1079-1094. DOI: 10.1016/j.cell.2015.11.001. |
| [33] |
CALZADILLA-BERTOT L, VILAR-GOMEZ E, WONG VW, et al. ABIDE: An accurate predictive model of liver decompensation in patients with nonalcoholic fatty liver-related cirrhosis[J]. Hepatology, 2021, 73(6): 2238-2250. DOI: 10.1002/hep.31576. |
| [34] |
|
| [35] |
BIANCO C, JAMIALAHMADI O, PELUSI S, et al. Non-invasive stratification of hepatocellular carcinoma risk in non-alcoholic fatty liver using polygenic risk scores[J]. J Hepatol, 2021, 74(4): 775-782. DOI: 10.1016/j.jhep.2020.11.024. |
| [36] |
YOUNES R, CAVIGLIA GP, GOVAERE O, et al. Long-term outcomes and predictive ability of non-invasive scoring systems in patients with non-alcoholic fatty liver disease[J]. J Hepatol, 2021, 75(4): 786-794. DOI: 10.1016/j.jhep.2021.05.008. |
| [37] |
PETTA S, SEBASTIANI G, BUGIANESI E, et al. Non-invasive prediction of esophageal varices by stiffness and platelet in non-alcoholic fatty liver disease cirrhosis[J]. J Hepatol, 2018, 69(4): 878-885. DOI: 10.1016/j.jhep.2018.05.019. |






 DownLoad:
DownLoad: