| [1] |
GOYAL S, SAKHUJA P. Autoimmune pancreatitis: Current perspectives[J]. Indian J Pathol Microbiol, 2021, 64(Supplement): S149-S159. DOI: 10.4103/ijpm.ijpm_59_21. |
| [2] |
SHIMOSEGAWA T, CHARI ST, FRULLONI L, et al. International consensus diagnostic criteria for autoimmune pancreatitis: Guidelines of the International Association of Pancreatology[J]. Pancreas, 2011, 40(3): 352-358. DOI: 10.1097/MPA.0b013e3182142fd2. |
| [3] |
PODDIGHE D. Autoimmune pancreatitis and pancreatic cancer: Epidemiological aspects and immunological considerations[J]. World J Gastroenterol, 2021, 27(25): 3825-3836. DOI: 10.3748/wjg.v27.i25.3825. |
| [4] |
HAGHBIN H, CHUANG J, FATIMA R, et al. Correlation of autoimmune pancreatitis and malignancy: Systematic review and Meta-analysis[J]. Dig Dis Sci, 2021. DOI: 10.1007/s10620-021-07179-9. |
| [5] |
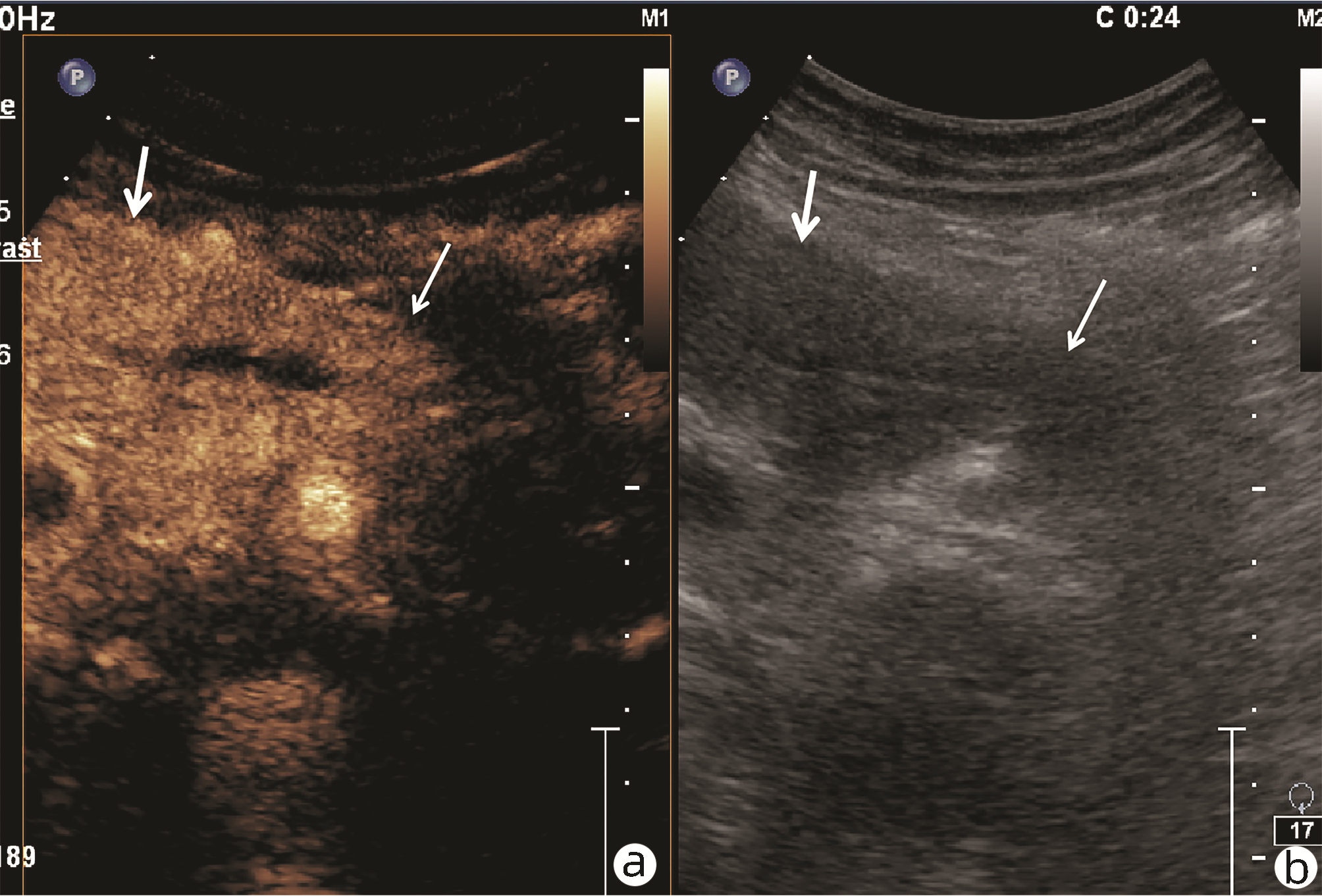
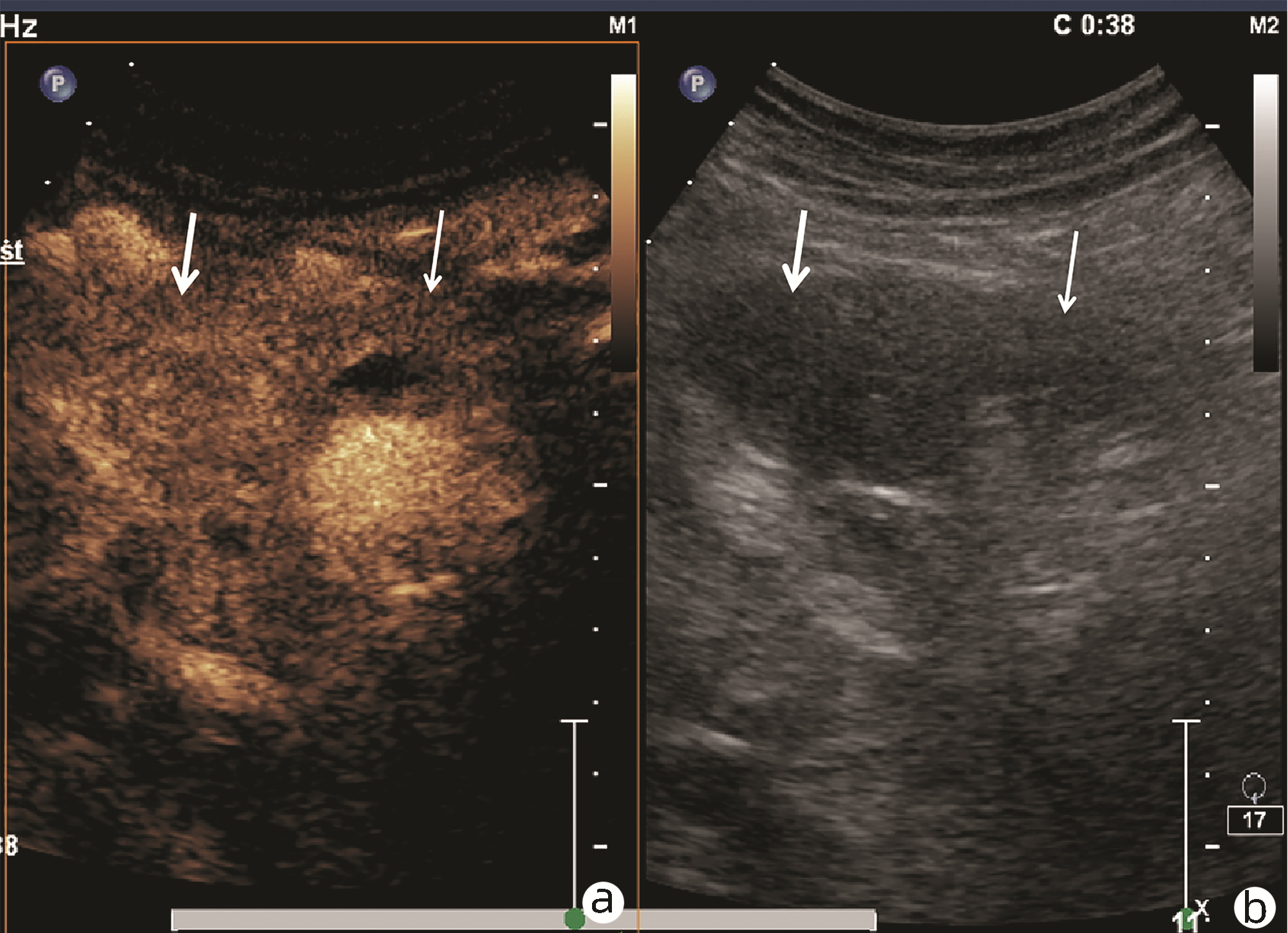
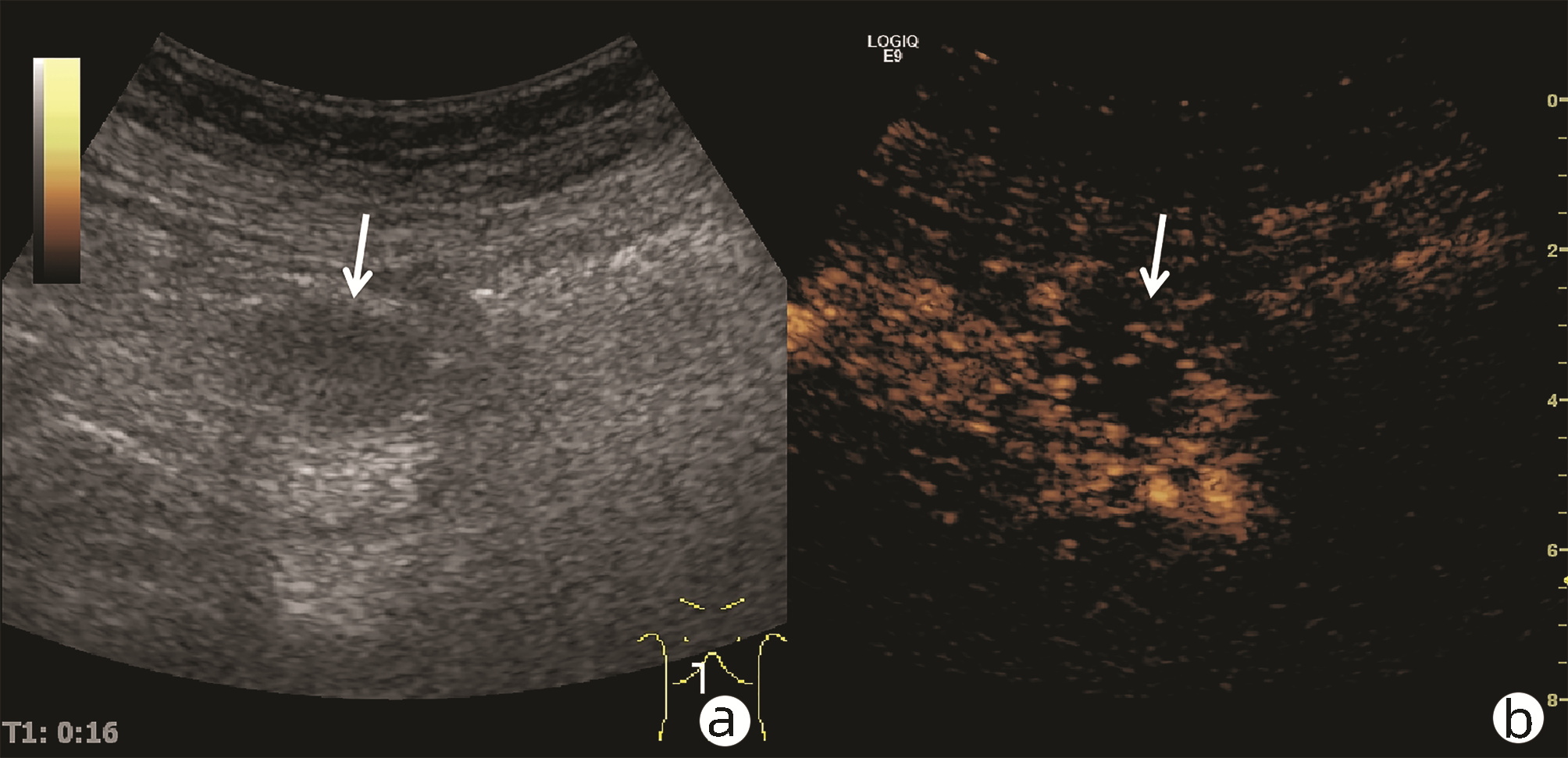
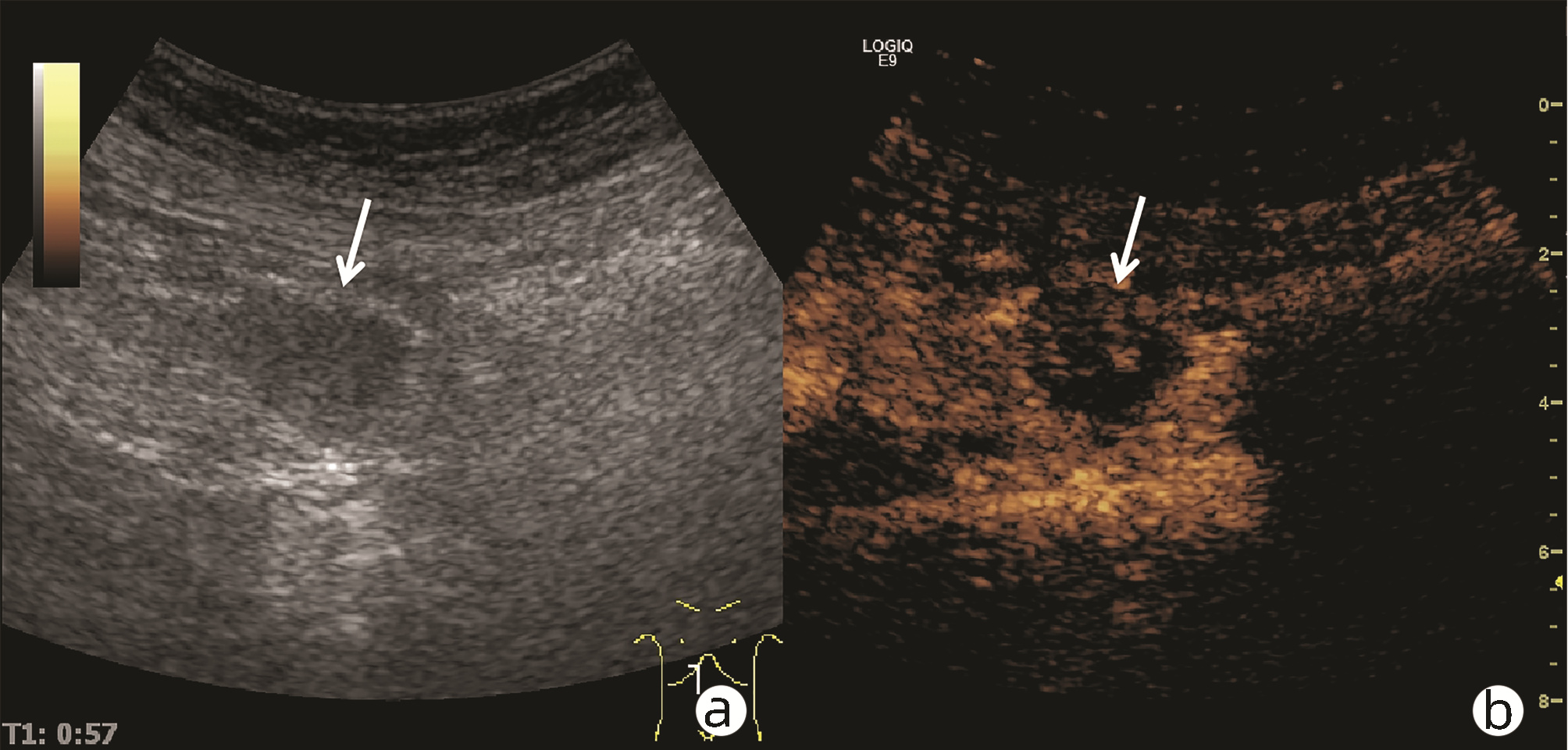
ZHANG Q, YANG DH, YU LY, et al. Clinical value of contrast-enhanced ultrasound in diagnosis of isolated autoimmune pancreatitis[J]. Chin J Ultrasound Med, 2019, 35(1): 35-38. DOI: 10.3969/j.issn.1002-0101.2019.01.013. |
| [6] |
NAITOH I, KAMISAWA T, TANAKA A, et al. Clinical characteristics of immunoglobulin IgG4-related sclerosing cholangitis: Comparison of cases with and without autoimmune pancreatitis in a large cohort[J]. Dig Liver Dis, 2021, 53(10): 1308-1314. DOI: 10.1016/j.dld.2021.02.009. |
| [7] |
CHEN ZK, ZHANG XJ, QIAN QF, et al. Ultrasonic features and diagnosis of autoimmune pancreatitis[J]. Chin J Med Imaging Technol, 2019, 35(2): 310-311. DOI: 10.13929/j.1003-3289.201807102. |
| [8] |
ZHANG XL, YANG PP, QIAN LX. Ultrasound manifestations and characteristics analysis of IgG4-related autoimmune pancreatitis[J]. J Clin Exp Med, 2019, 18(19): 2127-2129. DOI: 10.3969/j.issn.1671-4695.2019.19.034. |
| [9] |
MACINGA P, BAJER L, DEL CHIARO M, et al. Pancreatic cancer in patients with autoimmune pancreatitis: A scoping review[J]. Pancreatology, 2021, 21(5): 928-937. DOI: 10.1016/j.pan.2021.03.007. |
| [10] |
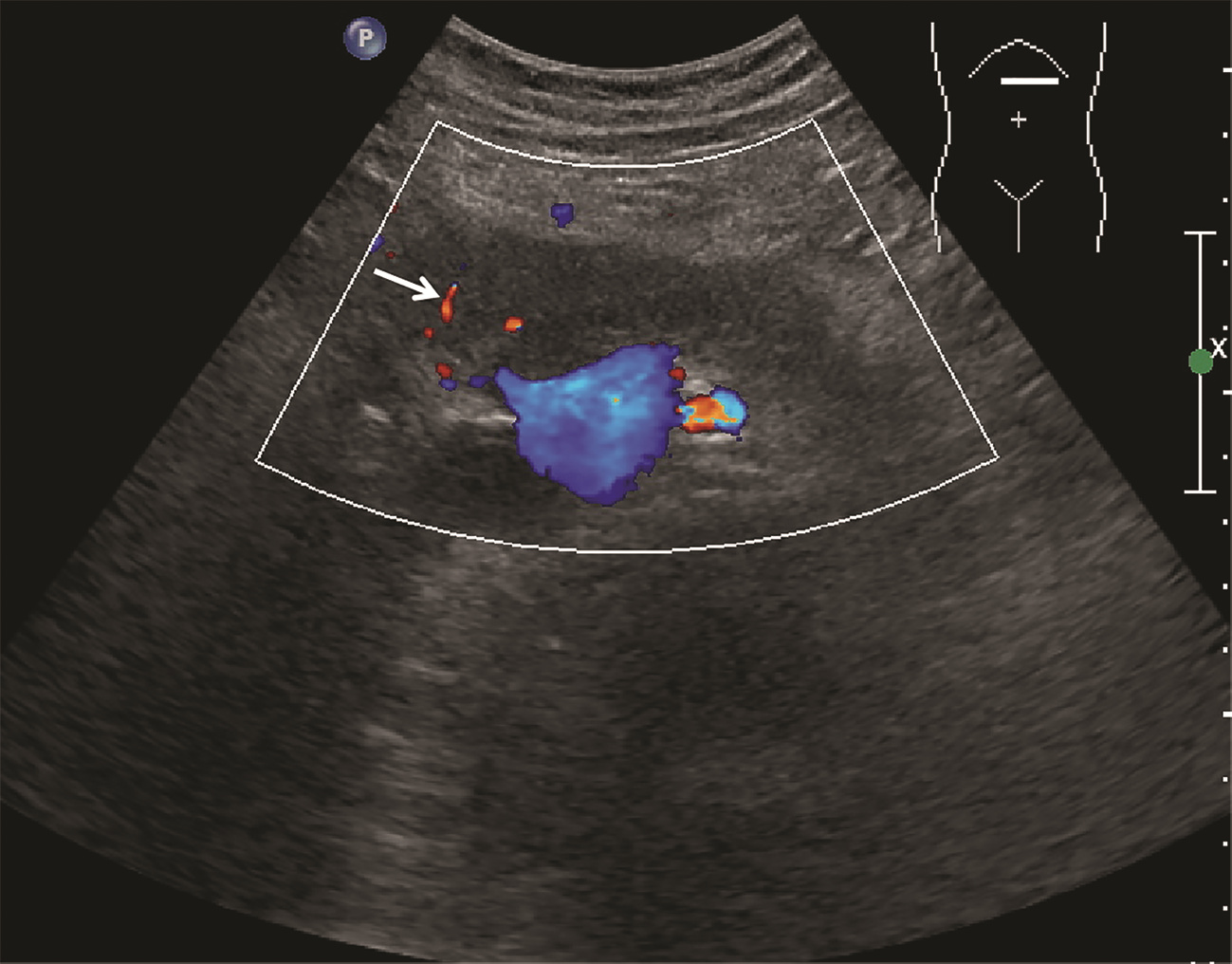
ZHOU CX, ZHU XH, HUANG Y, et al. Value of contrast-enhance ultrasound and color doppler ultrasonography in the diagnosis of pancreatic tumors[J]. Pract J Cancer, 2017, 32(5): 841-843. DOI: 10.3969/j.issn.1001-5930.2017.05.045. |
| [11] |
HAN YC. Comparison of ultrasonography characteristics and clinical manifestations between autoimmune pancreatitis and pancreatic cancer[J]. Clin Res Pract, 2019, 4(8): 98-99. DOI: 10.19347/j.cnki.2096-1413.201908038. |
| [12] |
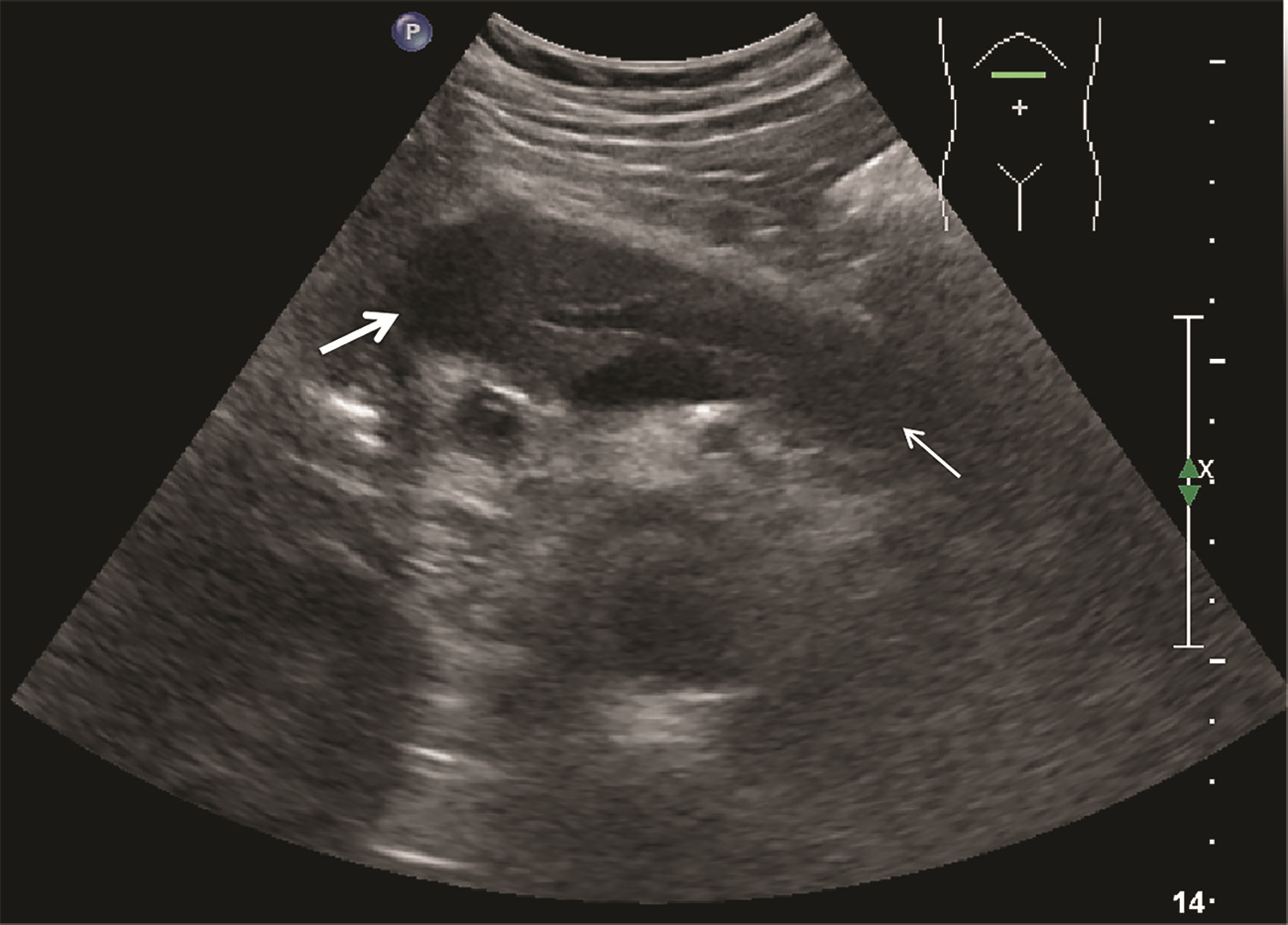
CONTI CB, CEREATTI F, DRAGO A, et al. Focal autoimmune pancreatitis: A simple flow chart for a challenging diagnosis[J]. Ultrasound Int Open, 2020, 6(3): E67-E75. DOI: 10.1055/a-1323-4906. |
| [13] |
GAO F, DU LF. The review of ultrasound mediated micrbubble for pancreatic cancer diagnosis and treatment[J]. Chin J Ultrasonogr, 2020, 29(10): 911-915. DOI: 10.3760/cma.j.cn131148-20200514-00397. |
| [14] |
|
| [15] |
|
| [16] |
XU XH, GUO WH, LI Y. Diagnostic value of EUS-EG combined with CEH-EUS in pancreatic space-occupying lesions[J]. Guangdong Med J, 2020, 41(20): 2146-2149. DOI: 10.13820/j.cnki.gdyx.20192312. |














 DownLoad:
DownLoad: