|
[1]LIU HL,WU XL,CAI GZ,et al.Minimally invasive treatment of small hepatocellular carcinoma in the deep portion of the liver complicated by portal hypertension:an analysis of 46cases[J].Clin J Curr Adv Gen Surg,2015,18(3):238-240.(in Chinese)刘洪亮,吴晓龙,蔡广臻,等.微创治疗肝脏深部微小肝癌合并门静脉高压46例分析[J].中国现代普通外科进展,2015,18(3):238-240.
|
|
[2]LI C,ZHANG QY,SUN KL,et al.Application of hepaticresection combined with selective decongestive devascularization of gastrosplenic region in hepatocellular carcinoma with moderate/severe portal hypertension[J].J Hepatopancreatobiliary Surg,2015,27(1):5-8.(in Chinese)李仓,张启瑜,孙克龙,等.肝癌切除联合选择性减断流术在原发性肝癌合并中重度门静脉高压症中的应用[J].肝胆胰外科杂志,2015,27(1):5-8.
|
|
[3]Chinese Society of Liver Cancer,Chinese Anti-Cancer Association;Liver Cancer Study Group,Chinese Society of Hepatology,Chinese Medical Association;Chinese Society of Pathology,Chinese Anti-Cancer Association,et al.Evidence-based practice guidelines for the standardized pathological diagnosis of primary liver cancer in China(2015 update)[J].J Clin Hepatol,2015,31(6):833-839.(in Chinese)中国抗癌协会肝癌专业委员会,中华医学会肝病学分会肝癌学组,中国抗癌协会病理专业委员会,等.原发性肝癌规范化病理诊断指南(2015年版)[J].临床肝胆病杂志,2015,31(6):833-839.
|
|
[4]MEHTA G,GUSTOT T,MOOKERJEE RP,et al.Inflammation and portal hypertension-the undiscovered country[J].J Hepatol,2014,61(1):155-163.
|
|
[5]WU SS,LIU HY,CHEN QL,et al.Association between CD4+/CD8+ratio in peripheral blood before hepatectomy for liver cancer and patient prognosis[J].J Clin Hepatol,2015,31(12):2066-2069.(in Chinese)吴珊珊,刘鸿瑜,陈秋恋,等.肝癌切除术前外周血中CD4+/CD8+值与患者预后的相关性分析[J].临床肝胆病杂志,2015,31(12):2066-2069.
|
|
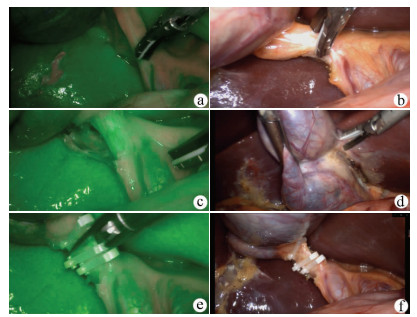
[6]JIN G,NING LJ,LI GW,et al.Analysis of short-term effects of three-dimensional conformal radiotherapy with chemoembolization for hepatic carcinoma[J].Trauma and Grit Medicine,2015,3(3):169-171.(in Chinese)金罡,宁路江,李光炜,等.化学治疗栓塞术联合三维适形放射治疗原发性肝癌60例近期疗效观察[J].创伤与急危重病医学,2015,3(3):169-171.
|
|
[7]HUANG DH,SHI JS,ZHANG CH.Usage analysis of human serum albumin in patients with liver cancer and liver cirrhosis after hepatectomy[J].J Clin Hepatol,2015,31(6):910-914.(in Chinese)黄东海,施建设,张诚华.原发性肝癌合并肝硬化患者肝切除术后人血白蛋白的应用分析[J].临床肝胆病杂志,2015,31(6):910-914.
|
|
[8]ZHANG GS,HUANG H,ZHUANG LY.Splenic artery ligation for treatment of portal hypertension of patients with hepatic carcinoma[J/CD].Chin J Oper Proc Gen Surg:Electronic Version,2015,8(1):35-38.(in Chinese)张国松,黄海,庄林渊.肝癌合并门静脉高压术中脾动脉结扎的临床疗效观察[J/CD].中华普外科手术学杂志:电子版,2015,8(1):35-38.
|
|
[9]LI W,WANG LZ,YANG XG,et al.Efficacy of transjugular intrahepatic portosystemic shunt with covered stents in the treatment of portal hypertension in 46 patients with primary hepatocellular carcinoma[J].Chin J Dig,2015,8(6):367-370.(in Chinese)李威,王黎洲,杨学刚,等.采用覆膜支架行经颈静脉肝内门体静脉分流术治疗原发性肝癌并门静脉高压46例疗效分析[J].中华消化杂志,2015,8(6):367-370.
|
|
[10]HUANG SZ,ZHOU Q.Research advances in primary hepatocellular carcinoma complicated by portal vein tumor thrombus[J].J Hepatobiliary Surg,2015,23(2):155-157.(in Chinese)黄陕州,周奇.原发性肝细胞癌合并门静脉癌栓研究进展[J].肝胆外科杂志,2015,23(2):155-157.
|
|
[11] GONG JB,MEI CQ,JIANG JX.Clinical efficacy of re-modified sugiura procedure for portal hypertention[J].Chin J Dig Surg,2016,15(7):674-679.(in Chinese)龚江波,梅长青,江建新.再改良的Sugiura术治疗门静脉高压症的临床疗效[J].中华消化外科杂志,2016,15(7):674-679.
|
|
[12]SHI G,LI JD,WANG XF,et al.Simultaneous hepatectomy and splenectomy for primary hepatocellular carcinoma accompanied with liver cirrhosis and hypersplenism[J].J North Sichuan Med Coll,2015,30(5):615-617.(in Chinese)石刚,李敬东,王小飞,等.联合肝脾切除在原发性肝癌合并肝硬化和脾功能亢进患者中的应用[J].川北医学院学报,2015,30(5):615-617.
|
|
[13]LIU LX,YIN DL.Prevention and management of operative complications after hepatectomy for liver cancer[J/CD].Chin J Oper Proc Gen Surg:Electronic Version,2014,8(1):23-25.(in Chinese)刘连新,尹大龙.肝癌肝切除术后常见并发症与处理[J/CD].中华普外科手术学杂志:电子版,2014,8(1):23-25.
|
|
[14]JIN H,ZHAO H,WANG B,et al.Clinical effect of selective hepatic inflow occlusion in left hemihepatectomy for primary liver cancer[J].Jiangsu Med J,2016,42(3):334-335.(in Chinese)金辉,赵华,王彬,等.选择性入肝血流阻断在原发性肝癌左半肝切除术中的临床效果[J].江苏医药,2016,42(3):334-335.
|
|
[15]CAO JL,LU SC,ZENG DB,et al.Clinical analysis of splenectomy and selective devascularization based on intra-operative free portal pressure[J].Chin J Hepatobiliary Surg,2014,20(9):648-651.(in Chinese)曹技磊,卢实春,曾道炳,等.基于术中自由门静脉压测定的脾切除加选择性断流术的临床分析[J].中华肝胆外科杂志,2014,20(9):648-651.
|
|
[16]XU JW,ZHANG YM,SONG Y,et al.Laparoscopic splenectomy and pericardial devascularization for portal hypertension[J].Chin J Min Inv Surg,2015,9(7):601-603.(in Chinese)徐继威,张耀明,宋越,等.完全腹腔镜下脾切除联合贲门周围血管离断术治疗门脉高压症[J].中国微创外科杂志,2015,9(7):601-603.
|
|
[17] HUANG J,LONG K,SON M.Clinical efficacy of laparoscopic splenectomy combined with pericardial devascularization[J].Chin J Dig Surg,2016,15(7):684-688.(in Chinese)黄洁,龙奎,孙敏.腹腔镜脾切除联合贲门周围血管离断术的临床疗效[J].中华消化外科杂志,2016,15(7):684-688.
|
|
[18]JIANG QF,WANG YX,LI K,et al.Laparoscopic splenectomy plus pericardial devascularization for portal hypertension[J].J Chin Practical Diagn Ther,2014,28(5):469-470.(in Chinese)姜青峰,王要轩,李珂,等.腹腔镜脾切除联合贲门周围血管离断术治疗门静脉高压症临床分析[J].中华实用诊断与治疗杂志,2014,28(5):469-470.
|
|
[19]WANG WJ,TANG Y,FENG XS,et al.Experience on application of modified laparoscopic splenectomy and devascularization for portal hypertension[J/CD].Chin J Laparoscopic Surgery:Electronic Edition,2015,8(2):12-17.(in Chinese)王文静,唐勇,冯贤松,等.改良腹腔镜脾切除及贲门周围血管离断术的应用体会[J/CD].中华腔镜外科杂志:电子版,2015,8(2):12-17.
|







 下载:
下载:

 本站查看
本站查看




 DownLoad:
DownLoad: