| [1] |
WANG CE, XU WT, GONG J, et al. Treatment of patients with nonalcoholic fatty liver disease[J]. Clin J Med Offic, 2022, 50( 9): 897- 899, 903. DOI: 10.16680/j.1671-3826.2022.09.06. |
| [2] |
FARRELL GC, WONG VW, CHITTURI S. NAFLD in Asia—as common and important as in the West[J]. Nat Rev Gastroenterol Hepatol, 2013, 10( 5): 307- 318. DOI: 10.1038/nrgastro.2013.34. |
| [3] |
MAK LY, SETO WK, HUI RW, et al. Fibrosis evolution in chronic hepatitis B e antigen-negative patients across a 10-year interval[J]. J Viral Hepat, 2019, 26( 7): 818- 827. DOI: 10.1111/jvh.13095. |
| [4] |
ESLAM M, SANYAL AJ, GEORGE J, et al. MAFLD: a consensus-driven proposed nomenclature for metabolic associated fatty liver disease[J]. Gastroenterology, 2020, 158( 7): 1999- 2014. DOI: 10.1053/j.gastro.2019.11.312. |
| [5] |
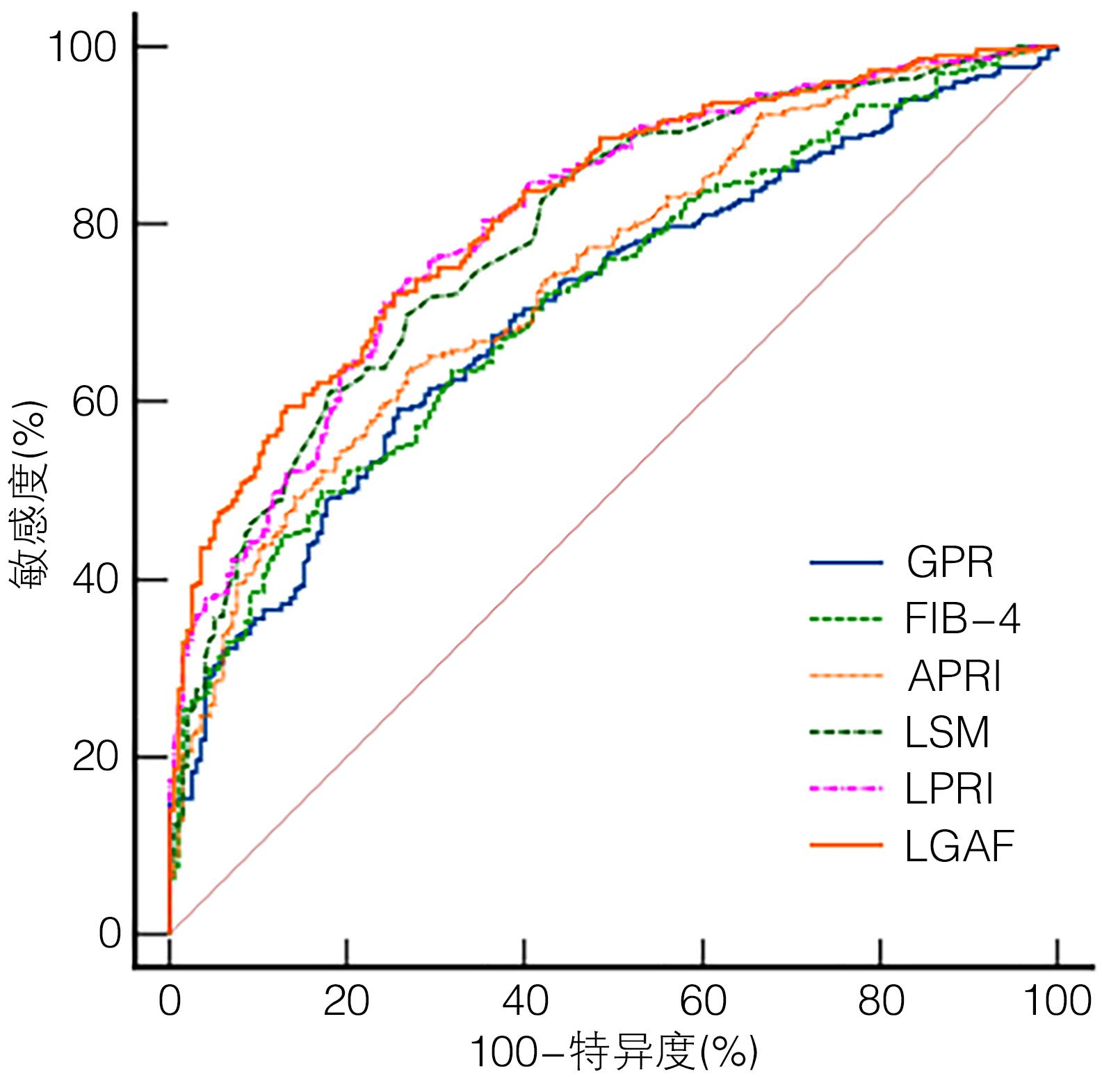
GONG H, LI LP. Value of Fibroscan combined with GPR, APRI, NFS or FIB-4 for progressive liver fibrosis in patients with chronic hepatitis B and nonalcoholic fatty liver disease[J]. J Clin Hepatol, 2020, 36( 3): 541- 545. DOI: 10.3969/j.issn.1001-5256.2020.03.014. |
| [6] |
WANG Q, XIE W, LIU L, et al. Serum markers for predicting advanced fibrosis in patients with chronic hepatitis B and nonalcoholic fatty liver disease[J]. Medicine(Baltimore), 2021, 100( 18): e25327. DOI: 10.1097/MD.0000000000025327. |
| [7] |
Foundation for Hepatitis Prevention and Control; Chinese Society of Infectious Disease and Chinese Society of Hepatology, Chinese Medical Association; Liver Disease Committee of Chinese Research Hospital Association. Consensus on clinical application of transient elastography detecting liver fibrosis: a 2018 update[J]. Chin J Hepatol, 2019, 27( 3): 182- 191. DOI: 10.3760/cma.j.issn.1007-3418.2019.03.004. |
| [8] |
CHENG DY, LI B, JI SB, et al. Application of transient elastography in noninvasive diagnosis of liver fibrosis[J/CD]. Chin J Liver Dis(Electronic Version), 2021, 13( 4): 9- 13. DOI: 10.3969/j.issn.1674-7380.2021.04.003. |
| [9] |
PARK JJ, PARK JY, KIM DY, et al. Prediction of significant fibrosis in chronic hepatitis C patients with normal ALT[J]. Hepatogastroenterology, 2011, 58( 109): 1321- 1327. DOI: 10.5754/hge11041. |
| [10] |
OKAJIMA A, SUMIDA Y, TAKETANI H, et al. Liver stiffness measurement to platelet ratio index predicts the stage of liver fibrosis in non-alcoholic fatty liver disease[J]. Hepatol Res, 2017, 47( 8): 721- 730. DOI: 10.1111/hepr.12793. |
| [11] |
Chinese Society of Infectious Diseases, Chinese Medical Association; Chinese Society of Hepatology, Chinese Medical Association. Guidelines for the prevention and treatment of chronic hepatitis B(version 2019)[J]. J Clin Hepatol, 2019, 35( 12): 2648- 2669. DOI: 10.3969/j.issn.1001-5256.2019.12.007. |
| [12] |
ESLAM M, SARIN SK, WONG VW, et al. The Asian Pacific Association for the Study of the Liver clinical practice guidelines for the diagnosis and management of metabolic associated fatty liver disease[J]. Hepatol Int, 2020, 14( 6): 889- 919. DOI: 10.1007/s12072-020-10094-2. |
| [13] |
GOODMAN ZD. Grading and staging systems for inflammation and fibrosis in chronic liver diseases[J]. J Hepatol, 2007, 47( 4): 598- 607. DOI: 10.1016/j.jhep.2007.07.006. |
| [14] |
Chinese Society of Hepatology, Chinese Medical Association; Chinese Society of Gastroenterology, Chinese Medical Association; Chinese Society of Infectious Diseases, Chinese Medical Association. Consensus on the diagnosis and therapy of hepatic fibrosis(2019)[J]. J Clin Hepatol, 2019, 35( 10): 2163- 2172. DOI: 10.3969/j.issn.1001-5256.2019.10.007. |
| [15] |
LEMOINE M, SHIMAKAWA Y, NAYAGAM S, et al. The gamma-glutamyl transpeptidase to platelet ratio(GPR) predicts significant liver fibrosis and cirrhosis in patients with chronic HBV infection in West Africa[J]. Gut, 2016, 65( 8): 1369- 1376. DOI: 10.1136/gutjnl-2015-309260. |
| [16] |
LIN S, HUANG J, WANG M, et al. Comparison of MAFLD and NAFLD diagnostic criteria in real world[J]. Liver Int, 2020, 40( 9): 2082- 2089. DOI: 10.1111/liv.14548. |
| [17] |
YAMAMURA S, ESLAM M, KAWAGUCHI T, et al. MAFLD identifies patients with significant hepatic fibrosis better than NAFLD[J]. Liver Int, 2020, 40( 12): 3018- 3030. DOI: 10.1111/liv.14675. |
| [18] |
van KLEEF LA, CHOI H, BROUWER WP, et al. Metabolic dysfunction-associated fatty liver disease increases risk of adverse outcomes in patients with chronic hepatitis B[J]. JHEP Rep, 2021, 3( 5): 100350. DOI: 10.1016/j.jhepr.2021.100350. |
| [19] |
RUGIVARODOM M, PONGPAIBUL A, CHAINUVATI S, et al. Prognostic relevance of metabolic dysfunction-associated steatohepatitis for patients with chronic hepatitis B[J]. J Clin Transl Hepatol, 2023, 11( 1): 76- 87. DOI: 10.14218/JCTH.2022.00055. |
| [20] |
DONG M, WU J, YU X, et al. Validation and comparison of seventeen noninvasive models for evaluating liver fibrosis in Chinese hepatitis B patients[J]. Liver Int, 2018, 38( 9): 1562- 1570. DOI: 10.1111/liv.13688. |
| [21] |
EDDOWES PJ, SASSO M, ALLISON M, et al. Accuracy of fibroscan controlled attenuation parameter and liver stiffness measurement in assessing steatosis and fibrosis in patients with nonalcoholic fatty liver disease[J]. Gastroenterology, 2019, 156( 6): 1717- 1730. DOI: 10.1053/j.gastro.2019.01.042. |
| [22] |
RIGOR J, DIEGUES A, PRESA J, et al. Noninvasive fibrosis tools in NAFLD: validation of APRI, BARD, FIB-4, NAFLD fibrosis score, and Hepamet fibrosis score in a Portuguese population[J]. Postgrad Med, 2022, 134( 4): 435- 440. DOI: 10.1080/00325481.2022.2058285. |
| [23] |
HUANG CM, HU ZW, NIE YQ, et al. The value of non-invasive diagnostic model in predicting liver fibrosis in patients with chronic hepatitis B combined with non-alcoholic fatty liver disease[J]. Chin J Gastroenter Hepatol, 2019, 28( 8): 915- 918. DOI: 10.3969/j.issn.1006-5709.2019.08.018. |
| [24] |
CHEN X, GOH GB, HUANG J, et al. Validation of non-invasive fibrosis scores for predicting advanced fibrosis in metabolic-associated fatty liver disease[J]. J Clin Transl Hepatol, 2022, 10( 4): 589- 594. DOI: 10.14218/JCTH.2021.00311. |
| [25] |
UCAR F, SEZER S, GINIS Z, et al. APRI, the FIB-4 score, and Forn's index have noninvasive diagnostic value for liver fibrosis in patients with chronic hepatitis B[J]. Eur J Gastroenterol Hepatol, 2013, 25( 9): 1076- 1081. DOI: 10.1097/MEG.0b013e32835fd699. |
| [26] |
XIAO G, YANG J, YAN L. Comparison of diagnostic accuracy of aspartate aminotransferase to platelet ratio index and fibrosis-4 index for detecting liver fibrosis in adult patients with chronic hepatitis B virus infection: a systemic review and meta-analysis[J]. Hepatology, 2015, 61( 1): 292- 302. DOI: 10.1002/hep.27382. |
| [27] |
ZHANG Z, WANG G, KANG K, et al. The diagnostic accuracy and clinical utility of three noninvasive models for predicting liver fibrosis in patients with HBV infection[J]. PLoS One, 2016, 11( 4): e0152757. DOI: 10.1371/journal.pone.0152757. |
| [28] |
LI Q, SONG J, HUANG Y, et al. The gamma-glutamyl-transpeptidase to platelet ratio does not show advantages than APRI and Fib-4 in diagnosing significant fibrosis and cirrhosis in patients with chronic hepatitis B: A retrospective cohort study in China[J]. Medicine(Baltimore), 2016, 95( 16): e3372. DOI: 10.1097/MD.0000000000003372. |
| [29] |
REN T, WANG H, WU R, et al. Gamma-glutamyl transpeptidase-to-platelet ratio predicts significant liver fibrosis of chronic hepatitis B patients in China[J]. Gastroenterol Res Pract, 2017, 2017: 7089702. DOI: 10.1155/2017/7089702. |
| [30] |
LUO J, DU Z, LIANG D, et al. Gamma-Glutamyl Transpeptidase-to-Platelet ratio predicts liver fibrosis in patients with concomitant chronic hepatitis B and nonalcoholic fatty liver disease[J]. J Clin Lab Anal, 2022, 36( 8): e24596. DOI: 10.1002/jcla.24596. |
| [31] |
HUANG CM, YANG Z, NIE YQ, et al. Prediction of liver fibrosis by gamma-glutamyl-transpeptidase-to-platelet ratio in patients with chronic hepatitis B viral infection with normal serum transaminase levels[J]. J Prac Hepatol, 2018, 21( 6): 859- 862. DOI: 10.3969/j.issn.1672-5069.2018.06.009. |
| [32] |
European Association for the Study of the Liver. EASL 2017 clinical practice guidelines on the management of hepatitis B virus infection[J]. J Hepatol, 2017, 67( 2): 370- 398. DOI: 10.1016/j.jhep.2017.03.021. |
| [33] |
Korean Association for the Study of the Liver(KASL). KASL clinical practice guidelines for management of chronic hepatitis B[J]. Clin Mol Hepatol, 2022, 28( 2): 276- 331. DOI: 10.3350/cmh.2022.0084. |
| [34] |
TERRAULT NA, LOK A, MCMAHON BJ, et al. Update on prevention, diagnosis, and treatment of chronic hepatitis B: AASLD 2018 hepatitis B guidance[J]. Hepatology, 2018, 67( 4): 1560- 1599. DOI: 10.1002/hep.29800. |
| [35] |
ZHANG GL, XU SC, ZENG J, et al. Optimizing the use of the gamma-glutamyl transpeptidase-to-platelet ratio and transient elastography to identify liver cirrhosis in patients with chronic hepatitis B concurrent with nonalcoholic fatty liver disease[J]. Dis Markers, 2019, 2019: 2585409. DOI: 10.1155/2019/2585409. |
| [36] |
LI Q, HUANG C, XU W, et al. Accuracy of FibroScan in analysis of liver fibrosis in patients with concomitant chronic hepatitis B and nonalcoholic fatty liver disease[J]. Medicine(Baltimore), 2020, 99( 23): e20616. DOI: 10.1097/MD.0000000000020616. |
| [37] |
ZHOU JL, WANG BQ, SUN YM, et al. Application value of liver stiffness measurement-to-platelet ratio index score in diagnosis of hepatitis B liver fibrosis and liver cirrhosis[J]. J Clin Hepatol, 2022, 38( 7): 1529- 1533. DOI: 10.3969/j. issn. 1001-5256.2022.07.014.
|













 DownLoad:
DownLoad: