| [1] |
Liver Failure and Artificial Liver Group, Chinese Society of Infectious Diseases, Chinese Medical Association; Severe Liver Disease and Artificial Liver Group. Guideline for diagnosis and treatment of liver failure(2018)[J]. J Clin Hepatol, 2019, 35( 1): 38- 44. DOI: 10.3969/j.issn.1001-5256.2019.01.007. |
| [2] |
ARROYO V, MOREAU R, JALAN R. Acute-on-chronic liver failure[J]. N Engl J Med, 2020, 382( 22): 2137- 2145. DOI: 10.1056/NEJMra1914900. |
| [3] |
HERNAEZ R, SOLÀ E, MOREAU R, et al. Acute-on-chronic liver failure: An update[J]. Gut, 2017, 66( 3): 541- 553. DOI: 10.1136/gutjnl-2016-312670. |
| [4] |
|
| [5] |
BI ZH, WANG LX, LIAN JQ. Definition, prognostic assessment, and advances in the diagnosis and treatment of acute-on-chronic liver failure[J]. J Clin Hepatol, 2022, 38( 7): 1671- 1676. DOI: 10.3969/j.issn.1001-5256.2022.07.041. |
| [6] |
ZACCHERINI G, WEISS E, MOREAU R. Acute-on-chronic liver failure: Definitions, pathophysiology and principles of treatment[J]. JHEP Rep, 2020, 3( 1): 100176. DOI: 10.1016/j.jhepr.2020.100176. |
| [7] |
KARVELLAS CJ, FRANCOZ C, WEISS E. Liver transplantation in acute-on-chronic liver failure[J]. Transplantation, 2021, 105( 7): 1471- 1481. DOI: 10.1097/TP.0000000000003550. |
| [8] |
KIM WR, MANNALITHARA A, HEIMBACH JK, et al. MELD 3.0: The model for end-stage liver disease updated for the modern era[J]. Gastroenterology, 2021, 161( 6): 1887- 1895. DOI: 10.1053/j.gastro.2021.08.050. |
| [9] |
KAMATH PS, KIM WR. The model for end-stage liver disease(MELD)[J]. Hepatology, 2007, 45( 3): 797- 805. DOI: 10.1002/hep.21563. |
| [10] |
KAMATH PS, WIESNER RH, MALINCHOC M, et al. A model to predict survival in patients with end-stage liver disease[J]. Hepatology, 2001, 33( 2): 464- 470. DOI: 10.1053/jhep.2001.22172. |
| [11] |
BIGGINS SW, KIM WR, TERRAULT NA, et al. Evidence-based incorporation of serum sodium concentration into MELD[J]. Gastroenterology, 2006, 130( 6): 1652- 1660. DOI: 10.1053/j.gastro.2006.02.010. |
| [12] |
MALINCHOC M, KAMATH PS, GORDON FD, et al. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts[J]. Hepatology, 2000, 31( 4): 864- 871. DOI: 10.1053/he.2000.5852. |
| [13] |
ABDALLAH MA, KUO YF, ASRANI S, et al. Validating a novel score based on interaction between ACLF grade and MELD score to predict waitlist mortality[J]. J Hepatol, 2021, 74( 6): 1355- 1361. DOI: 10.1016/j.jhep.2020.12.003. |
| [14] |
MEZZANO G, JUANOLA A, CARDENAS A, et al. Global burden of disease: Acute-on-chronic liver failure, a systematic review and meta-analysis[J]. Gut, 2022, 71( 1): 148- 155. DOI: 10.1136/gutjnl-2020-322161. |
| [15] |
GOUDSMIT BFJ, BRAAT AE, TUSHUIZEN ME, et al. Development and validation of a dynamic survival prediction model for patients with acute-on-chronic liver failure[J]. JHEP Rep, 2021, 3( 6): 100369. DOI: 10.1016/j.jhepr.2021.100369. |
| [16] |
HA JM, SOHN W, CHO JY, et al. Static and dynamic prognostic factors for hepatitis-B-related acute-on-chronic liver failure[J]. Clin Mol Hepatol, 2015, 21( 3): 232- 241. DOI: 10.3350/cmh.2015.21.3.232. |
| [17] |
CHEN MJ, LI X, TANG SH. Progress of multidimensional evaluation of liver function in prognosis of patients with liver failure[J]. Clin J Med Offic, 2023, 51( 9): 901- 903, 907. DOI: 10.16680/j.1671-3826.2023.09.05. |
| [18] |
GUSTOT T, FERNANDEZ J, GARCIA E, et al. Clinical Course of acute-on-chronic liver failure syndrome and effects on prognosis[J]. Hepatology, 2015, 62( 1): 243- 252. DOI: 10.1002/hep.27849. |
| [19] |
YU ZJ, ZHANG Y, CAO YY, et al. A dynamic prediction model for prognosis of acute-on-chronic liver failure based on the trend of clinical indicators[J]. Sci Rep, 2021, 11( 1): 1810. DOI: 10.1038/s41598-021-81431-0. |
| [20] |
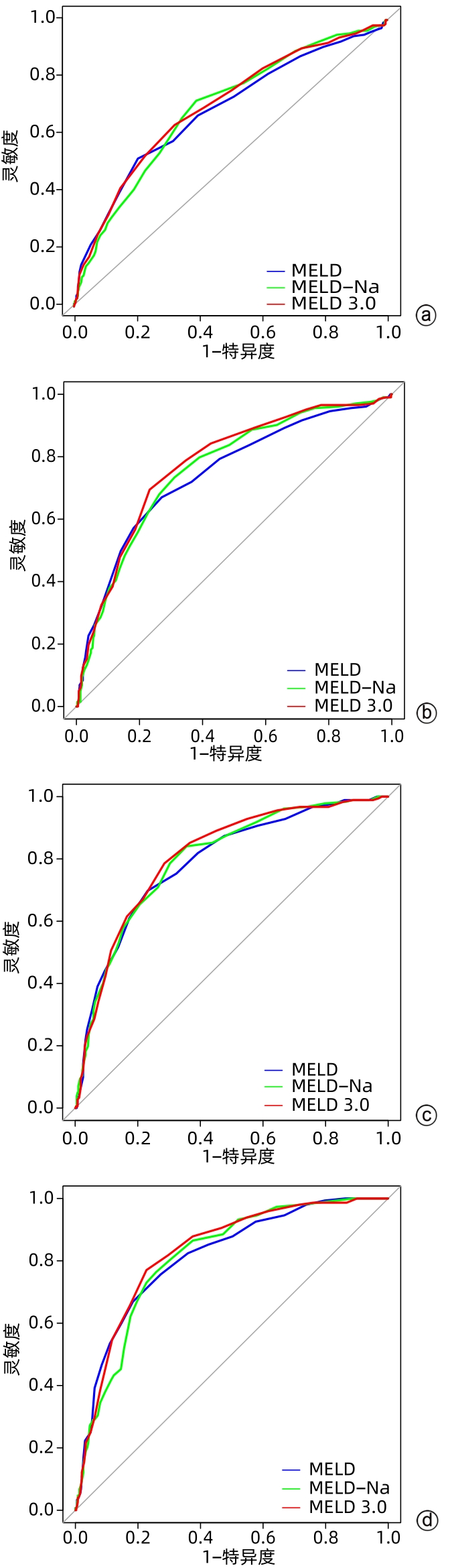
LIU WS, SHEN LJ, TIAN H, et al. ABC prognostic classification and MELD 3.0 and COSSH-ACLF II prognostic evaluation in acute-on-chronic liver failure[J]. Chin J Hepatol, 2022, 30( 9): 976- 980. DOI: 10.3760/cma.j.cn501113-20220308-00103. |








 本站查看
本站查看




 DownLoad:
DownLoad:
