| [1] |
Polaris Observatory Collaborators. Global prevalence, treatment, and prevention of hepatitis B virus infection in 2016: a modelling study[J]. Lancet Gastroenterol Hepatol, 2018, 3( 6): 383- 403. DOI: 10.1016/S2468-1253(18)30056-6. |
| [2] |
ZHOU WW, HUANG J, PAN FM. Research progress in epidemiological characteristics and therapeutic drugs of chronic hepatitis B[J]. J Changchun Univ Chin Med, 2022, 38( 12): 1420- 1424. DOI: 10.13463/j.cnki.cczyy.2022.12.028. |
| [3] |
RINELLA ME, NEUSCHWANDER-TETRI BA, SIDDIQUI MS, et al. AASLD Practice Guidance on the clinical assessment and management of nonalcoholic fatty liver disease[J]. Hepatology, 2023, 77( 5): 1797- 1835. DOI: 10.1097/HEP.0000000000000323. |
| [4] |
LEE YB, HA Y, CHON YE, et al. Association between hepatic steatosis and the development of hepatocellular carcinoma in patients with chronic hepatitis B[J]. Clin Mol Hepatol, 2019, 25( 1): 52- 64. DOI: 10.3350/cmh.2018.0040. |
| [5] |
SHIHA G, IBRAHIM A, HELMY A, et al. Asian-Pacific Association for the Study of the Liver(APASL) consensus guidelines on invasive and non-invasive assessment of hepatic fibrosis: a 2016 update[J]. Hepatol Int, 2017, 11( 1): 1- 30. DOI: 10.1007/s12072-016-9760-3. |
| [6] |
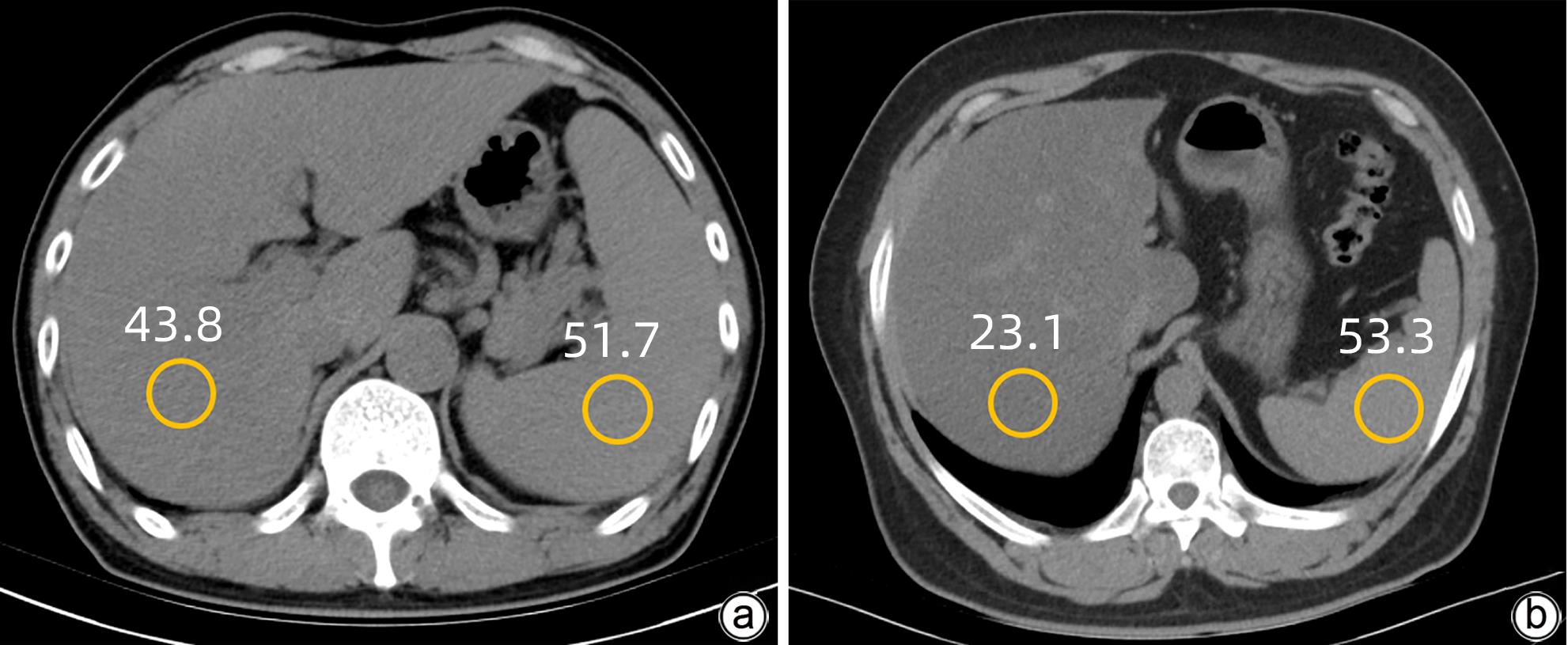
ROGIER J, ROULLET S, CORNÉLIS F, et al. Noninvasive assessment of macrovesicular liver steatosis in cadaveric donors based on computed tomography liver-to-spleen attenuation ratio[J]. Liver Transpl, 2015, 21( 5): 690- 695. DOI: 10.1002/lt.24105. |
| [7] |
FERRAIOLI G. Quantitative assessment of liver steatosis using ultrasound controlled attenuation parameter(Echosens)[J]. J Med Ultrason(2001), 2021, 48( 4): 489- 495. DOI: 10.1007/s10396-021-01106-1. |
| [8] |
Committee of Hepatology, Chinese Research Hospital Association, Fatty Liver Expert Committee, Chinese Medical Doctor Association, National Workshop on Fatty Liver and Alcoholic Liver Disease, Chinese Society of Hepatology, et al. Expert recommendations on standardized diagnosis and treatment for fatty liver disease(2019 revised edition)[J]. J Clin Hepatol, 2019, 35( 11): 2426- 2430. DOI: 10.3969/j.issn.1001-5256.2019.11.007. |
| [9] |
TAMAKI N, AJMERA V, LOOMBA R. Non-invasive methods for imaging hepatic steatosis and their clinical importance in NAFLD[J]. Nat Rev Endocrinol, 2022, 18( 1): 55- 66. DOI: 10.1038/s41574-021-00584-0. |
| [10] |
DULAI PS, SIRLIN CB, LOOMBA R. MRI and MRE for non-invasive quantitative assessment of hepatic steatosis and fibrosis in NAFLD and NASH: Clinical trials to clinical practice[J]. J Hepatol, 2016, 65( 5): 1006- 1016. DOI: 10.1016/j.jhep.2016.06.005. |
| [11] |
National Workshop on Fatty Liver and Alcoholic Liver Disease, Chinese Society of Hepatology, Chinese Medical Association, Fatty Liver Expert Committee, Chinese Medical Doctor Association. Guidelines of prevention and treatment for nonalcoholic fatty liver disease: A 2018 update[J]. J Clin Hepatol, 2018, 34( 5): 947- 957. DOI: 10.3969/j.issn.1001-5256.2018.05.007. |
| [12] |
YE J, WU Y, LI F, et al. Effect of orlistat on liver fat content in patients with nonalcoholic fatty liver disease with obesity: assessment using magnetic resonance imaging-derived proton density fat fraction[J]. Therap Adv Gastroenterol, 2019, 12: 1756284819879047. DOI: 10.1177/1756284819879047. |
| [13] |
YANG M, WEI L. Impact of NAFLD on the outcome of patients with chronic hepatitis B in Asia[J]. Liver Int, 2022, 42( 9): 1981- 1990. DOI: 10.1111/liv.15252. |
| [14] |
CASTERA L, FRIEDRICH-RUST M, LOOMBA R. Noninvasive assessment of liver disease in patients with nonalcoholic fatty liver disease[J]. Gastroenterology, 2019, 156( 5): 1264- 1281.e4. DOI: 10.1053/j.gastro.2018.12.036. |
| [15] |
PARK CC, NGUYEN P, HERNANDEZ C, et al. Magnetic resonance elastography vs transient elastography in detection of fibrosis and noninvasive measurement of steatosis in patients with biopsy-proven nonalcoholic fatty liver disease[J]. Gastroenterology, 2017, 152( 3): 598- 607.e2. DOI: 10.1053/j.gastro.2016.10.026. |
| [16] |
LEE SS, PARK SH. Radiologic evaluation of nonalcoholic fatty liver disease[J]. World J Gastroenterol, 2014, 20( 23): 7392- 7402. DOI: 10.3748/wjg.v20.i23.7392. |
| [17] |
ZHONG L, CHEN JJ, CHEN J, et al. Nonalcoholic fatty liver disease: quantitative assessment of liver fat content by computed tomography, magnetic resonance imaging and proton magnetic resonance spectroscopy[J]. J Dig Dis, 2009, 10( 4): 315- 320. DOI: 10.1111/j.1751-2980.2009.00402.x. |
| [18] |
CHEN S, HUANG ZH. Advances in quantitative imaging evaluation of non-alcoholic fatty liver disease[J]. J New Clin Medicine, 2018, 11( 12): 1283- 1286. DOI: 10.3969/j.issn.1674-3806.2018.12.32. |
| [19] |
KARLAS T, PETROFF D, SASSO M, et al. Individual patient data meta-analysis of controlled attenuation parameter(CAP) technology for assessing steatosis[J]. J Hepatol, 2017, 66( 5): 1022- 1030. DOI: 10.1016/j.jhep.2016.12.022. |
| [20] |
NOGAMI A, YONEDA M, IWAKI M, et al. Non-invasive imaging biomarkers for liver steatosis in non-alcoholic fatty liver disease: present and future[J]. Clin Mol Hepatol, 2023, 29( Suppl): S123- S135. DOI: 10.3350/cmh.2022.0357. |
| [21] |
MA YN, LIU JC. Research progress in the noninvasive quantitative diagnosis of hepatic steatosis using controlled attenuation parameters[J]. Chin J Gastroenterol Hepatol, 2020, 29( 11): 1309- 1312. DOI: 10.3969/j.issn.1006-5709.2020.11.023. |






 DownLoad:
DownLoad: