| [1] |
BRUIX J, REIG M, SHERMAN M. Evidence-based diagnosis, staging, and treatment of patients with hepatocellular carcinoma[J]. Gastroenterology, 2016, 150(4): 835-853. DOI: 10.1053/j.gastro.2015.12.041 |
| [2] |
TAN YH, SHANG YY, ZHANG T, et al. Current status and perspectives of multimodality therapy for hepatocellular carcinoma[J]. J Clin Hepatol, 2019, 35(8): 1858-1860. (in Chinese) DOI: 10.3969/j.issn.1001-5256.2019.08.047 |
| [3] |
KOOBY DA, STOCKMAN J, BEN-PORAT L, et al. Influence of transfusions on perioperative and long-term outcome in patients following hepatic resection for colorectal metastases[J]. Ann Surg, 2003, 237(6): 860-869; discussion 869-870.
|
| [4] |
TORZILLI G, MAKUUCHI M, INOUE K, et al. No-mortality liver resection for hepatocellular carcinoma in cirrhotic and noncirrhotic patients: Is there a way? A prospective analysis of our approach[J]. Arch Surg, 1999, 134(9): 984-992. DOI: 10.1001/archsurg.134.9.984 |
| [5] |
|
| [6] |
TORZILLI G, PROCOPIO F, DONADON M, et al. Safety of intermittent Pringle maneuver cumulative time exceeding 120 minutes in liver resection: A further step in favor of the "radical but conservative" policy[J]. Ann Surg, 2012, 255(2): 270-280. DOI: 10.1097/SLA.0b013e318232b375 |
| [7] |
GLANEMANN M, VOLLMAR B, NUSSLER AK, et al. Ischemic preconditioning protects from hepatic ischemia/reperfusion-injury by preservation of microcirculation and mitochondrial redox-state[J]. J Hepatol, 2003, 38(1): 59-66. DOI: 10.1016/S0168-8278(02)00327-6 |
| [8] |
KUPIEC-WEGLINSKI JW, BUSUTTIL RW. Ischemia and reperfusion injury in liver transplantation[J]. Transpl Proc, 2005, 37(4): 1653-1656. DOI: 10.1016/j.transproceed.2005.03.134 |
| [9] |
MAN K, FAN ST, NG IO, et al. Tolerance of the liver to intermittent pringle maneuver in hepatectomy for liver tumors[J]. Arch Surg, 1999, 134(5): 533-539. DOI: 10.1001/archsurg.134.5.533 |
| [10] |
WU CC, HWANG CR, LIU TJ, et al. Effects and limitations of prolonged intermittent ischaemia for hepatic resection of the cirrhotic liver[J]. Br J Surg, 1996, 83(1): 121-124. DOI: 10.1002/bjs.1800830139 |
| [11] |
BISMUTH H. Surgical anatomy and anatomical surgery of the liver[J]. World J Surg, 1982, 6(1): 3-9. DOI: 10.1007/BF01656368 |
| [12] |
CLAUDIO L, BRENDON S, MARCO S, et al. Assessing the quality of studies in meta-analyses: Advantage and limitations of the Newcastie Ottawa Scale[J]. WJMA, 2017, 5(4): 80. DOI: 10.13105/wjma.v5.i4.80 |
| [13] |
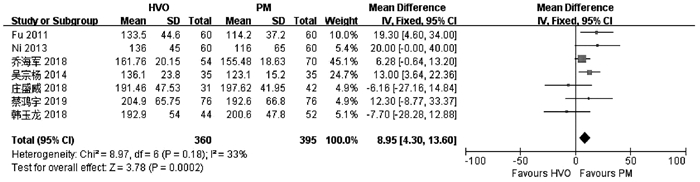
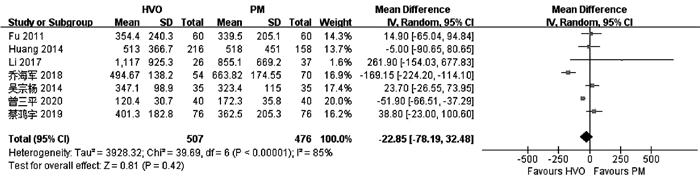
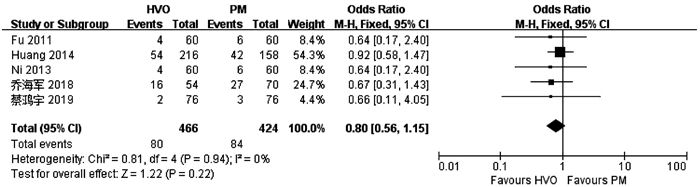
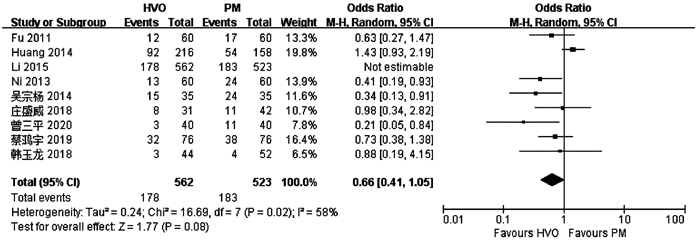
HUANG Z, ZHANG P, WANG H, et al. Comparing outcomes of two vascular inflow occlusion techniques and treatment without vascular occlusion during major hepatectomy in patients with hepatitis B-related hepatocellular carcinoma[J]. PLoS One, 2014, 9(9): e107303. DOI: 10.1371/journal.pone.0107303 |
| [14] |
LI M, ZHANG T, WANG L, et al. Selective hemihepatic vascular occlusion versus pringle maneuver in hepatectomy for primary liver cancer[J]. Med Sci Monit, 2017, 23: 2203-2210. DOI: 10.12659/MSM.900859 |
| [15] |
NI JS, LAU WY, YANG Y, et al. A prospective randomized controlled trial to compare pringle manoeuvre with hemi-hepatic vascular inflow occlusion in liver resection for hepatocellular carcinoma with cirrhosis[J]. J Gastrointest Surg, 2013, 17(8): 1414-1421. DOI: 10.1007/s11605-013-2236-z |
| [16] |
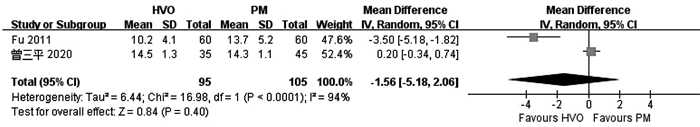
FU SY, LAU WY, LI GG, et al. A prospective randomized controlled trial to compare Pringle maneuver, hemihepatic vascular inflow occlusion, and main portal vein inflow occlusion in partial hepatectomy[J]. Am J Surg, 2011, 201(1): 62-69. DOI: 10.1016/j.amjsurg.2009.09.029 |
| [17] |
|
| [18] |
ZENG SP. Application effect comparison the first hepatic portal blood flow occlusion method and hemi-hepatic blood flow occlusion method in the treatment of primary hepatocellular carcinoma patients with hemi-hepatectomy[J]. Chin Mod Med, 2020, 27(3): 122-128. (in Chinese) DOI: 10.3969/j.issn.1674-4721.2020.03.036 |
| [19] |
HAN YL, MIAO J, YIN JJ. Comparison of different hepatic inflow occlusion in hepatectomy in treatm ent of patients with primary large liver cancer[J]. J Prac Hepatol, 2018, 21(1): 104-107. (in Chinese) DOI: 10.3969/j.issn.1672-5069.2018.01.025 |
| [20] |
|
| [21] |
|
| [22] |
|
| [23] |
ZHANG NP, ZHANG XJ. Evaluation of different hepatic blood flow blocking methods in laparoscopic hepatectomy of patients with liver cancer[J/CD]. Chin J Liver Dis (Electronic Version), 2019, 11(3): 58-63. (in Chinese)
张能平, 张雄杰. 不同肝血流阻断方式在肝癌患者腹腔镜肝切除术中的应用[J/CD]. 中国肝脏病杂志(电子版), 2019, 11(3): 58-63.
|
| [24] |
ZHU P, LAU WY, CHEN YF, et al. Randomized clinical trial comparing infrahepatic inferior vena cava clamping with low central venous pressure in complex liver resections involving the Pringle manoeuvre[J]. Br J Surg, 2012, 99(6): 781-788. DOI: 10.1002/bjs.8714 |
| [25] |
SELZNER N, RUDIGER H, GRAF R, et al. Protective strategies against ischemic injury of the liver[J]. Gastroenterology, 2003, 125(3): 917-936. DOI: 10.1016/S0016-5085(03)01048-5 |
| [26] |
|
| [27] |
XIAOBIN F, ZIPEI L, SHUGUO Z, et al. The Pringle manoeuvre should be avoided in hepatectomy for cancer patients due to its side effects on tumor recurrence and worse prognosis[J]. Med Hypotheses, 2009, 72(4): 398-401.
|
| [28] |
BELGHITI J, NOUN R, MALAFOSSE R, et al. Continuous versus intermittent portal triad clamping for liver resection: A controlled study[J]. Ann Surg, 1999, 229(3): 369-375.
|
| [29] |
GUO T, XIAO Y, LIU Z, et al. The impact of intraoperative vascular occlusion during liver surgery on postoperative peak ALT levels: A systematic review and meta-analysis[J]. Int J Surg, 2016, 27: 99-104.
|
| [30] |
WANG HQ, YANG JY, YAN LN. Hemihepatic versus total hepatic inflow occlusion during hepatectomy: A systematic review and meta-analysis[J]. World J Gastroenterol, 2011, 17(26): 3158-3164.
|
| [31] |
|
| [32] |
RAHBARI NN, KOCH M, MEHRABI A, et al. Portal triad clamping versus vascular exclusion for vascular control during hepatic resection: A systematic review and meta-analysis[J]. J Gastrointest Surg, 2009, 13(3): 558-568.
|







 下载:
下载:

 本站查看
本站查看





 DownLoad:
DownLoad: