| [1] |
Liver Failure and Artificial Liver Group, Chinese Society of Infectious Diseases, Chinese Medical Association; Severe Liver Disease and Artificial Liver Group, Chinese Society of Hepatology, Chinese Medical Association. Guideline for diagnosis and treatment of liver failure(2018)[J]. J Clin Hepatol, 2019, 35(1): 38-44. (in Chinese)
中华医学会感染病学分会肝衰竭与人工肝学组, 中华医学会肝脏病学分会重型肝病与人工肝学组. 肝衰竭诊治指南(2018年版)[J]. 临床肝胆病杂志, 2019, 35(1): 38-44.
|
| [2] |
ZHANG J, ZHOU XM. Value of different scoring systems in predicting short-term mortality of patients with acute-on-chronic liver failure[J]. J Clin Hepatol, 2019, 35(9): 1990-1994. (in Chinese) DOI: 10.3969/j.issn.1001-5256.2019.09.021 |
| [3] |
MEHTA G, MOOKERJEE RP, SHARMA V, et al. Systemic inflammation is associated with increased intrahepatic resistance and mortality in alcohol-related acute-on-chronic liver failure[J]. Liver Int, 2015, 35(3): 724-34. DOI: 10.1111/liv.12559 |
| [4] |
PAN C, GU Y, ZHANG W, et al. Dynamic changes of lipopolysaccharide levels in different phases of acute on chronic hepatitis B liver failure[J]. PLoS One, 2012, 7(11): e49460. DOI: 10.1371/journal.pone.0049460 |
| [5] |
FUJITA T, SOONTRAPA K, ITO Y, et al. Hepatic stellate cells relay inflammation signaling from sinusoids to parenchyma in mouse models of immune-mediated hepatitis[J]. Hepatology, 2016, 63(4): 1325-1339. DOI: 10.1002/hep.28112 |
| [6] |
LI J, ZHAO YR, TIAN Z. Roles of hepatic stellate cells in acute liver failure: From the perspective of inflammation and fibrosis[J]. World J Hepatol, 2019, 11(5): 412-420. DOI: 10.4254/wjh.v11.i5.412 |
| [7] |
JIN L, GAO H, WANG J, et al. Role and regulation of autophagy and apoptosis by nitric oxide in hepatic stellate cells during acute liver failure[J]. Liver Int, 2017, 37(11): 1651-1659. DOI: 10.1111/liv.13476 |
| [8] |
TIAN Z, CHEN Y, YAO N, et al. Role of mitophagy regulation by ROS in hepatic stellate cells during acute liver failure[J]. Am J Physiol Gastrointest Liver Physiol, 2018, 315(3): g374-g384. DOI: 10.1152/ajpgi.00032.2018 |
| [9] |
DAS J, GHOSH J, MANNA P, et al. Acetaminophen induced acute liver failure via oxidative stress and JNK activation: Protective role of taurine by the suppression of cytochrome P450 2E1[J]. Free Radic Res, 2010, 44(3): 340-55. DOI: 10.3109/10715760903513017 |
| [10] |
MONIAUX N, DARNAUD M, GARBIN K, et al. The reg3α (HIP/PAP) lectin suppresses extracellular oxidative stress in a murine model of acute liver failure[J]. PLoS One, 2015, 10(5): e0125584. DOI: 10.1371/journal.pone.0125584 |
| [11] |
KINUGASA H, WHELAN KA, TANAKA K, et al. Mitochondrial SOD2 regulates epithelial-mesenchymal transition and cell populations defined by differential CD44 expression[J]. Oncogene, 2015, 34(41): 5229-39. DOI: 10.1038/onc.2014.449 |
| [12] |
KIM SR, KIM DI, KIM SH, et al. NLRP3 inflammasome activation by mitochondrial ROS in bronchial epithelial cells is required for allergic inflammation[J]. Cell Death Dis, 2014, 5: e1498. DOI: 10.1038/cddis.2014.460 |
| [13] |
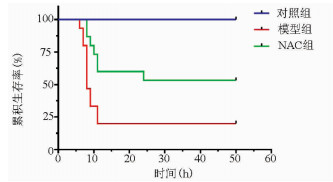
GAO YD, TIAN Y, ZHANG XY, et al. Effect of magnesium isoglycyrrhizinate on concanavalin A-induced acute liver failure in mice[J]. J Clin Hepatol, 2020, 36(7): 1571-1576. (in Chinese) DOI: 10.3969/j.issn.1001-5256.2020.07.024 |
| [14] |
EDWARDS S, LALOR PF, NASH GB, et al. Lymphocyte traffic through sinusoidal endothelial cells is regulated by hepatocytes[J]. Hepatology, 2005, 41(3): 451-459. DOI: 10.1002/hep.20585 |
| [15] |
BIEGHS V, VERHEYEN F, van GORP PJ, et al. Internalization of modified lipids by CD36 and SR-A leads to hepatic inflammation and lysosomal cholesterol storage in Kupffer cells[J]. PLoS One, 2012, 7(3): e34378. DOI: 10.1371/journal.pone.0034378 |
| [16] |
DECHÂNE A, SOWA JP, GIESELER RK, et al. Acute liver failure is associated with elevated liver stiffness and hepatic stellate cell activation[J]. Hepatology, 2010, 52(3): 1008-1016. DOI: 10.1002/hep.23754 |













 DownLoad:
DownLoad: